A systematic evaluation on the pattern of treatment of osteoporosis
advertisement

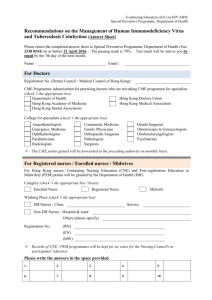
Awareness and pattern of management of osteoporosis among medical practitioners in Hong Kong Tai Pang Ip1, Cindy Loo Kuen Lam2, Annie Wai Chee Kung3 1 Division of Endocrinology, Department of Medicine, Tung Wah Eastern Hospital; 2Family Medicine Unit, 3Division of Endocrinology, Department of Medicine, University of Hong Kong, Queen Mary Hospital, Hong Kong, PR China. Introduction: Epidemiological studies have projected a vast increase in osteoporotic fractures in Asia. Awareness of osteoporosis among medical professionals and the pattern of management in Asia have not been explored. Objectives: To evaluate the awareness of osteoporosis and the pattern of management in two groups of medical practitioners in Hong Kong: (1) hospital-based practitioners in the public sector (PH); (2) clinic-based private practitioners (PC). Methods: 504 medical practitioners in Hong Kong with their self-reported practice likely to receive clients with or at high risk of osteoporosis were invited to complete a postal questionnaire on the diagnosis and management of their osteoporosis patients. Results: Overall response rate was 41% (PH33%, PC51%). 76% of the whole cohort reported treating osteoporosis patients in their practice. 91% believed that osteoporosis was under-diagnosed. The asymptomatic nature of the disease (66%), inaccessibility (45%) and high cost (54%) of the diagnostic tools were considered major reasons for under-diagnosis. DEXA was employed for diagnosis by only 53% of the physicians (PH 51%, PC 55%; p=NS). Calcaneal bone ultrasound was used by 31% of the responders as the only diagnostic tool, especially among clinic-based doctors (PC 45%, PH 17%, 0.001). 33% of the surveyed doctors were unaware of published guidelines for BMD measurements. Concerning treatment goals, 82% considered prevention of future fracture (PH 85%, PC80%; p=NS) and 66% believed improvement in the quality of life of patients (PH64%, PC70%; P=NS) as critical or highly important whereas only about half of the doctors thought that increase in BMD (PH46%, PC57%; P=NS) and low side effect of therapeutic agents (PH52%, PC60%; P=NS) were important treatment goals, and about 1/3 of the doctors claimed that convenient dosing schedule (PH27%, PC38%; P=NS) and presence of analgesic effect of the drugs (PH33%, PC40%; P=NS) were important. On the other hand, 60% of the doctors (PH61%, PC60%; P=NS) considered the cost of therapy a critical or highly important element in the management. Conclusions: This study showed that doctors in Hong Kong were aware of osteoporosis, though the disease was still under-diagnosed and under-treated due to inaccessibility and high cost of the diagnostic tools and therapeutic agents. These findings stress the importance of expanding efforts to update the knowledge and increase the awareness among health care providers and also provide future directions for developing strategies for management of osteoporosis in developing Asian regions.