Total Body Cooling
advertisement

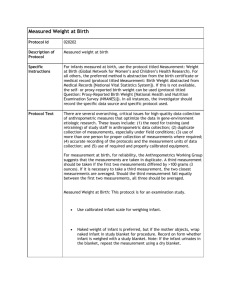
NS 1800.14 Therapeutic Measures NP 10/05 Parkland Health & Hospital System Women & Infant Specialty Health Nursery Services Procedure Manual Total Body Cooling for Infants with Hypoxic Ischemic Encephalopathy Practice Statement Upon the written order of the attending neonatologist or neonatal fellow the licensed nurse shall initiate, monitor and discontinue total body cooling therapy on infants with moderate to severe Hypoxic Ischemic Encephalopathy (HIE). Total body cooling should be started on qualifying infant’s before 6 hours of age. Purpose Total body cooling has been proven to decrease moderate and severe disability or death in infants born with moderate to severe asphyxia. Equipment Pre-printed provider orders: Phase 1 Initiation of Hypothermia # 6221 Phase 2 Rewarming of Hypothermia # 6222-A Phase 2 Rewarming Worksheet # 6222-B Blanketrol II Model 222R and Distilled Water Hose # 286 Rectal/Esophageal Sterile Disposable Probe Probe Adaptor Cable Maxi-Therm Lite Pediatric Blanket (single patient use) Maxi- Therm Lite Adult Blanket (single patient use) IV pole Procedure A. Eligibility Criteria 1. The attending or neonatal fellow shall evaluate all term infants ( 36 weeks gestation) admitted to the NICU with a diagnosis of neonatal depression, acute perinatal asphyxia or encephalopathy for total body cooling therapy. 2. Infants will be evaluated in two steps. Step A is an evaluation of clinical and biochemical criteria followed by Step B a neurologic exam to assess the stage of encephalopathy. Step A Evaluation of Clinical and Biochemical Criteria All infants will be evaluated for the following parameters: 1. History of an acute perinatal event: abruptio placenta, cord prolapse, severe FHR abnormality: variable or late decelerations 2. Apgar score 5 at 10 minutes. 3. Cord pH 7.0 or first postnatal blood gas pH 7.0 within 1 hour. 4. Base deficit on cord gas 16 mEq/L or first postnatal blood gas 16 mEq/L within 1 hour. 5. Continued need for ventilation initiated at birth and continued for at least 10 minutes. NS 1800.14 Therapeutic Measures NP 10/05 Page 2 of 5 3. Based upon the above criteria infant’s meeting specific parameters shall be catogorized as either A1 or A2. A1 are those infants that have either a: Cord pH ≤ 7.0 or first postnatal blood gas pH ≤ 7.0 within 1 hour OR Base deficit on cord gas ≥ 16 mEq/L or first postnatal blood gas ≥ 16 mEq/L within 1 hour. A2 are those infants with no blood gas or a blood gas with the pH between 7.0 and 7.15 and base deficit between 10-15.9 mEq/L that have had an acute perinatal event with either a: Apgar score ≤ 5 at 10 minutes OR Need for ventilation initiated at birth and continued for atleast 10 minutes. 4. The attending physician or designee will perform a neurologic exam for infants in A1 and A2 categories. The infant must show signs of moderate or severe HIE in at least 3 of the following 6 categories to be eligible for total body cooling. Infants who present with clinical seizures immediately qualify for total body cooling even if they do not meet step B criteria. Step B Neurological Exam CATEGORY SIGNS OF HIE Normal To Mild Moderate Severe 1. LEVEL OF CONSCIOUSNESS 1 2 = Lethargic 3 = Stupor/coma 2. SPONTANEOUS ACTIVITY 1 3 = No activity 3. POSTURE 1 2 = Decreased activity 2=Distal flexion, complete extension 2 = Hypotonia (focal or general) 4. TONE 1 3 = Decerebrate 3 = Flaccid 5. PRIMITIVE REFLEXES Suck Moro 6. AUTONOMIC SYSTEM 1 1 2 = Weak 2 = Incomplete 3 = Absent 3 = Absent Pupils 1 2 = Constricted Heart rate 1 2 = Bradycardia 3 = Deviation/dilated/ non-reactive to light 3 = Variable HR Respiration 1 2 = Periodic breathing 3 = Apnea NS 1800.14 Therapeutic Measures NP 10/05 Page 3 of 5 B. Cooling Procedures 1. Obtain pre-printed orders for Total Body Cooling. The attending physician or neonatal fellow shall sign the Pre-Printed Initiation Cooling order sheet. 2. Gather equipment to the bedside. 3. Pre-cool the blanketrol blanket: a. Attach the adult and pediatric hypothermia blankets to the hypothermia machine. b. Place the adult hypothermia blanket on an IV pole. c. Close the toggles on both the adult and pediatric blankets. d. Fill the cooling unit reservoir with 4 liters of Sterile Water. e. Plug in the system. f. POWER ON - status light will come on which says "Check Set Point". Make sure the temperatures are reading in the Celsius mode. The switch is on the front of the unit beside the "On/Off Switch". g. Push "TEMP SET" switch to pre-cool and lower temperature to 5°C by pushing the down arrow▼. (Do not go <5° or the blanket will alarm). h. OPEN the toggles on both of the cooling blankets. i. Press MANUAL CONTROL to start cooling blanket (the blanket's motor should come on). j. Let blanket cool. 3. Place the esophageal probe 2cm above the diaphragm: a. Determine esophageal temperature placement by measuring tip of nose to ear lobe and down to the xiphoid process, then minus 2 cm. Mark the distance on the tube with tape. b. Warm the esophageal probe in warm water, and lubricate the first 5-cm. c. Insert esophageal probe, preferably via the nares, and if not possible, then orally. d. Confirm placement with a CXR. 4. Place the infant on the pre-cooled blanket 25x33” and attach esophageal temperature probe to blanket. The blanket should be kept dry. The infant may be placed directly on the blanket or one thin sheet may be placed over the blanket, under the infant. 5. Place the IV pole with the adult blanket out of the way. Make sure none of the hoses are kinked. The large blanket on the IV pole is needed to minimize large fluctuations in the infant’s temperature. 6. Turn the infant’s radiant warmer to manual mode and decrease heat output to 0. There should be no external heat source. Maintain temperature probe so the skin temperature reading is on. 7. Press “TEMP SET” on the blanket and adjust the temperature to 33.5 oC with the ▲ arrow. NS 1800.14 Therapeutic Measures NP 10/05 Page 4 of 5 8. Press "AUTO CONTROL" (blanket's motor should go on and off with cooling). To be sure the unit is working properly, the wheel at the side of the unit will be turning. Goal temperature 33.5 degrees C with an acceptable temperature range of 32.5 – 34.5 º C. 9. Record esophageal and skin temperature every hour for 12 hours then every 2 hours. 10. Record heart rate and blood pressure at baseline, hourly for 12 hours, then every 2 hours. If infant requires inotropic support record blood pressure at baseline, the hourly while on inotropic support. Anticipate bradycardia. 11. Obtain blood gases at baseline, 4, 8, 12, 24,48, and 72 hours of age. infant’s temperature on blood gas slip. Record 12. Obtain serum electrolytes, BUN, and creatinine at baseline, 24, 48, and at 72 hours. 13. Check skin condition every 4 hours for areas of skin breakdown. Notify the provider of areas of redness. 14. Use pulse oximetry cautiously, if at all. Obtain provider order’s to discontinue pulse oximetry during hypothermia if not functioning properly. 15. Notify attending/neonatal fellow if temperature drops below 31 ºC. 16. A HUS shall be performed within 24 hours as clinically indicated. 17. The infant is to remain on the hypothermia blanket continuously for 72 hours. After 72 hours rewarming orders will be initiated. C. Re-warming Procedures 1. At the end of 72 hours obtain pre-printed provider order for rewarming. attending or neonatal fellow shall sign the order form. The 2. Obtain re-warming worksheet. Avoid rapid re-warming of the infant. 3. Press “TEMP SET” on the cooling unit. 4. Increase the temperature on the cooling unit by 0.5ºC every hour until the set point temperature on the cooling unit is on 36.5 º C. Record esophageal and skin temperature, heart rate, blood pressure and blanketrol readings hourly on the rewarming worksheet. 5. Once the set point on the cooling unit has been on 36.5 for one-hour switch the cooling unit to monitor only. NS 1800.14 Therapeutic Measures NP 10/05 Page 5 of 5 6. Switch the radiant warmer temperature mode from manual to servo and set the servo control temperature to 0.5ºC above infant’s skin temperature. 7. Increase the servo control temperature by 0.5ºC each hour until the servo control reading is set 36.5ºC. Record esophageal and skin temperature, heart rate and blood pressure readings hourly on the rewarming worksheet. 8. Once the infant’s skin temperature reaches 36.5ºC remove cooling blanket and esophageal probe. Dispose of pediatric and adult blankets. Place machine in dirty utility room for proper cleaning. 9. Obtain further vital sign per level of care and document on the NNICU flowsheet. 10. A MRI should be performed at discharged or at 44 weeks postconceptual age per standard of care.