Royal Hobart Hospital Renal Services
advertisement

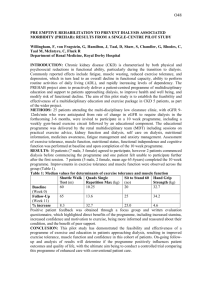
32 Development of a Home Therapies First Policy Award category: Best Team Contribution for Service Excellence, Leadership Award through new Ways of Working and Leadership Award for Safety and Quality Contact: Royal Hobart Hospital Renal Services 0438 589 811 Within Royal Hobart Hospital’s (RHH) Renal Unit we developed and implemented a philosophy of Home Dialysis ‘First’. This was in response to the increasing literature showing the benefits of self-management in chronic disease patients and of home dialysis in comparison with in centre (3 x per week) treatment. Individual benefits include patient empowerment, improved quality of life, decreased travel for treatment, ability to dialyse longer and more frequently, flexibility to dialyse at a time that suits their lifestyle and improved health outcomes. There are also secondary benefits such as decreased rates of hospitalisation, ability to return to and maintain a productive working and family life and significantly lower cost to the health system (Kidney Health Australia. 2012, pp. 11-12). We have also realised since introduction that the phrase Home Dialysis ‘First’ is a misnomer. Not all patients go home, but some remain independent in the training facility. We are therefore promoting patient independence in their dialysis treatment. Other patients achieve varying degrees of independence called assisted care. In 2010 Kidney Health Australia (KHA) undertook a nationwide consumer survey of adult dialysis patients. This survey showed that 30% of Tasmanian dialysis patients would be willing to dialyse at home. Our project was to change our model of care to promote independent dialysis and self-management as the preferred dialysis option, thus aligning with our philosophy. Results from the 2010 KHA survey also enabled conclusions to be drawn about barriers to home dialysis. Patients are generally comfortable once they are established on dialysis; this implies that to improve home dialysis rates, patients need to be exposed to home therapies early to avoid the “status quo” bias against changing to these therapies once established (Kidney Health Australia, 2011). In developing our model of care we have combined our Chronic Kidney Disease (CKD) Educator, Home Haemodialysis (HHD) and Peritoneal Dialysis (PD) teams and placed them in one facility, the Karingal Renal Education Centre (KREC). Previously they had worked relatively independently of each other. The patient experience has now changed from a nurse dependent dialysis to independent dialyser who is already reaping the benefits of their own dialysis. Our patients attend pre dialysis education and information in KREC and are now exposed to other patients self-managing their own care from the start of their dialysis journey. Pathways were developed from CKD through to treatment options (Appendix 1) and a framework for home haemodialysis was developed to assist in defining the level of independence achievable by the individual. This then determines dialysis location. Buy in was sought and achieved from all members of the renal multidisciplinary team (Dr’s, Nurses, Allied Health). Patients are now provided with the opportunity to make an informed choice on their treatment option in consultation with the CKD educator. This aligns with the core principles in the Australian Commission on Safety and Quality in Health Care (ACSQHC) framework. Namely, to provide care that is consumer centred, driven by information and organised for safety (ACSQHC. 2013). Since commencing this project we have doubled our Home Haemodialysis patient numbers from 6 at the start of the project to 12. Our patients are better educated prior to commencing dialysis and are able to make an informed choice on the dialysis treatment which works for them. Our patients can also transfer between home/independent treatment modalities easily as suits their situations. It encourages empowerment and flexibility and better health outcomes for this patient cohort. The majority of our independent patients dialyse of an evening thus allowing them to retain their days to live normally and many of these patients are able to continue to work and enjoy family life. Patients have a continuum of education and categories of ability and realistically not all can become fully independent. Patients who are unable to achieve full independence can meet varying degrees of self-management. These patients are classified as assisted care and can perform aspects of their own treatment as assessed by staff. This means that instead of them failing to meet certain criteria, they can take pride in what they are able to achieve. We have implemented a range of quality improvement initiatives stemming from the new model of care to ensure that we continue to create a better service for our cohort. These include: Commencement of an annual Peritoneal Dialysis (PD) Master Class aimed at providing a continuation of education and tips for PD patients to keep them healthy and happy on PD. These classes are very person centric, collaborative and promote home dialysis. They are attended by our medical team and involve consultation with dieticians and social workers in their planning. Feedback is always gathered from the patients and families in order to meet their needs and improve what we do. It has been excellent and attendance is always good (approx. 85%). It provides an opportunity for PD patients to come together to share experiences and tips, and the feedback has demonstrated how helpful our consumers have found this to be. One example quoted from feedback comments, “I am not alone”. Aside from training to undertake their dialysis modality, people who are diagnosed with the beginning stages of CKD are able to come to KREC and be seen by our CKD educator prior to needing dialysis to learn about their disease and their treatment options. This enables them to prepare for the upcoming changes and to learn how to stay as well as they can at home. We find that patient’s feel much more prepared when they have had the time, along with their family/support systems, to consider what option best fits their lifestyle. At KREC we have included space for both the renal Social Worker and Dietician to set up and work. They are both able to see patients here, and easily have involvement with new/home therapy and independent patients. We find this very useful as do our cohort. Often, pre dialysis patients are able to not just see the Chronic Kidney Disease Educator, but to be reviewed by the dietician who will work with them to keep them as well as they can be at home, prior to commencing dialysis. They also then have the benefit of the social worker being close by, enabling for early prepare for any extra support patients will require. We gained a grant from Kidney Health Australia (KHA) to perform a 12 month trial of patient education/social classes aimed at CKD and home patients to show them healthy and tasty eating choices on their required dietary restrictions and easy exercise classes to promote healthy living such as Tai Chi. The feedback from this was so widely positive that KHA have taken this on board and created the Kidney Club which is modelled after it. The development of a brand new initiative in creating ‘Independent dialysis pods’ with 24/7 access in the Karingal Renal Education Centre has proved to be very beneficial for our patients. The ‘pods’ provide another dialysis option for independently trained patients. They are given a fob access and dialyse within the facility independently once they are fully accessed and signed off by staff. It is extremely useful for those patients who are unable to or don’t wish to perform their dialysis in their own home. Patients who are deemed safe and competent can attend the facility during or after hours for treatment at their convenience, around work, school, family and social commitments. This flexibility has provided an opportunity for those patients who are capable to still become independent instead of being unable due to logistics. After much work and collaboration they have been set up with all necessary safety measures (security cameras, door release in case of emergency, checklists and accessible portable telephones) and are fully operational. Patients continue to have regular meetings with the multidisciplinary team to ensure that they are well and continuing to be safe. Our team has created multiple documents and guidelines to support our service such as pamphlets (appendix 3) training records, troubleshooting and setup manuals for each of the machines as well as guidelines for assistance with PD dressings. These get constantly updated, and one improvement we have made because of some patients input (who learn by pictures better than reading), we have added photographs of set up steps into our dialysis machine manuals. We have seen a great increase in the family support and involvement for the individual suffering chronic Kidney disease. One of our Nephrologists has been able to commence a monthly home therapy clinic at KREC, whereby patients can come with their families to discuss their progress with their doctor, nursing staff, social worker and renal dietician. This clinic is both informative for nursing staff to guide us in the care we give to the individual, but also as an educational opportunity for the patient and their family. We have also reintroduced an after hours nurse call system to support our independent patients (both peritoneal and haemo) who dialyse over the weekend, night times or in the evenings.