food poisoning in three family dairy herds associated with
advertisement

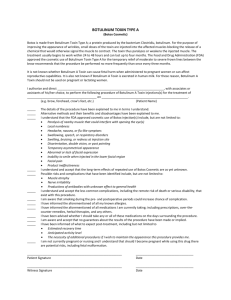
ISRAEL JOURNAL OF VETERINARY MEDICINE Vol. 56 (3) 2001 FOOD POISONING IN THREE FAMILY DAIRY HERDS ASSOCIATED WITH CLOSTRIDIUM BOTULINUM TYPE B. S. Bruckstein and A. M. Tromp Hechaklaiet, Beer Tuvia, 83815, and Koret School of Veterinary Medicine, Hebrew University of Jerusalem, Israel Abstract In spring 1995 an outbreak of suspected botulism type B occurred in three dairy farms simultaneously. The affected animals were adult milking cows suffering from total lack of appetite, diarrhea, dehydration, increased salivation, and regurgitation mostly of saliva and fluids. The milk yield drastically decreased. Of the 24 affected cows some recovered, but 14 cows had to be slaughtered. In most of the slaughtered animals the principal finding was an acute or subacute aspiration pneumonia. Toxicological examinations were negative for botulinum toxins but Clostridium botulinum type B was isolated from the abomasum contents and from the liver of one animal. All the farms in the area obtained their feed from a central, cooperative feeding plant. Six days before the outbreak the three farms were supplied with their daily ration from a single batch from the same mixing wagon. Based on the clinical symptoms, the single source of the feed, the negative toxicological examinations, but the isolation of Clostridium botulinum type B from the abomasal contents of one cow suggest strongly that this outbreak was caused by type B toxin. The differences between the syndrome caused by Botulinum type B toxin and that caused by Botulinum types C and D toxin are discussed. Introduction The neurotoxins produced by the Clostridium botulinum bacterium affect all mammals. The Gram positive, anaerobic, sporeforming bacterium produces exotoxin during its growing stage and during autolysis(1). Eight types of exotoxins are known: A, B, Ca, Cb, D, E, F, and G. Each type differs in toxicity for different mammals and in geographical distribution. The toxin is thermolabile, but the spores are heat resistant. During beer production, for example, temperatures of 750C - 850C are reached that kill the toxin, but the spores may survive. The disease is caused in one of three ways: By ingesting food containing the preformed toxin, contamination of an open wound, as in tetanus, and ingestion of the bacterium, resulting in the production of exotoxin within the digestive tract, so called toxico-infection (2). Ingestion of preformed toxin is the most prevalent way of infection (1). Type B botulism is especially widespread in the central Atlantic states of the U.S.A.(1). Of the two forms of B-toxins, the proteolytic toxin is the most virulent; while the nonproteolytic toxin affects the cholinergic nerves. Muscles containing more efferent nerves, such as the pharyngeal muscles, are affected first (1). Detection of the toxin is rarely accomplished by routine laboratory examination. The procedure consists of injecting mice intraperitoneally with food, feces, serum, and organs extracts. By protecting mice with specific antiserum the type of toxin is determined. A definitive diagnosis is accomplished only through determination of the toxin. A tentative diagnosis is made on the basis of clinical symptoms and isolation of the organism from the feed or the digestive tract contents. Other paralytic disorders can be differentiated from botulism by electromyography (1). Type C and D Botulism intoxication of cattle is in most cases related to animal protein derived from cadavers infected with Clostridium botulinum. Type B botulism differs since it needs vegetable protein to grow and produce toxin. A number of publications describing outbreaks of Type B botulism mention as possible sources of the vegetable-rich protein, food ingredients such as brewers’ grains, soya beans, soya silage, alfalfa silage, rotting vegetables and spoiled rye silage with a high pH (1,3,4,5-8). In Holland 22 Farms were infected with botulism type B in 1977, as a result of ingesting wet brewers’ grains. The epidemiological investigation and an experimental feeding trial were performed at the faculty for Veterinary Medicine of Utrecht, and proved that the syndrome was caused by type B botulism intoxication. The clinical aspects and the disease pattern are completely different from botulism caused by C or D type toxin (3,9). Indigestion and diarrhea are the first symptoms of type B Botulism. Type B toxicosis is characterized by the involvement of the digestive tract and the prominent clinical signs are considerably increased salivation, caused by difficulties in swallowing and regurgitation resulting in aspiration pneumonia. No recumbency or weakness or paralysis of the hind legs is observed. Publications describe these clinical symptoms as atypical food intoxication caused by botulism type B (3,9). These publications discuss the difficulty in isolating the toxin from blood, organs or food. In the 1977 outbreak in only 4.4 % of the cases was the toxin detected by laboratory tests. Manifestation of the Disease The outbreak occurred in three dairy farms (A,B,C) of about 50 cows each. In farm A, 8 cows were affected and 5 were slaughtered, in farm B, 10 were affected and 7 were slaughtered and in farm C, 2 of the 6 affected cows were slaughtered. The farms obtain their feed for all their dairy cattle from the same cooperative feeding plant. This plant supplies a total ration containing corn-silage, grain-silage, hay and concentrates. A mineral mixture is added and various by-products from fruit and vegetable production are used depending on the availability. This plant supplies feed to about 4000 dairy cows. It is prepared in 6 mixer wagons containing 6000 kg each yielding 133 total rations. A computer automatically records the farm, the amount delivered, the date, time and type of feed. Six days before the outbreak the three farms received their daily total ration from a single batch brought by the same wagon. All the animals are routinely vaccinated with a botulinum type C and D toxoid. On each farm, 6 to10 adult cows, in various stages of the lactation were affected. The clinical symptoms were: anorexia, decline in milk production, increased salivation, vomiting, and a part of the affected animals had severe greenish diarrhea with a bad smell, while some cows passed pasty faeces. The sick cows were apathetic, and they salivated enormous volumes of fluid and suffered waves of regurgitation rising through the esophagus and discharged through mouth and nostrils. After only 5 minutes the manger was filled with great pools of fluid. On two farms two cows died on the first day of the outbreak. Extreme loss of body condition occurred shortly after the beginning of the outbreak. Physical examination: Heart rate was 84 beats/minute, respiration rate increased, few and weak rumenal contractions, and normal body temperature were recorded. One cow suffered from subcutaneous emphysema on the back and dorsal pelvis. This was due to rupture of the pleura allowing air to exit through the mediastinum into the subcutis. Course of the Disease During the 10 days following the onset of the disease, some of the herd improved, while others deteriorated and had to be culled. A total of 14 of 24 worst affected cows were culled and the other 10 recovered. As a specific therapy does not exist, treatment was limited to symptomatic and supportive medication. Laboratory Findings Blood, urine, contents of the digestive tract, and feed ingredients were examined bacteriologically and toxicologically. Organic phosphorus, carbamates and chlorinated hydrocarbons were not detected, nor was cholinesterase. Urine and feed ingredients were examined for nitrates with negative results. Necropsy Postmortem examination of the 14 cadavers showed the following: all were in poor condition with dry and compacted rumenal contents. The other parts of the digestive tract contained thin, bloody feces. An acute or subacute diffuse pneumonia was observed in 6 culled cows. Brain examinations for rabies were negative. Rumen content and lungs were examined bacteriologically and Pasteurella haemolytica type A was isolated from the lungs. Clostridium botulinum type B was isolated from the abomasum and liver of one cow. Type B toxin was not found in the rumen or in suspected feed (Brewers’ grains). Discussion and Conclusion The major question that araises in the diagnosis of Botulism type B may be made on basis of the clinical symptoms and the isolation of the bacterium Clostridium type B, but without demonstration of the toxin. The disease caused by type B botulism presents completely different manifestations from type C and D. The characteristic paralysis of the C and D toxins are never found in botulism B intoxication. Cases of botulism type C and D, caused by silage containing poultry manure or grain- or corn-silage, contaminated with cadavers of mice, rats or snakes are much more frequent. Silage containing poultry manure is one of the food ingredients for fattening baby beef and sometimes for replacement heifers. These animals are therefore exposed to a high risk of botulism type C or D intoxication. Israeli regulations clearly stipulate that poultry manure is forbidden in beef production, but permitted only for young non-pregnant females. Grain- and corn-silage among the staple food ingredients for all cattle in the country and also constitute a danger of botulism type C or D intoxication. A breakdown in the vaccination procedure caused an outbreak in 1994, resulting in the death or slaughter of 70 bulls and young heifers caused by botulism type D but no toxin was identified. The animals were recumbent, the paralysis starting with the tail and progressing to the hind legs. The clinical picture included complete stasis of the digestive tract but no paralysis of the tongue was observed. On the other hand, the increased salivation, regurgitation of saliva and fluids and dehydration were not encountered in the C and D type botulism. In 1977, 175 cows from 22 dairy farms were afflicted in Holland. In only 4% of these cases was the exotoxin isolated, but from 13% of suspected food ingredients (Brewer’s grain) (9). The diagnosis was made on the symptomatology. Organic material from the clinical cases was used in an induced intoxication, resulting in the same clinical symptoms. The isolation of a large quantities of Clostridium botulinum type B from the rumen and faeces of diseased cows further strengthened the diagnosis. It should be realized nevertheless that this orgamism can be found in the gastro-intestinal tract of healthy animals (3). When a number of experimental intoxications were produced with the contaminated Brewer’s grain (4,9,10), it became evident that the toxin that is considered as a typical exotoxin was mostly attached to the bacteriumal cell, with very little free toxin released. This made identification of the toxin extremely difficult (10). Rumen contents or feces contained 105-107 bacteria/gr in cows that were fed with contaminated Brewer’s grain. For more than 8 weeks the infected animals shed bacteria, and infected the surroundings, especially the pasture. (4) The fact that all three farms were supplied with feed from the same wagon 6 days before the clinical symptoms strongly suggests an incubation period of 6 days. In our opinion it is legitimate to base the diagnosis of botulism B on the clinical symptoms and the isolation of large numbers of Clostridium botulinum type B from the gastro-intestinal tract. Differences between Botulism B and Botulism C and D. The syndroms caused by Clostridium botulinum C and D differ completely clinically from the disease caused by Clostridium botulinum B. Experimental infection performed by the Faculty of Veterinary Medicine, Utrecht, helped to document the various symptoms. Botulism B: The comparatively light cases exhibit a syndrome of indigestion, diarrhea or constipation, and a marked decline in appetite and milk production. In more serious case difficulties in swallowing occur, resulting in regurgitation of ruminal fluid and increased production of saliva. (fig 1.) Aspiration pneumonia is a common secondary complication of the acute form (1,4,8,9,10). These clinical signs were observed in the incident described here, however, the afflicted cows stood upright and wandered about, and only in terminal stages complete collapse and paralysis were seen. Half the diseased animals were slaughtered and the other half recovered. In extreme cases recumbency and respiratory distress occurred. Fig. 1. Botulism C and D: The most distinct symptoms of a botulism C or D intoxication are paralysis of the hind part of the body, decrease in the muscle tonus of the tail and the muscles of the hind part of the body, presence of dry and hard feces in the rectum, and the characteristic recumbency. (fig 2.) The recovery of botulism C and D is extremely rare. Fig 2. Atypical forms of botulism B intoxication occur, resulting in a different clinical picture, and very are much related to the specific sensitivity of the infected animals to the toxin and the ingested dose. Treatment of clinical botulism does not exist. Dutch attempts to improve the survival rate by using antiserum B did not succeed. In both groups, in Holland and the event reported here, the survival rate was similar (3). References 1. Divers, T. J., Bartholomew, R. C., Messick, J. B., Whitlock, R. H. and Sweeney, R. W.: Clostridium botulinum type B toxicosis in a herd of cattle and a group of mules. JAVMA, 188(4): 382-385, 1986. 2. Klyza, J. P.: Botulism syndromes: shaker foals and forage poisoning. In: Robinson, N. E., (ed). Current therapy in equine medicine. 1st ed. Philadelphia, WB Saunders Co. pp. 367-370, 1983. 3. Breukink, H. J., Wagenaar, A., Wensing, T., Notermans, S. and Poulos, P.W.: Food Poisoning in Cattle Caused by Ingestion of Brewers' Grains Contaminated with Clostridium botulinum Type B. Tijdschr. Diergeneesk., deel 103(6): 303-311, 1978. 4. Notermans, S., Breukink, H. J., Wensing, T. H. and Wagenaar, G.: Incidence of Clostridium botulinum in the Rumen Contents and Faeces of Cattle Fed Brewers' Grains Naturally Contaminated with Clostridium botulinum. Tijdschr. Diergeneesk. deel 103(24):1327-1333, 1978. 5. Haagsma, J., Haesebrouck, F., Devriese, L. and Bertels, G.: An outbreak of botulism type B in horses. Vet. Rec. 127: 206, 1990. 6. Tamarin, R. and Neeman, L.:The identification of Clostridum botulinum type B toxin as the cause of an outbreak of botulism in equine. Refuah Veterinarit, 19: 45, 1962. 7. Kromholtz, D.: A botulism like disease of equine in Israel. Refuah Veterinarit 19. 49, 1962. 8. Davidzon, M.: Suspected botulism in cattle in Southern of Israel. Refuah Veterinarit, 19: 171, 1962. 9. Haagsma, J. and Terlaak, E.A.: Atypical Case of Type B Botulism in Cattle, Caused by Supplementary Feeding of Brewers' Grains. Tijdschr. Diergeneesk. deel 103(6): 312-325, 1978. 10. Haagsma, J. and Terlaak, E. A.: Cell- Associated Toxin as a Cause of Type B Botulism in Cattle. Tijdschr. Diergeneesk. deel 103(24): 1317-1325, 1978.