AAA
advertisement

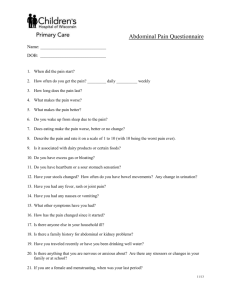
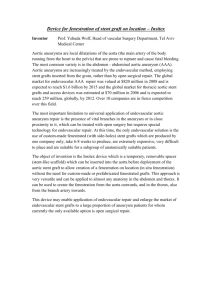
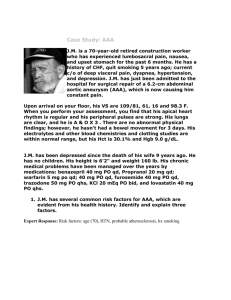
1 Patient History A 70 year old male smoker with a history of high blood pressure came into the Portland VA Medical Center on 10/28/05 for his routine chest x-rays, as well as an ultrasound. The patient’s Doctor ordered this ultrasound exam as follow-up for his previous surgeries which included a coronary artery bypass graft (CABG) on 02/05/93, a Cholecystectomy on 05/10/93, and an inguinal hernia repair on 03/15/96. Incidentally, the ultrasound revealed that the distal portion of the patient’s abdominal aorta contained a 7.5 cm. segment of aneurysm. To confirm the location and dimensions of the aneurysm, abdominal and pelvic CT’s were performed almost a year later, on 08/28/06. After confirming the diagnosis from ultrasound and CT, an endograft operation was scheduled for 11/16/06. Typically, since the aneurysm was greater than 5 cm, it should have been treated immediately to avoid the risk of a potentially fatal rupture. It was unknown as to why the patient or Doctor waited almost a year to perform a confirming CT exam and an endograft operation to follow. Most likely, they decided to wait in order to distinguish whether the aneurysm would change dimensions or remain the same size. According to the University of Michigan Health System, if a patient is diagnosed with an aneurysm and it is repaired through open surgery, the mortality rate for that patient is about 5 percent. If, however, the aneurysm is repaired through open surgery after it has ruptured, the mortality rate is about 80 percent. In this case, the Doctor seemed to be taking a detrimental risk when they waited almost a year for the follow up CT’s and the endograft treatment. About Abdominal Aortic Aneurysms An Abdominal Aortic Aneurysm (AAA) is a localized dilation or bleeding of the abdominal aorta that exceeds the normal diameter by more than 50 percent (Endo, 2007). 2 Abdominal aortic aneurysms are the 12th leading cause of death in the United States and roughly 80 percent of aortic aneurysms occur in the abdominal aortic segment below the kidney arteries. Each year, about 3 percent to 9 percent of those between the ages of 60 to 70 years old, have abdominal aortic aneurysms (Endo, 2007). Many of these aneurysms are a silent problem because they are difficult to detect and some patients feel no abdominal pain. Although the aneurysm proved to be an incidental finding in this patient’s case, the patient history suggested otherwise. Statistically, smoking and high blood pressure increase the risk of aortic aneurysms. Figure 1: Abdominal Aortic and Left Common Iliac Aneurysms www.vascularsociety.org.uk Ultrasound Findings The abdominal aortic ultrasound completed on 10/28/05, concluded that the maximum dimensions of the aneurysm measured 5.8 x 5.8 cm. The proximal abdominal aorta measured 2.4 x 2.3 cm. and the mid-abdominal aorta measured 2.3 x 2.4 cm. The right and left common iliac arteries appeared normal, measuring 1.2 cm correspondingly. 3 Figure 2: Ultrasound of the AAA CT On 08/28/06, almost a year after the initial ultrasound, the CT techs obtained a noncontrast CT of the patient’s abdomen and pelvis using 5 mm. axial images through the abdomen. Following the administration of 100 cc of Ultravist, 2 mm. axial images were then obtained through the abdomen and pelvis in the arterial phase (Radiologist’s report). Anatomy Normally, almost every organ of the body is demonstrated on an abdominal CT. This includes the spleen, liver, pancreas, gallbladder, adrenal glands, portal vein, aorta, inferior vena cava, superior mesenteric vein, all portions of the colon, stomach, kidneys, inferior mesenteric artery, duodenum, left and right renal veins and arteries, small intestine, common hepatic artery, celiac trunk, and the splenic artery and vein (Netters). CT Findings According to the Radiologist’s report, mild scarring was present at the right lung base. A sub centimeter hypo density was also seen within the lower pole of the right kidney, which represented a simple cyst. Colonic diverticula were present and the gallbladder was surgically removed. An increased enhancement within the liver measured 5 mm. in the posterior segment, 4 most likely representing a focus of heterogeneous enhancement. In addition to the Radiologist’s report, the angiography techs noticed a large cyst in the anterior portion of the left kidney. Figure 3: CT of abdomen displaying a left renal cyst The Radiologist’s report also described the conventional arterial aortic anatomy such as single renal arteries shown bilaterally, a single left renal vein, and early branching of the right renal vein. Additional findings confirmed that a fusiform infrarenal abdominal aortic aneurysm measured 6.7 x 6.7 cm. in the greatest dimension. The aneurysm extended to the bifurcation and into the left common iliac measuring 2.6 x 2.7 cm, and into the right common iliac measuring 2.0 x 2.4 cm. Compared to the previous ultrasound measurements on 10/28/05, these dimensions confirmed a dramatic increase in the size of the aneurysm as well as both common iliac arteries. Based upon these findings, the patient’s Doctor scheduled an abdominal aortic aneurysm repair with a stent graft placement. Figure 4 & 5: CT angiograms (CTAs) of the AAA 5 Figure 6 & 7: CT’s of the AAA Figure 8: Angiogram of the AAA Angiography Three months after the patient’s abdominal and pelvic CT, the patient was admitted to the hospital on 11/16/06 for an endograft procedure. In the past, the most common way to treat an aneurysm before it ruptured was to perform a highly invasive surgery that required a large abdominal incision in order to repair the aneurysm. The newly approved endograft procedure, however, treats the AAA from the inside out. This innovative method entails the Doctor placing a stent graft and a woven polyester tube inside a diseased vessel without surgically opening the tissue adjoining the diseased vessel. This endovascular graft is approximately the size of a pencil in diameter. With the endograft in place, 6 blood can travel from the heart, through the device, into the pelvis, and bypass the aneurysm. This endograft has an 80 percent to 90 percent success rate for patients and a much faster recovery rate than other surgical techniques (Endo, 2007). Figure 9: Endovascular Stent Graft (Endograft) www.angioplasty-vir.com Preparation Before the patient arrived in the angiography suite, the techs prepared the sterile table and set up the necessary equipment needed for the procedure. Although the endograft procedure was less invasive than past surgical procedures, the surgery team’s attendance was mandatory. In total, approximately twenty people filled the angiography suite. Technical Process According to the Radiologist’s report, the Doctor obtained informed consent after the Physical Activity Readiness Questionnaire (PARQ) conference. The patient was brought to the angiography suite and placed under general anesthesia using 10,000 units of Heparin. 300 ml of Visipaque-320 contrast was administered during the procedure. A small incision was made at the patient’s groins and access was gained into both common femoral arteries using open 18 gauge needles. Two Perclose arteriotomy sutures were placed within each arteriotomy site without closure of these sutures. The Doctor placed 8 French vascular sheaths in both groins as well as a 5 French marker pigtail within the abdominal aorta at the level of the renal arteries. 7 An aortogram was performed and measurements were taken to choose the appropriate stent graft. Next, the left vascular sheath was exchanged for an 18 French vascular sheath. Through a left transfemoral approach, a 23 mm x 14.5 mm x 180 mm main body portion of a stent graft was deployed without incident. The Doctor selected the contralateral limb gate through the right vascular sheath by using a 5 French Berenstein catheter and Storq wire. A 12 French sheath was placed within the right groin after the Berenstein catheter and sheath were removed. Through this approach, a 14.5 mm x 120 mm contralateral stent graft limb was deployed without incident. Angioplasty was then performed at the proximal portion of the stent graft, at the gate of the contralateral limb, and at the iliac limbs. Post stent graft deployment angiography was performed. All wires and catheters were removed, and hemostasis was achieved using the prepositioned Perclose devices and manual compression. After successful placement of the AAA endograft, the Doctor noticed a small residual type 2 endoleak at the contralateral gate junction. Considering the patient’s heparinized status, the Doctor thought the leak would seal in time. The patient was then transferred to the Intensive Care Unit in stable condition (Radiologist’s report). Figure 10: Angiogram after placement of endograft 8 Prognosis On 12/15/06, one month after the AAA endograft repair, the CT techs performed a follow-up abdomen and pelvis CT. Technical Process The CT techs obtained 5mm axial non-contrast images of the abdomen and pelvis. The techs then administered 100 cc of Ultravist intravenous contrast. Following the administration of contrast, the techs achieved 2mm delayed images through the abdomen and pelvis. CT Findings The gallbladder was surgically absent and the patient’s aorta displayed atherosclerosis. The 6.7 x 6.9 cm abdominal aortic aneurysm was unchanged. It was infrarenal and extended down to the bifurcation with unchanged, bilateral proximal common iliac artery aneurysms. The follow up CT exhibited a patent aortic stent graft with no evidence of an endoleak. The Radiologist also concluded that a stenosis of the left renal artery existed at the origin. In addition to the stenosis, the Radiologist noted the already existing large left upper pole renal cyst measuring 2.5 cm in diameter. Scattered colonic and moderate sigmoid diverticulosis was present, without evidence of diverticulitis (Radiologist’s report). Figures 10, 11, & 12: Post CT and CTAs of the AAA 9 Given that endovascular repair is a fairly new development, the patient might require further operations to ensure that his stent graft remains effective. Around 5 to 10 percent, or 1 in 10-20 patients undergoing an endograft, will require a further procedure every year to keep the stent working normally and prevent the aneurysm from rupturing (Mosquera, 2002). Although risks of rupture exist, endovascular stenting remains the preferred treatment for nearly half of all patients with aneurysms in the United States (Nowygrod, 2006). After confirming that the patient’s AAA and common iliac artery aneurysms were unchanged, and without continuing evidence of an endoleak, the patient’s procedure proved to be a success. Although he will continue to be closely monitored after the operation and for the rest of his life, the benefits of his endovascular repair greatly outweighed the risk.