Neonatal Respiratory Distress
advertisement

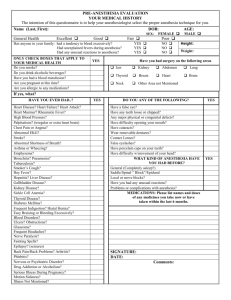
Cesarean Section Anesthesia and Neonatal Resuscitation David B. Brunson, DVM, MS, DACVA Small Animal Track 2012 ISVMA Annual Conference Proceedings Neonatal Resuscitation and Cesarean Section Anesthesia: Care of the newborn has dramatically changed in the past 30 years due to increased knowledge of birth and the availability of new drugs for pain management and anesthesia. Considerations for the timing of medications, delivery of the newborn and support for babies will change the way we care for these patients. “No more shaking the baby” By the end of gestation, many physiologic changes have occurred in the dam. Although these changes are considered "normal" they do affect our anesthetic management of the pregnant patient. In addition, anesthesia is complicated by the presence of two patients. Some common physiologic changes include: 1) Pulmonary function a. Increased alveolar ventilation b. Decreased functional residual capacity (FRC) and expiratory reserve volume (ERV). These changes explain in part the ease with which the pregnant patient can be anesthetized with inhalation anesthetics. However, MAC is reduced also during pregnancy possibly due to progesterone. 2) Dilutional anemia, although the red blood cell mass increases during pregnancy there is an even greater increase in plasma volume. For example, the packed cell volume of the pregnant bitch have been shown to decrease from a mean of 44.8% to 30.6%. 3) Increased cardiac output 4) Increased oxygen consumption Considerations for anesthesia of the pregnant patient. 1) Minimize stress of the dam 2) Avoid hypoxemia - pre-oxygenate the pregnant patient for 5 minutes prior to induction of anesthesia. An endotracheal tube is a requirement in any patient under general anesthesia. Mechanical ventilation should be available to avoid hypercarbia and respiratory acidosis during anesthesia. 3) Avoid hypotension - this means maintaining an adequate intravascular volume through administration of an isotonic, poly-ionic fluid such as lactated Ringer's solution. If fluid support does not overcome hypotension, then a vasopressor may be indicated. 4) Avoid hypothermia - anesthetic drugs tend to cause vasodilation that results in heat loss. Hypothermia slows drug metabolism, can lead to cardiac dysrrhythmia and increased hypotension, and can delay recovery. Circulating hot water pads are preferable to heating lamps or electric heating pads as there is less chance of thermal injury to the anesthetized patient. 5) Maintain as light a plane of anesthesia as possible; avoid drug overdosage. 6) Alpha-2 agonists - Xylazine (Rompun) at least in cattle, has been associated with spontaneous abortion in the third trimester of pregnancy. C-section Anesthetic Techniques Most drugs cross the placenta and affect the fetus. Glycopyrrolate and most neuromuscular blockers do not cross the placenta because of their large molecular size, high degree of ionization, and low lipid solubility. Furthermore, because of differences between maternal and fetal pH and the pka of drugs it is possible for drugs to become trapped and accumulate in the fetus, thus potentially causing depression of the neonate. Regional anesthesia +/- premedication The advantage with this technique is that there is minimal depression of the dam and neonate. However, half the body is anesthetized and the other half is not; the dam can be apprehensive, excited, uncomfortable, and uncooperative. Excessive movement is not uncommon. Regional anesthetic Techniques usually involve a line block or epidural, and Neuroleptanalgesia (sedation plus analgesics (opioids)), or dissociative (ketamine) anesthetics. Again, it is important to consider transplacental transfer of drugs, and to select drugs or dosages that minimize this effect. When sedatives are used there will be some neonatal depression, but there is usually better control of the dam. Inhalation Gas Anesthesia Usually involves some premedication of the dam with a light dose of a narcotic, tranquilizer, or sedative. Anesthesia is induced by mask using, high fresh gas flowrates. In small animals oxygen can be used to induce anesthesia with 3-4% halothane or isoflurane. Once anesthesia is achieved and stabilized the lowest possible concentration of primary anesthetic (halothane, isoflurane, or sevoflurane) is used which permits completion of the surgery. Inhalation anesthetics readily cross the placenta because of their high lipid solubility and relatively low molecular weights. Thus, it is not unusual to deliver a depressed neonate with this technique. The neonate can eliminate the anesthetic in the same fashion as the dam through the lungs. The key to successful recovery of the neonate is to be sure that it is breathing adequately, or else you must support ventilation-using techniques outlined in the following section on neonatal resuscitation. Short-acting injectable anesthetics Thiobarbiturates, propofol and diazepam/ketamine can be used for induction of general anesthesia. They should not be used for maintaining anesthesia. The initial drug will be rapidly redistributed to muscle. The drug concentration in the fetus, uterus and placenta will rapidly decrease minimizing CNS depression in the baby. Repeated doses will have the potential for prolonged depression. The surgeon should plan removal of the fetus at approximately 15 minutes after the start of anesthesia. Balanced anesthesia This involves "a little bit of this and a little of that". Basically, one tries to use small quantities of a variety of drugs to achieve immobility, analgesia and muscle relaxation in the dam, and minimal drug depression of the neonate. Intrauterine Physiology The fetal circulation effectively delivers blood high in oxygen and nutrients to the fetal heart and brain. The lungs that are unable to oxygenate the blood are perfused with only enough blood to meet the pulmonary tissue needs. At parturition this circulatory pattern must change if the neonate is to survive in the extra-uterine environment. The partial pressure of oxygen in fetal blood is lower than required by adult animals. The manner in which a fetal animal compensates for this relative hypoxic condition varies from species to species. In some species such as bovine, and primates this relative hypoxic condition is compensated for by a fetal hemoglobin that has an increased affinity for and an increased ability to release oxygen at the tissues. In the lungs the lower oxygen tensions cause a constriction of the vasculature. This vasoconstriction produces high pulmonary vascular resistance and prevents blood flow through the non-ventilated lungs. This phenomenon is called hypoxic vasoconstriction and remains as a characteristic of the pulmonary vasculature through adult life. Although the fetal lungs are not involved with the elimination of carbon dioxide and the absorption of oxygen, they serve several special functions. The lungs produce amniotic fluid to cushion the fetus. They act as an important reservoir of glycogen during late pregnancy. As the end of fetal development approaches the lungs begin to produce the surface-active substance that will be required to stabilize the air-inflated lungs. This substance is called surfactant and is an essential requirement for alveolar stability in the newly inflated lung, of the newborn. Near parturition the fetal lung becomes primed for the initiation of breathing. The muscles of respiration contract and relax as the functional development of the respiratory center reaches maturity. The ventilatory efforts are weak because of the mild stimuli that reach the neonate through the intrauterine environment. Another indication of fetal lung maturity is the lung size. The fetal lung becomes filled with surfactant-rich fluid to a volume comparable to the functional residual capacity of the inflated neonatal lungs. This ensures that the lungs will be of a size capable of sustaining the newborn immediately following birth. Parturition Induced Changes in the Neonate Tremendous changes occur in both the cardiovascular and pulmonary systems at the moment of birth. The events that occur are a carefully developed cascade of steps. Each event must occur in order to allow the next step to proceed. Many stimuli are present during birth that causes respiratory center stimulation. Tactile stimuli – compression and relaxation of the uterine muscles during the birthing process activate proprioceptive nerve pathways in the fetus. Umbilical blood flow may become reduced resulting in lower oxygen tension and higher carbon dioxide tension in the fetal blood. Central and peripheral chemoreceptors become activated with changes in the gas tension and blood pH resulting in secondary stimulation of the respiratory center of the brain. Ventilation is stimulated due to the change in temperature from the uterus to the outside world. The first breath marks the end of fetal life and the beginning of the neonatal period. The neonate must successfully inflate its lungs and begin effective ventilation soon after birth if it is to survive. In fact, the inflation of the lungs is the first and most important step of a cascade of events that must occur if the neonate is to survive. The effort necessary to initially inflate the fluid filled fetal lung requires negative intra-thoracic pressures in the range of -60 to minus -80 cm H20 are required. Once air is retained within the lung, and the fluid absorbed, the effort of breathing is reduced to the range of -8 to -12 cm H20 pressure. With air in the lung the pulmonary vascular resistance will rapidly decrease as the vessels dilate in response to the increased oxygen and the decreased carbon dioxide tensions. The reduction in pulmonary vascular resistance and the concomitant increase in pulmonary blood flow is the second step of the cascade. Vaso-active kinins are released from the aerated lung further cause the pulmonary vessels to dilate, and also cause constriction of the ductus arteriosus and umbilical vessels. As the resistance to blood flow into the lungs decreases right arterial pressure also decreases. Simultaneously, increased blood flow into the left atrium, and increased systemic vascular resistance due to constriction in the umbilical arteries, cause functional closure of the foramen ovale. At this point the newborn animal has switched from the fetal circulatory pattern to the independent pulmonary and cardiovascular systems of the adult. Neonatal Respiratory Distress Possible causes Dystocia due to any cause can cause the neonate to become severely hypoxic, acidotic, and weak. With severe hypoxia or acidosis the ability of the neonate to initiate ventilation diminishes until it is unable to generate the large negative pressures needed to displace the lung fluid. Weak neonates are often delivered following caesarian sections. This can be due to a prolonged and stressful labor prior to delivery, or pharmacologic depression of the neonate. In the human, respiratory distress syndrome of the newborn is associated with an immaturity of the lung and is most frequently a problem of premature infants. The immature infant lacks sufficient amounts of surfactant resulting in unstable alveoli. In order to sustain these, infants, they are intubated and maintained on mechanical ventilators until the lungs produce enough surfactant to remain inflated. Resuscitation Procedures for the Newborn DON’T SHAKE BABIES Be prepared Clip the dam as much as possible prior to induction of anesthesia. Have towels for drying the neonates, and a warm, draft-free area for keeping them until the surgery is finished. Have endotracheal tubes and drugs readily available for resuscitation. Have a plan of action. As soon as the fetus is delivered a series of evaluations need to be performed. If the neonate begins to fail in its conversion from a fetus to a neonate, resuscitation must be instituted immediately. After initially cleaning the face, nose, and oral pharynx of mucous and fetal membranes, the heart rate, mucous membrane color and respiratory efforts should be evaluated. The results of the initial evaluation will be quite variable depending on the vitality of the neonate but is important to establish the basis for future evaluations. Neonates with weak or slow heartbeats, pale mucous membranes, and lacking any ventilatory effort should be immediately resuscitated. If ventilation is shallow, erratic, or labored the neonate should be closely monitored and the veterinarian should be prepared to intubate the neonate. Strong vigorous neonates should be rechecked each 30 seconds and incubated if respiratory distress begins to occur. The success of the resuscitation is dependent upon early support before cardiovascular failure occurs. The first step in ventilatory support is to intubate the trachea. Attempts to inflate the lungs by blowing through the nose of the neonate, or by using a mask, will result in air filling the stomach, since the resistance to inflate the stomach is less than the resistance to displacement of the lung liquid. However, if this is the only means available to you for inflating the lungs, do it. Neonatal animals are relatively easy to intubate. The key to successful intubation is extension of the head and the neck to straighten the airway. An assistant is helpful for positioning the neonate. Placement of the neonate in ventral recumbency helps intubation. Puppies & kittens - Because of their small size, Cole endotracheal tubes are best for these neonates. Depending on the breed a lighted laryngoscope may or may not be needed. You should have one available. Following incubation the neonate should be ventilated. Inflation of the fetal lungs will be difficult until the lung liquid is absorbed through the alveoli. Several commercial ventilators are available. However, it is possible to inflate the lungs of the neonate by blowing through the endotracheal tube. This is often the only readily available source for positive pressure ventilation. Most full-term neonates will readily convert to the neonatal circulatory pattern following several deep breaths. A few may require sustained ventilatory support in order for the lungs to remain filled with air. Once the neonate begins to breathe and is able to forcefully move a sizable volume of air through the endotracheal tube, ventilatory support can be stopped. The endotracheal tube should remain in place until the neonate strongly objects to the presence of the tube. Swallowing, coughing, and the ability to hold its head up are signs that the endotracheal tube is no longer needed. Following intubation and lung inflation, additional methods of postpartum care can be utilized. Since heat loss can rapidly occur in newborns due to evaporation and convection, care should be taken to keep the neonate warm and dry. Hypothermic infants are unable to respond to normal amounts of stimulation and frequently will not suckle or breathe adequately. Dextrose containing fluids can be given intravenously to the neonate in order to provide a readily available energy source. Forced feeding of neonates that lack strong reflex responses may result in pulmonary aspiration of the milk. Furthermore, if the neonate is hypothermic its ability to digest and absorb milk-based nutrients will be markedly slowed. Fluid therapy may be indicated in those newborns with a low intravascular volume and inadequate perfusion of tissues as determined by capillary refill time (CRT). Neonatal animals display characteristic behavior patterns when they are anoxic. Initially there is struggling, gasping, hypertension and bradycardia. This is followed by a short period of apnea, then a period of more regular and deeper gasping with a slight increase in heart rate. Following this is a second period of apnea that is often fatal due to cardiovascular failure. Stimulatory drugs such as Doxapram have been used in apneic animals in an attempt to stimulate ventilation. In low doses Doxopram stimulates respiration by stimulating carotid chemoreceptors, but in higher doses it stimulates both respiratory and non-respiratory centers in the medulla. Doxopram and other stimulatory drugs are not effective if used during the second period of apnea since the chemoreceptors are already maximally stimulated. These drugs may be of some benefit if used in the initial period of apnea. However, the key to resuscitation of the neonate in the latter stages of anoxia is full inflation of the lungs with air or oxygen by Positive pressure ventilation. DON’T SHAKE BABIES NOTE: Hanging the new born upside-down, swinging, sucking fluid from the lungs or slapping them to stimulate initiation of ventilation is not effective and should not be part of neonatal resuscitation.