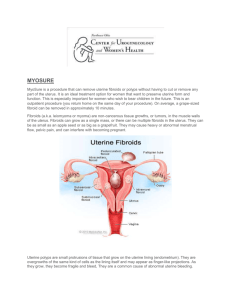
Treatment
advertisement

The Islamic university of Gaza Faculty of nursing Midwifery department Gynecology Sep.2012 1 Menstrual Cycles: Basic Biology: the cycle begins Did you know that when a baby girl is born, she has all the eggs her body will ever use, and many more, perhaps as many as 450,000? They are stored in her ovaries, each inside its own sac called a follicle. As she matures into puberty, her body begins producing various hormones that cause the eggs to mature. This is the beginning of her first cycle; it's a cycle that will repeat throughout her life until the end of menopause. Let's start with the hypothalamus. The hypothalamus is a gland in the brain responsible for regulating the body's thirst, hunger, sleep patterns, libido and endocrine functions. It releases the chemical messenger Follicle Stimulating Hormone Releasing Factor (FSH-RF) to tell the pituitary, another gland in the brain, to do its job. The pituitary then secretes Follicle Stimulating Hormone (FSH) and a little Leutenizing Hormone (LH) into the bloodstream which cause the follicles to begin to mature. The maturing follicles then release another hormone, estrogen. As the follicles ripen over a period of about seven days, they secrete more and more estrogen into the bloodstream. Estrogen causes the lining of the uterus to thicken. It causes the cervical mucous to change. When the estrogen level reaches a certain point it causes the hypothalamus to release Leutenizing Hormone Releasing Factor (LH-RF) causing the pituitary to release a large amount of Leutenizing Hormone (LH). This surge of LH triggers the one most mature follicle to burst open and release an egg. This is called ovulation. [Many birth control pills work by blocking this LH surge, thus inhibiting the release of an egg. Ovulation As ovulation approaches, the blood supply to the ovary increases and the ligaments contract, pulling the ovary closer to the Fallopian tube, allowing the egg, once released, to find its way into the tube. Just before ovulation, a woman's cervix secretes an abundance of clear "fertile mucous" which is characteristically stretchy. Fertile mucous helps facilitate the sperm's movement toward the egg. Some women use daily mucous monitoring to determine when they are most likely to become pregnant. Mid cycle, some women also experience cramping or other sensations. Basal body temperature rises right after ovulation and stays higher by about .4 degrees F until a few days before the next period. Inside the Fallopian tube, the egg is carried along by tiny, hair like projections, called "cilia" toward the uterus. Fertilization occurs if sperm are present. [A tubal pregnancy, called ectopic pregnancy, is the rare situation when e a fertilized egg implants or gets lodged outside the 2 uterus. It is a dangerous life-threatening situation if the fertilized egg starts developing and growing into an embryo inside the fallopian tube or elsewhere. The tube will rupture causing internal bleeding and surgery is require A woman can use a speculum to monitor her own ovulation and use this information to avoid or encourage a pregnancy. This is the allnatural fertility awareness method (FAM) of family planning. Uterine Changes Between midcycle and menstruation, the follicle from which the egg burst becomes the corpus luteum (yellow body). As it heals, it produces the hormones estrogen and, in larger amounts, progesterone which is necessary for the maintenance of a pregnancy. the later stages of healing, if the uterus is not pregnant, the follicle turns white and is called the corpus albicans. Estrogen and progesterone are sometimes called "female" hormones, but both men and women have them, just in different concentrations. Progesterone causes the surface of the uterine lining, the endometrium, to become covered with mucous, secreted from glands within the lining itself. If fertilization and implantation do not occur, the spiral arteries of the lining close off, stopping blood flow to the surface of the lining. The blood pools into "venous lakes" which, once full, burst and, with the endometrial lining, form the menstrual flow. Most periods last 4 to 8 days but this length varies over the course of a lifetime. Some researchers view menses as the natural monthly cleansing of the uterus and vagina of sperm and bacteria they carried. Cramps and Other Sensations Women can experience a variety of sensations before, during or after their menses. Common complaints include backache, pain in the inner thighs, bloating, nausea, diarrhea, constipation, headaches, breast tenderness, irritability, and other mood changes. Women also experience positive sensations such as relief, release, euphoria, connection with nature, creative energy, increased sex drive and more intense orgasms. Uterine cramping is one of the most common uncomfortable sensations women may have during menstruation. There are two kinds of cramping. Spasmodic cramping is probably caused by prostaglandins, chemicals that affect muscle tension. Some prostaglandins cause relaxation, and some cause constriction. A diet high in linoleic and liblenic acids, found 3 in vegetables and fish, increases the prostaglandins for aiding muscle relaxation. Congestive cramping causes the body to retain fluids and salt. To counter congestive cramping, avoid wheat and dairy products, alcohol, caffeine, and refined sugar. Natural options to alleviate cramping: Increase exercise. This will improve blood and oxygen circulation throughout the body, including the pelvis. Try not using tampons. Many women find tampons increase cramping. Don't select an IUD (intrauterine device) as your birth control method. Avoid red meat, refined sugars, milk, and fatty foods. Eat lots of fresh vegetables, whole grains (especially if you experience constipation or indigestion), nuts, seeds and fruit. Avoid caffeine. It constricts blood vessels and increases tension. Meditate, get a massage. Have an orgasm (alone or with a partner). Drink ginger root tea (especially if you experience fatigue). Put cayenne pepper on food. It is a vasodilator and improves circulation. Breathe deeply, relax, notice where you hold tension in your body and let it go. Ovarian Kung Fu alleviates or even eliminates menstrual cramps and PMS, it also ensures smooth transition through menopause Take time for yourself! -Anecdotal information suggests eliminating Nutra-Sweet from the diet will significantly relieve menstrual cramps. If you drink sugar-free sodas or other forms of Nutra-Sweet, try eliminating them completely for two months and see what happens. The hormones in our bodies are especially sensitive to diet and nutrition. PMS and menstrual cramping are not diseases, but rather, symptoms of poor nutrition. Premenstrual Syndrome or PMS -PMS has been known by women for many years. However, within the past 30 or so years, pharmaceutical companies have targeted and created a market to treat this normal part of a woman's cycle as a disease. These companies then benefit from the sale of drugs and treatments. -Premenstrual syndrome refers to the collection of symptoms or sensations women experience as a result of high hormone levels before, and sometimes during, their periods. 4 -One type of PMS is characterized by anxiety, irritability and mood swings. These feelings are usually relieved with the onset of bleeding. Most likely, this type relates to the balance between estrogen and progesterone. If estrogen predominates, anxiety occurs. If there's more progesterone, depression may be a complaint. -Sugar craving, fatigue and headaches signify a different type of PMS. In addition to sugar, women may crave chocolate, white bread, white rice, pastries, and noodles. These food cravings may be caused by the increased responsiveness to insulin related to increased hormone levels before menstruation. In this circumstance, women may experience symptoms of low blood sugar; their brains are signaling a need for fuel. A consistent diet that includes complex carbohydrates will provide a steady flow of energy to the brain and counter the ups and downs of blood sugar variations. -It's true that most women will have cycles that are around 28 days. But, a woman can be healthy and normal and have just 3 or 4 cycles a year. [However, while variations might be healthy and normal, they could also be a sign of a serious underlying problem. For example, a recent news article suggested that irregular menstrual cycles may predict Type 2 Diabetes.] -Ovulation occurs about 14-16 days before women have their period (not 14 days after the start of their period). The second half of the cycle, ovulation to menstruation, is fairly consistently the same length, but the first part changes from person to person and from cycle to cycle. In rare cases, a women may ovulate twice in a month, once from each ovary. -Conception/Fertilization of an egg, can only occur after ovulation. The egg stays alive for about 24 hours once released from the ovary. Sperm can stay alive inside a woman's body for 3-4 days, but possibly as long as 6-7 days. If a couple has intercourse before or after ovulation occurs, they can get pregnant, since the live sperm are already inside the woman's body when ovulation occurs. Thus a woman can become pregnant from intercourse for about 7-10 days in the middle of her cycle. -Fertility Awareness is a birth control method where women monitor their cycles daily to identify ovulation. They are learning to predict ovulation to prevent or encourage pregnancy. It requires training and diligent record keeping. From our work providing abortion services, we know that some women can be pregnant and continue to have periods at the same time. We also know of cases where women have gotten pregnant during their menstrual period. 5 Common Menstrual Problems -Most issues teens confront when they start menstruating are completely normal. In fact, many girls and women have had to deal with one or more of them at one time or another: -Premenstrual Syndrome (PMS) PMS includes both physical and emotional symptoms that many females get right before their periods, such as: acne bloating fatigue backaches breasts tenderness. headaches constipation diarrhea food cravings depression or feeling blue irritability difficulty concentrating difficulty handling stress -Different girls may have some or all of these symptoms in varying combinations. PMS is usually at its worst during the 7 days before the period starts and disappears soon after it begins. But girls usually don't develop symptoms associated with PMS until several years after menstruation starts — if ever. -Although the exact cause of PMS is unknown, it seems to occur because of changing hormone levels, and their effect on chemicals in the brain. During the second half of the menstrual cycle, the amount of progesterone in the body increases. Then, about 7 days before the period starts, levels of both progesterone and estrogen drop. Some girls' bodies seem to be more sensitive to these hormone changes than others. Talk to your daughter's doctor if her symptoms are severe or interfere with her normal activities. 6 Cramps: -Many girls experience abdominal cramps during the first few days of their periods. They're caused by prostaglandin, a chemical in the body that makes the smooth muscle in the uterus contract. These involuntary contractions can be either dull or sharp and intense. -The good news is that cramps usually only last a few days. But call your daughter's doctor if she has severe cramps that keep her home from school or from doing stuff with her friends. Irregular Periods -It can take 2 to 3 years from a girl's first period for her body to develop a regular cycle. During that time, the body is essentially adjusting to the influx of hormones unleashed by puberty. And what's "regular" varies from person to person. The typical cycle of an adult female is 28 days, although some are as short as 21 days and others are as long as 45. -Changing hormone levels might make a girl's period last a short time during one month (just a few days) and a long time the next (up to a week). She may skip months, get two periods almost right after each other, or alternate between heavy and light bleeding from one month to another. -But any girl who's sexually active and skips a period should see a doctor to make sure she's not pregnant. And if your daughter's period still hasn't settled into a relatively predictable pattern after 3 years, or if she has four or five regular periods and then skips her period or becomes irregular, make an appointment with her doctor to check for possible problems. Also let your daughter's doctor know if her cycle is less than 21 days or more than 45 days, or if she doesn't get a period for 3 months at any time after first beginning to menstruate. Delayed Menarche -Girls go through puberty at different rates. Some reach menarche (the medical term for the first period or the beginning of menstruation) as early as 9 or 10 years old and others don't have their first periods until they're well into their teen years. So, if your daughter is a "late bloomer," it doesn't necessarily mean there's something wrong with her. 7 -When girls get their periods actually depends a lot on genetics. Girls often start menstruating at approximately the same age their mothers or grandmothers did. Also, certain ethnic groups, on average, go through puberty earlier than others. For instance, African-American girls, on average, start puberty and get their periods before Caucasian girls do. -Let your daughter's doctor know if she hasn't gotten her period by age 15, or by 3 years after starting puberty. Problems That May Be Cause for Concern -Although most period problems are harmless, a few conditions can be more serious and require medical attention: Amenorrhea (the Absence of Periods) Girls who haven't started their periods by the time they're 16 years old or 3 years after they've shown the first signs of puberty have primary amenorrhea, which is usually caused by a genetic abnormality, a hormone imbalance, or a structural problem. Hormones are also often responsible for secondary amenorrhea, which is when a girl who had normal periods suddenly stops menstruating for more than 6 months or three of her usual cycles. -Since pregnancy is the most common cause of secondary amenorrhea, it should always be ruled out when a girl skips periods. In addition to hormone imbalances, other things that can cause both primary and secondary amenorrhea include: stress significant weight loss or gain anorexia (amenorrhea can be a sign that a girl is losing too much weight and may have anorexia) stopping birth control pills thyroid conditions ovarian cysts other conditions that can affect hormone levels -Something that can also cause primary and secondary amenorrhea is excessive exercising (often distance running ) combined with a poor diet, which usually results in inappropriate weight loss or failure to gain weight during growth. But this doesn't include the usual gym class or school sports team, even those that practice often. To exercise so much 8 that she delays her period, a girl would have to train vigorously for several hours a day, most days of the week, and not get enough calories, vitamins, and minerals. Menorrhagia: (Extremely Heavy, Prolonged Periods) -It's normal for a girl's period to be heavier on some days than others. But signs of menorrhagia (excessively heavy or long periods) can include soaking through at least one sanitary (pad) an hour for several hours in a row or periods that last longer than 7 days. Girls with menorrhagia sometimes stay home from school or social functions because they're worried they won't be able to control the bleeding in public. -The most frequent cause of menorrhagia is an imbalance between the levels of estrogen and progesterone in the body, which allows the endometrium (the lining of the uterus) to keep building up. When the endometrium is finally shed during menstruation, the resulting bleeding is particularly heavy. -Because many adolescents have slight hormone imbalances during puberty, menorrhagia isn't uncommon in teens. But in some cases, heavy menstrual bleeding can be caused by problems such as: fibroids (benign growths) or polyps in the uterus thyroid conditions clotting disorders inflammation or infection in the vagina or cervix -If your daughter has heavy periods, or periods that last longer than 7 days, talk to her doctor. Dysmenorrhea (Painful Periods) -There are two types of dysmenorrhea, which is severely painful menstruation that can interfere with a girl's ability to attend school, study, or sleep: 9 1. Primary dysmenorrheal: - is very common in teens and is not caused by a disease or other condition. Instead, the culprit is prostaglandin, the same chemical behind cramps. Large amounts of prostaglandin can lead to nausea, vomiting, headaches, backaches, diarrhea, and severe cramps. Fortunately, these symptoms usually last for only a day or two. 2. Secondary dysmenorrhea : -is pain caused by some physical condition like polyps or fibroids in the uterus, endometriosis, pelvic, or adenomyosis (uterine tissue growing into the muscular wall of the uterus). -Having cramps for a day or two each month is common, but if your daughter has symptoms severe enough to keep her from her normal activities, discuss it with her doctor. Endometriosis: In this condition, tissue normally found only in the uterus starts to grow outside the uterus — in the ovaries, fallopian tubes, or other parts of the pelvic cavity. It can cause abnormal bleeding, dysmenorrheal, and general pelvic pain. Treating Menstrual Problems; -To determine whether a problem requires treatment, the doctor will ask several questions and do a thorough physical exam. The doctor may do a pelvic exam, a Pap smear, blood tests (to check hormone levels), or urine tests. If there might be a structural problem or some sort of growth, an ultrasound or CT scan may be performed. Together, these tests can help the doctor determine how a condition should be handled. -Growths such as polyps or fibroids can often be removed and endometriosis can often be treated with medications or surgery. If a hormone imbalance is to blame, the doctor will likely suggest hormone therapy with birth control pills or other hormone-containing medications. 10 -And for menstrual pain with no underlying medical cause, antiinflammatory medicines are the most effective treatment. Conditions like clotting disorders or thyroid problems may require treatment with medications as well. When to Call the Doctor? -Although most period problems aren't cause for alarm, certain symptoms do call for a trip to the doctor. This is particularly true if a girl's normal cycle changes. So take your daughter to her doctor if she: hasn't started her period by the time she's 15 or her period hasn't become regular after 3 years of menstruating. The most likely cause is a hormone imbalance (which may need treatment), but this also might point to another medical problem. stops getting her period or it becomes irregular after it has been regular. Also let your daughter's doctor know if her cycle is less than 21 days or more than 45 days, or if she doesn't get a period for 3 months at any time after first beginning to menstruate. has heavy or long periods, especially if she gets her period frequently. In some cases, significant blood loss can cause irondeficiency anemia. Also, heavy bleeding could be a sign of a growth in the uterus, a thyroid condition, an infection, or a blood clotting problem. has very painful periods. Having cramps for a couple of days is normal, but if your daughter isn't able to participate in her normal activities, let the doctor know. She might have a medical problem, such as endometriosis, causing the pain. -Helping Your Daughter…. -When your daughter's experiencing a particularly bad bout of PMS or cramps, you can help make her more comfortable. Suggest that she: 11 eat a balanced diet with lots of fresh fruit and vegetables reduce her intake of salt (which can cause water retention) and caffeine (which can make her jumpy and anxious) include foods with calcium, which may reduce the severity of her PMS symptoms try over-the-counter pain relievers like acetaminophen or ibuprofen for cramps, headaches, or back pain take a brisk walk or bike ride to relieve stress and aches soak in a warm bath or put a hot water bottle on her abdomen, which may help her relax -If you notice that your daughter's usual periods are causing her great discomfort and interfering with her life, talk to her doctor to make sure nothing else is causing the problem and to see if anything can help. Sometimes, hormone treatment, usually in the form of birth control pills, can help ease many symptoms associated with uncomfortable periods. -But the most important way you can help your daughter feel more at ease about her period is to talk to her and explain that most annoying or uncomfortable conditions that accompany menstruation are normal and may improve over time. And be understanding when she's cranky and unhappy. After all, no one's at her best all the time — including you. Toxic shock syndrome (TSS) - is a serious but uncommon bacterial infection. TSS was originally linked to the use of tampons, but is now also known to be associated with the contraceptive sponge and diaphragm birth control methods. TSS has also resulted from wounds secondary to minor trauma or surgery incisions where bacteria have been able to enter the body and cause the infection. -The symptoms of TSS include sudden high fever, a faint feeling, watery diarrhea, headache, and muscle aches. There are two types of this condition. The first, toxic shock syndrome, is caused by Staphylococcus aureus bacteria and has been associated with the use of tampons. (TSS was initially linked to a particular type of tampon, which has since been taken off the market.) Although the exact connection is still not clear, researchers suspect that certain types of high-absorbency tampons provided a moist, warm home where the bacteria could thrive. -TSS can affect anyone who has any type of staph infection, including pneumonia, abscess, skin or wound infection, a blood infection called septicemia, or a bone infection called osteomyelitis. -The second type of related infection, streptococcal toxic shock syndrome, or STSS, is caused by streptococcus bacteria. Most often STSS appears after streptococcus bacteria have invaded areas of 12 injured skin, such as cuts and scrapes, surgical wounds, and even chickenpox blisters. Toxic shock syndrome from staphylococcus starts suddenly with vomiting, high fever (temperature at least 102° Fahrenheit [38.8° Celsius]), a rapid drop in blood pressure (with lightheadedness or fainting), watery diarrhea, headache, sore throat, and muscle aches. Within 24 hours, a sunburn-like rash appears. There also may be bloodshot eyes and an unusual redness under the eyelids or inside the mouth (and vagina in females). After that, broken blood vessels may appear on the skin. Other symptoms may include: confusion or other mental changes; decreased urination; fatigue and weakness; thirst; weak and rapid pulse; pale, cool, moist skin; and rapid breathing. Prevention: -The bacteria that cause toxic shock syndrome can be carried on unwashed hands and prompt an infection anywhere on the body. So hand washing is extremely important. -Girls can reduce their risk of TSS by either avoiding tampons or alternating them with sanitary napkins. Girls who use only tampons should choose ones with the lowest absorbency that will handle menstrual flow and change the tampons frequently. Between menstrual periods, store tampons away from heat and moisture (where bacteria can grow) — for example, in a bedroom rather than in a bathroom closet. -Because staphylococcus bacteria are often carried on dirty hands, it's important for girls to to wash their hands thoroughly before and after inserting a tampon. If your daughter is just starting her menstrual period, she should know about taking these precautions. Any female who has recovered from TSS should check with her doctor before using tampons again Diagnosis and Treatment: -Doctors typically diagnose TSS and STSS by doing a physical exam and conducting blood tests that assess a child's liver and kidney function. In toxic shock syndrome, doctors may want to rule out conditions like measles or Rocky Mountain spotted fever, which can produce similar symptoms. A doctor may also take samples of fluid 13 from an abscess, boil, or infected wound to look for a possible source of staphylococcus or streptococcus infection. -Doctors typically treat TSS with antibiotics. If there is a pocket of infection, like an abscess, a doctor also may need to drain the infected area. A child who has TSS is monitored for signs of shock until the condition has stabilized and seems to be improving. Steroids are also sometimes used to treat severe cases of TSS. -As with TSS, doctors typically treat STSS with antibiotics and give intravenous fluids and medications to maintain normal blood pressure. Surgery is sometimes necessary to remove areas of dead skin and muscle around an infected wound. When to Call the Doctor: Call your doctor immediately if your child has any of the following signs and symptoms: 1-Signs of shock: - Go to the emergency department immediately or call an ambulance if your child has cold hands and feet; a pulse that is fast and weak; confusion or other mental changes; pale, moist skin; shortness of breath; abnormally fast breathing; or a strong feeling of anxiety or fear. 2-Signs of TSS: - Look for fever; rash (especially a rash that looks like sunburn); nausea and vomiting; watery diarrhea; confusion or other mental changes; and decreased urination. If your daughter uses tampons, ask her to tell you immediately if she notices any unusual vaginal discharge, especially if it smells strange or bad. Most of the time that will be due to other causes, but no matter the cause, it still rates evaluation. Signs of STSS: Look for the symptoms of shock listed above, plus a fever; blotchy rash; and an area of infected skin that is red, swollen, and painful. -Once you realize that something is wrong, it's important to get medical attention right away. The sooner your child gets treatment, the quicker the recovery will be. 14 Endometriosis (from endo, "inside", and metra, "womb") Definition: is a gynecological medical condition in women in which endometriallike cells appear and flourish in areas outside the uterine , most commonly on the ovaries. The uterine cavity is lined by endometrial cells, which are under the influence of female hormones. These endometrial-like cells in areas outside the uterus (endometriosis) are influenced by hormonal changes and respond in a way that is similar to the cells found inside the uterus. Symptoms often worsen with the menstrual cycle. -Endometriosis is typically seen during the reproductive years; it has been estimated that endometriosis occurs in roughly 5-10% of women. Symptoms may depend on the site of active endometriosis. Its main but not universal symptom is pelvic pain in various manifestations. Endometriosis is a common finding in women with infertility. Signs and symptoms Pelvic pain A major symptom of endometriosis is recurring pelvic pain. The pain can be mild to severe cramping that occurs on both sides of the pelvis, in the lower back and rectal area, and even down the legs. The amount of pain a woman feels is not necessarily related to the extent or stage (1 through 4) of endometriosis. Some women will have little or no pain despite having extensive endometriosis or endometriosis with scarring. On the other hand, women may have severe pain even though they have only a few small areas of endometriosis. However, pain does typically correlate to the extent of the disease. Symptoms of endometriosisrelated pain may include: dysmenorrhea – painful, sometimes disabling cramps during menses; pain may get worse over time (progressive pain), also lower back pains linked to the pelvis chronic pelvic pain – typically accompanied by lower back pain or abdominal pain 15 dyspareunia – painful sex dysuria – urinary urgency, frequency, and sometimes painful voiding Throbbing, gnawing, and dragging pain to the legs are reported more commonly by women with endometriosis. Compared with women with superficial endometriosis, those with deep disease appears to be more likely to report shooting rectal pain and a sense of their insides being pulled down. Individual pain areas and pain intensity appears to be unrelated Other to the surgical diagnosis, and the area of pain unrelated to area of endometriosis Other symptoms may be present, including: Constipation chronic fatigue heavy or long uncontrollable menstrual periods with small or large blood clots gastrointestinal problems including diarrhea, bloating and painful defecation extreme pain in legs and thighs back pain mild to extreme pain during intercourse pain from adhesions which may bind an ovary to the side of the pelvic wall, or they may extend between the bladder and the bowel, uterus, etc. extreme pain with or without the presence of menses premenstrual spotting mild to severe fever headaches depression hypoglycemia (low blood sugar) anxiety In addition, women who are diagnosed with endometriosis may have gastrointestinal symptoms that mimic irritable bowel syndrome Patients who rupture an endometriotic cyst may present with an acute abdomen as a medical emergency. -Occasionally pain may also occur in other regions. Cysts can occur in the bladder (although rare) and cause pain and even bleeding during 16 urination. Endometriosis can invade the intestine and cause painful bowel movements or diarrhea. -In addition to pain during menstruation, the pain of endometriosis can occur at other times of the month and doesn't have to be just on the date on menses. There can be pain with ovulation, pain associated with adhesions, pain caused by inflammation in the pelvic cavity, pain during bowel movements and urination, during general bodily movement i.e. exercise, pain from standing or walking, and pain with intercourse. But the most desperate pain is usually with menstruation and many women dread having their periods. Also the pain can start a week before menses, during and even a week after menses, or it can be constant. There is no known cure for endometriosis Cause While the exact cause of endometriosis remains unknown, many theories have been presented to better understand and explain its development. These concepts do not necessarily exclude each other. 1. Estrogens: Endometriosis is a condition that is estrogendependent and thus seen primarily during the reproductive years. In experimental models, estrogen is necessary to induce or maintain endometriosis. Medical therapy is often aimed at lowering estrogen levels to control the disease. Additionally, the current research into aromatase, an estrogen-synthesizing enzyme, has provided evidence as to why and how the disease persists after menopause and hysterectomy. 2. Retrograde menstruation: The theory of retrograde menstruation, first proposed by John A. Sampson, suggests that during a woman's menstrual flow, some of the endometrial debris exits the uterus through the fallopian tubes and attaches itself to the peritoneal surface (the lining of the abdominal cavity) where it can proceed to invade the tissue as endometriosis. While most women may have some retrograde menstrual flow, typically their immune system is able to clear the debris and prevent implantation and growth of cells from this occurrence. However, in some patients, endometrial tissue transplanted by retrograde menstruation may be able to implant and establish itself as endometriosis. Factors that might cause the tissue to grow in some women but not in others need to be studied, and some of the possible causes below may provide some explanation, e.g., hereditary factors, toxins, or a compromised immune system. It 17 can be argued that the uninterrupted occurrence of regular menstruation month after month for decades is a modern phenomenon, as in the past women had more frequent menstrual rest due to pregnancy and lactation. Sampson's theory certainly is not able to explain all instances of endometriosis, and it needs additional factors such as genetic or immune differences to account for the fact that many women with retrograde menstruation do not have endometriosis. In addition, at least one study found that endometriotic lesions are biochemically very different from transplanted ectopic tissue, which casts doubt on Sampson's theory. 3. Müllerianosis: A competing theory states that cells with the potential to become endometrial are laid down in tracts during embryonic development and organogenesis. These tracts follow the female reproductive (Mullerian) tract as it migrates caudally (downward) at 8–10 weeks of embryonic life. Primitive endometrial cells become dislocated from the migrating uterus and act like seeds or stem cells. This theory is supported by fetal autopsy 4. Coelomic Metaplasia: This theory is based on the fact that coelomic epithelium is the common ancestor of endometrial andperitoneal cells and hypothesizes that later metaplasia (transformation) from one type of cell to the other is possible, perhaps triggered by inflammation. This theory is further supported by laboratory observation of this transformation. 5. Genetics: Hereditary factors play a role. It is well recognized that daughters or sisters of patients with endometriosis are at higher risk of developing endometriosis themselves; for example, low progesterone levels may be genetic, and may contribute to a hormone imbalance. There is an about 10-fold increased incidence in women with an affected first-degree relative. A 2005 study published in the American Journal of Human Genetics found a link between endometriosis and chromosome 10q26One study found that in female siblings of patients with endometriosis the relative risk of endometriosis is 5.7:1 versus a control population. Transplantation: It is accepted that in specific patients endometriosis can spread directly. Thus endometriosis 18 has been found in abdominal incisional scars after surgery for endometriosis. It can also grow invasively into different tissue layers, i.e., from thecul-de-sac into the vagina. On rare occasions endometriosis may be transplanted by blood or by the lymphatic system into peripheral organs such as the lungs and brain. 6. Immune system: Research is focusing on the possibility that the immune system may not be able to cope with the cyclic onslaught of retrograde menstrual fluid. In this context there is interest in studying the relationship of endometriosis toautoimmune disease, allergic reactions, and the impact of toxins. It is still unclear what, if any, causal relationship exists between toxins, autoimmune disease, and endometriosis. 7. Environment: There is a growing suspicion that environmental factors may cause endometriosis, specifically some plastics and cooking with certain types of plastic containers with microwave ovens. Other sources suggest that pesticides and hormones in our food cause a hormone imbalance. 8. Birth Defect: In rare cases where imperforate hymen does not resolve itself prior to the first menstrual cycle and goes undetected, blood and endometrium are trapped within the uterus of the patient until such time as the problem is resolved by surgical incision. Many health care practitioners never encounter this defect, and due to the flu-like symptoms it is often misdiagnosed or overlooked until multiple menstrual cycles have passed. By the time a correct diagnosis has been made, endometrium and other fluids have filled the uterus and fallopian tubes with results similar to retrograde menstruation resulting in endometriosis. The initial stage of endometriosis may vary based on the time elapsed between onset and surgical procedure. Cause of pain The way endometriosis causes pain is the subject of much research. Because many women with endometriosis feel pain during or around their periods and may spill further menstrual flow into the pelvis with each menstruation, some researchers are trying to reduce menstrual events in patients with endometriosis. Endometriosis lesions react to hormonal stimulation and may "bleed" at the time of menstruation. The blood accumulates locally, causes 19 swelling, and triggers inflammatory responses with the activation of cytokines. It is thought that this process may cause pain. Pain can also occur from adhesions (internal scar tissue) binding internal organs to each other, causing organ dislocation. Fallopian tubes, ovaries, the uterus, the bowels, and the bladder can be bound together in ways that are painful on a daily basis, not just during menstrual periods. Smoking Smokers tend to be at a lower risk for endometriosis. Smoking causes decreased estrogens with increased breakthrough bleeding and shortened luteal phases. Smokers have an earlier than normal (by about 1.5–3 years) menopause which suggests that there is some toxic effect of smoking on the follicles directly. Chemically, nicotine has been shown to concentrate in cervical mucous and metabolites have been found in follicular fluid and been associated with delayed follicular growth and maturation. Finally, there is some effect on tubal motility because smoking is associated with an increased incidence of ectopic pregnancy as well as an increased spontaneous abortion rate. Pregnancy Aging brings with it many effects that may reduce fertility. Depletion over time of ovarian follicles affects menstrual regularity. Endometriosis has more time to produce scarring of the ovary and tubes so they cannot move freely or it can even replace ovarian follicular tissue if ovarian endometriosis persists and grows. Leiomyomata (fibroids) can slowly grow and start causing endometrial bleeding that disrupts implantation sites or distorts the endometrial cavity which affects carrying a pregnancy in the very early stages. Abdominal adhesions from other intraabdominal surgery, or ruptured ovarian cysts can also affect tubal motility needed to sweep the ovary and gather an ovulated follicle (egg). Endometriosis in postmenopausal women does occur and has been described as an aggressive form of this disease characterized by complete progesterone resistance and extraordinarily high levels of aromatase expression. In less common cases, girls may have endometriosis symptoms before they even reach menarche. Co-morbidity 20 Endometriosis bears no relationship to endometrial cancer. Current research has demonstrated an association between endometriosis and certain types of cancers, notably ovarian cancer, non-Hodgkin's lymphoma and brain cancer. Endometriosis often also coexists with leiomyoma or adenomyosis, as well as autoimmune disorders. A 1988 survey conducted in the US found significantly more Hypothyroidism, fibromyalgia, chronic fatigue syndrome, autoimmune diseases, allergies and asthma in women with endometriosis compared to the general population. Complications Complications of endometriosis include: Internal scarring Adhesions Pelvic cysts Chocolate cyst of ovaries Ruptured cyst Blocked bowel/bowel obstruction Infertility can be related to scar formation and anatomical distortions due to the endometriosis; however, endometriosis may also interfere in more subtle ways: cytokines and other chemical agents may be released that interfere with reproduction. Other complications of endometriosis include bowel and ureteral obstruction resulting from pelvic adhesions. Also, peritonitis from bowel perforation can occur. 21 Ovarian endometriosis may complicate pregnancy by decidualization, abscess and/or rupture, It is the most common adnexal mass detected during pregnancy, being present in 0.52% of deliveries as studied in the period 2002 to 2007. Still, ovarian endometriosis during pregnancy can be safely observed conservatively. Diagnosis Micrograph showing endometriosis (right) and ovarian stroma (left). H&E stain. A health history and a physical examination can in many patients lead the physician to suspect endometriosis. Surgery is the gold standard in diagnosis. However, in the United States most insurance plans will not cover surgical diagnosis unless the patient has already attempted to become pregnant and failed. Use of imaging tests may identify endometriotic cysts or larger endometriotic areas. It also may identify free fluid often within the cul-de-sac. The two most common imaging tests are ultrasound and magnetic resonance imaging (MRI). Normal results on these tests do not eliminate the possibility of endometriosis. Areas of endometriosis are often too small to be seen by these tests. The only way to diagnose endometriosis is by laparoscopy or other types of surgery with lesion biopsy. The diagnosis is based on the characteristic appearance of the disease, and should be corroborated by a biopsy. Surgery for diagnoses also allows for surgical treatment of endometriosis at the same time. Although doctors can often feel the endometrial growths during a pelvic exam, and your symptoms may be telltale signs of endometriosis, diagnosis cannot be confirmed without performing a laparoscopic procedure. Often the symptoms of ovarian cancer are identical to those of endometriosis. If a misdiagnosis of endometriosis occurs due to failure to confirm diagnosis through laparoscopy, early diagnosis of ovarian cancer, which is crucial for successful treatment, may have been missed. Staging 22 possible locations of endometriosis Surgically, endometriosis can be staged I–IV (Revised Classification of the American Society of Reproductive Medicine). The process is a complex point system that assesses lesions and adhesions in the pelvic organs, but it is important to note staging assesses physical disease only, not the level of pain or infertility. A patient with Stage I endometriosis may have little disease and severe pain, while a patient with Stage IV endometriosis may have severe disease and no pain or vice versa. In principle the various stages show these findings: Stage I (Minimal) Findings restricted to only superficial lesions and possibly a few filmy adhesions Stage II (Mild) In addition, some deep lesions are present in the cul-de-sac Stage III (Moderate) As above, plus presence of endometriomas on the ovary and more adhesions Stage IV (Severe) As above, plus large endometriomas, extensive adhesions. Treatments While there is no cure for endometriosis, in many patients menopause (natural or surgical) will abate the process. In patients in the reproductive years, endometriosis is merely managed: the goal is to provide pain relief, to restrict progression of the process, and to restore or preserve fertility where needed. In younger women with unfulfilled 23 reproductive potential, surgical treatment attempts to remove endometrial tissue and preserving the ovaries without damaging normal tissue. In women who do not have need to maintain their reproductive potential, hysterectomy and/or removal of the ovaries may be an option; however, this will not guarantee that the endometriosis and/or the symptoms of endometriosis will not come back, and surgery may induce adhesions which can lead to complications. In general, the diagnose of endometriosis is confirmed during surgery, at which time ablative steps can be taken. Further steps depend on circumstances: patients without infertility can be managed with hormonal medication that suppress the natural cycle and pain medication, while infertile patients may be treated expectantly after surgery, with fertility medication, or with IVF. Sonography is a method to monitor recurrence of endometriomas during treatments. Treatments for endometriosis in women who do not wish to become pregnant include: Hormonal medication Progesterone or Progestins: Progesterone counteracts estrogen and inhibits the growth of the endometrium. Such therapy can reduce or eliminate menstruation in a controlled and reversible fashion. Progestins are chemical variants of natural progesterone. Avoiding products with xenoestrogens, which have a similar effect to naturally produced estrogen and can increase growth of the endometrium. Hormone contraception therapy: Oral contraceptives reduce the menstrual pain associated with endometriosis. They may function by reducing or eliminating menstrual flow and providing estrogen support. Typically, it is a long-term approach. Recently Seasonalewas FDA approved to reduce periods to 4 per year. Other OCPs have however been used like this off label for years. Continuous hormonal consists of the use of combined oral contraceptive pills without the use of placebo pills, or the use ofNuvaRing or the contraceptive patch without the break week. This eliminates monthly bleeding episodes. 24 Danazol (Danocrine) and gestrinone are suppressive steroids with some androgenic activity. Both agents inhibit the growth of endometriosis but their use remains limited as they may cause hirsutism and voice changes. Gonadotropin Releasing Hormone (GnRH) agonist: These agents work by increasing the levels of GnRH. Consistent stimulation of the GnRH receptors results in downregulation, inducing a profound hypoestrogenism by decreasing FSH and LH levels. While effective in some patients, they induce unpleasant menopausal symptoms, and over time may lead to osteoporosis. To counteract such side effects some estrogen may have to be given back (addback therapy). These drugs can only be used for six months at a time. Lupron depo shot is a GnRH agonist and is used to lower the hormone levels in the woman's body to prevent or reduce growth of endometriosis. The injection is given in 2 different doses a once a month for 3 month shot with the dosage of (11.25 mg) or a once a month for 6 month shot with the dosage of (3.75 mg) Aromatase inhibitors are medications that block the formation of estrogen and have become of interest for researchers who are treating endometriosis. Other medication NSAIDs Anti-inflammatory. They are commonly used in conjunction with other therapy. For more severe cases narcotic prescription drugs may be used. NSAID injections can be helpful for severe pain or if stomach pain prevents oral NSAID use. MST Morphine sulphate tablets and other opioid painkillers work by mimicking the action of naturally occurring pain-reducing chemicals called "endorphins". There are different long acting and short acting medications that can be used alone or in combination to provide appropriate pain control. Diclofenac in suppository or pill form. Taken to reduce inflammation and as an analgesic reducing pain. Surgery Procedures are classified as 25 conservative when reproductive organs are retained, semi-conservative when ovarian function is allowed to continue, and radical when the uterus and ovaries are removed. Conservative therapy consists of removal, excision (called cystectomy) or ablation of endometriosis, adhesions, resection of endometriomas, and restoration of normal pelvic anatomy as much as is possible. There are combinations as well, notably one consisting of cystectomy followed by ablative surgery using a CO2 laser to vaporize the remaining 10%–20% of the endometrioma wall close to the hilus. Radical therapy in endometriosis removes the uterus (hysterectomy) and tubes and ovaries (bilateral salpingo-oophorectomy) and thus the chance for reproduction. Radical surgery is generally reserved for women with chronic pelvic pain that is disabling and treatmentresistant. Not all patients with radical surgery will become pain-free. Semi-conservative therapy preserves a healthy appearing ovary, and yet, it also increases the risk of recurrence. For patients with extreme pain, a presacral neurectomy may be indicated where the nerves to the uterus are cut. However, strong clinical evidence showed that presacral neurectomy is more effective in pain relief if the pelvic pain is midline concentrated, and not as effective if the pain extends to the left and right lower quadrants of the abdomen. This is due to the fact that the nerves to be transected in the procedure are innervating the central or the midline region in the female pelvis. Furthermore, women who had presacral neurectomy have higher prevalence of chronic constipation not responding well to medication treatment because of the potential injury to the parasympathetic nerve in the vicinity during the procedure. Comparison of medicinal and surgical interventions Efficacy studies show that both medicinal and surgical interventions produce roughly equivalent pain-relief benefits. Recurrence of pain was found to be 44 and 53 percent with medicinal and surgical interventions, respectively. However, each approach has its own advantages and disadvantages. Advantages of medicinal interventions 1. Decrease initial cost 2. Empirical therapy (i.e. Can be easily modified as needed) 26 3. Effective for pain control Disadvantages of medicinal interventions 1. Adverse effects are common 2. Not likely to improve fertility 3. Some can only be used for limited periods of time Advantages of surgery 1. Has significant efficacy for pain control. Has increased efficacy over medicinal intervention for infertility treatment 2. Combined with biopsy, it is the only way to achieve a definitive diagnosis 3. Can often be carried out as a minimal invasive (laparoscopic) procedure to reduce morbidity and minimalize the risk of postoperative adhesions Disadvantages of surgery 1. Cost 2. Risks are "poorly defined... and probably underestimated." In one study, 3-10% experienced major complications from surgery. 3. Efficacy is questionable. In the same study, substantial short-term pain relief was experienced by approximately 70-80% of the subjects. However, at 1 year follow-up, approximately 50% of the subjects needed analgesics or hormonal treatments Treatment of infertility While roughly similar to medicinal interventions in treating pain, the efficacy of surgery is especially significant in treating infertility. One study has shown that surgical treatment of endometriosis approximately doubles the fecundity (pregnancy rate). The use of medical suppression after surgery for minimal/mild endometriosis has not shown benefits for patients with infertility Use of fertility medication that stimulates ovulation (clomiphene citrate, gonadotropins) combined with intrauterine insemination (IUI) enhances fertility in these patients. In-vitro fertilization (IVF) procedures are effective in improving fertility in many women with endometriosis. IVF makes it possible to combine sperm and eggs in a laboratory and then place the resulting embryos into the woman's uterus. The decision when to apply IVF in endometriosis-associated infertility takes into account the age of the 27 patient, the severity of the endometriosis, the presence of other infertility factors, and the results and duration of past treatments. Other treatments One theory above suggests that endometriosis is an auto-immune condition and if the immune system is compromised with a food intolerance, then removing that food from the diet can, in some people, have an effect. Common intolerances in people with endometriosis are wheat, sugar, meat and dairy Avoiding foods high in hormones and inflammatory fats also appears to be important in endometriosis pain management. Eating foods high in indole-3carbinol, such as cruciferous vegetables appears to be helpful in balancing hormones and managing pain, as do omega 3 fatty acids, particularly EPA. The use of soy has been reported to both alleviate pain and to aggravate symptoms, making its use questionable. Physical therapy for pain management in endometriosis has been investigated in a pilot study suggesting possible benefit. Physical exertion such as lifting, prolonged standing or running does exacerbate pelvic pain. Use of heating pads on the lower back area, may provide some temporary relief. Laboratory studies indicate that heparin may alleviate endometriosis-associated fibrosis. Prognosis Proper counseling of patients with endometriosis requires attention to several aspects of the disorder. Of primary importance is the initial operative staging of the disease to obtain adequate information on which to base future decisions about therapy. The patient's symptoms and desire for childbearing dictate appropriate therapy. Not all therapy works for all patients. Some patients have recurrences after surgery or pseudo-menopause. In most cases, treatment will give patients significant relief from pelvic pain and assist them in achieving pregnancy. It is important for patients to be continually in contact with their physician and keep an open dialog throughout treatment. This is a disease without a cure but with the proper communication, a woman with endometriosis can attempt to live a normal, functioning life. Using cystectomy and ablative surgery, pregnancy rates are approximately 40%. Recurrence 28 The underlying process that causes endometriosis may not cease after surgical or medical intervention, and the annual recurrence rate is given as 5–20 % per year reaching eventually about 40% unless hysterectomy is performed or menopause reached, Monitoring of patients consists of periodic clinical examinations and sonography. Also, the CA 125 serum antigen levels have been used to follow patients with endometriosis. With combined cystectomy and ablative surgery, one study showed recurrence of a small endometrioma in only one case among fifty-two women (2%) at a mean follow-up of 8.3 months. Vaginal parturition decreases recurrence of endometriosis. In contrast, endometriosis recurrence rates have been shown to be higher in women who do not have vaginal parturition, such as in Cesarean section. Sexually Transmitted Diseases Overview (STDs) -Sexually transmitted diseases (STDs, venereal diseases) are among the most common infectious diseases in the United States today. STDs are sometimes referred to as sexually transmitted infections, since these conditions involve the transmission of an infectious organism between sex partners. More than 20 different STDs have been identified, and about 19 million men and women are infected each year in the United States, according to the CDC (2010). -Depending on the disease, the infection can be spread through any type of sexual activity involving the sex organs, the anus, or the mouth; an infection can also be spread through contact with blood during sexual activity. STDs are infrequently transmitted by any other type of contact (blood, body fluids or tissue removed from an STD infected person and placed in contact with an uninfected person); however, people that share unsterilized needles markedly increase the chance to pass many diseases, including STD's (especially hepatitis B), to others. Some diseases are not considered to be officially an STD (for example, hepatitis types A, C, E) but are infrequently noted to be transferred during sexual activity. Consequently, some authors include them as STD's, others do not. Consequently, lists of STD's can vary, depending on whether the STD is usually transmitted by sexual contact or only infrequently transmitted. 29 in women (for example, Chlamydia, genital herpes or gonorrhea). This can also occur in some men. -term consequences from STDs tend to be more severe for women than for men. Some STDs can cause pelvic infections such as pelvic inflammatory disease (PID), which may cause a tubo-ovarian abscess. The abscess, in turn, may lead to scarring of the reproductive organs, which can result in an ectopic pregnancy (a pregnancy outside the uterus), infertility or even death for a woman. Human papillomavirus infection (HPV infection), an STD, is a known cause of cancer of the cervix. an be passed from a mother to her baby before, during, or immediately after birth. person often obtains more than one pathogenic organism at a time. For example, many people (about 50%) are infected at a single sexual contact with both gonorrhea and Chlamydia. STDs caused by bacteria Chancroid (Haemophilus ducreyi) Chlamydia (Chlamydia trachomatis) Gonorrhea (Neisseria gonorrhea) Granuloma inguinale (Calymmatobacterium granulomatis) Lymphogranuloma venereum (Chlamydia trachomatis) Syphilis (Treponema pallidum) STDs caused by viruses Genital herpes (herpes simplex virus) Genital warts (human papillomavirus virus [HPV]) Hepatitis B and D, and infrequently, A*,C*,E* (hepatitis viruses, types A-E) HIV/AIDS (human immunodeficiency virus [HIV virus]) Molluscum contagiosum* (poxvirus) STD caused by protozoan 30 Trichomoniasis (Trichomonas vaginalis) STD's* caused by fungi Jock itch (Tenia cruris)* Yeast infections* (Candida albicans) STD's caused by parasites Pubic lice or crabs (Pediculosis pubis) Scabies* Sarcoptes scabiei For details about the pathogens that cause the diseases, the reader is urged to search the specific disease by simply clicking on it. Trichomoniasis, common cause of vaginitis. It is a sexually transmitted disease, and is caused by the single-celled protozoan parasite Trichomonas vaginalis producing mechanical stress on host cells and then ingesting cell fragments after cell death.[1] Trichomoniasis is primarily an infection of the urogenital tract; the most common site of infection is the urethra and the vagina in women. Symptoms Typically, only women experience symptoms associated with Trichomonas infection. Symptoms include inflammation of the cervix (cervicitis), urethra (urethritis), and vagina (vaginitis) which produce an itching or burning sensation. Discomfort may increase during intercourse and urination. There may also be a yellow-green, itchy, frothy foul-smelling ("fishy" smell) vaginal discharge. In rare cases, lower abdominal pain can occur. Symptoms usually appear in women within 5 to 28 days of exposure. In many cases, men may hold the parasite for some years without any signs (dormant). Some sexual health specialists have stated that the condition can probably be carried in the vagina for years, despite standard tests being negative . While symptoms are most common in women, some men may temporarily exhibit symptoms such as an irritation inside the penis, mild discharge, or slight burning after urination or ejaculation Diagnosis Trichomoniasis is diagnosed by visually observing the trichomonads via a microscope. In women, the examiner collects the specimen during a pelvic examination by inserting a speculum into the vagina and then using a cotton-tipped applicator to collect the sample. 31 Treatment Treatment for both pregnant and non-pregnant patients usually utilizes metronidazole (Flagyl) but with caution especially in early stages of pregnancy Complications Research has shown a link between trichomoniasis and two serious sequelæ. Data suggest that: Trichomoniasis is associated with increased risk of transmission of HIV. Trichomoniasis may cause a woman to deliver a low-birth-weight or premature infant. Trichomoniasis is also associated with increased chances of cervical cancer Evidence implies that infection in males potentially raises the risks of prostate cancer Prevention Because trichomoniasis is a sexually transmitted disease, abstinence is the preferred method to avoid contraction of this disease. Safe sex and hygiene practices may also help prevent trichomonas infection. Wear condoms. Wash before and after intercourse. Don't share swimsuits or towels. (Trichomonads survive for up to 45 minutes outside the body.) Shower immediately after swimming in a public pool. urinary incontinence -this embarrassing little problem is urinary incontinence, and lots of women -- regardless of age -- are secretly dealing with it. More than 13 million Americans have incontinence, and women are twice as likely to have it as men, according the Agency for Healthcare Research and Quality. About 25% to 45% of women suffer from urinary incontinence, defined as leakage at least once in the past year. The rates of urinary incontinence increase with age: 20%-30% of young women , 30%-40% of middle-aged women, and up to 50% of older women suffer from urinary incontinence. -"It's embarrassing, and it can really affect your quality of life - your emotional state, body, sexuality," Yet many put up with incontinence 32 needlessly, Brubaker tells WebMD. "People don't realize it's a medical condition, and that there's help. Many women think it's normal, part of having children or going into menopause." Though incontinence is "more common than you might think," it's not normal says Brubaker, who sees teens, and women in their 20s, 30s, or older with this issue. "You don't have to put up with it. There are often simple solutions that work." Understanding Urinary Incontinence in Women 4 Types of Urinary Incontinence When you can't control the release of your urine, you have urinary incontinence. For some the problem can be as minor as the rare dribble, for others as problematic as wetting your clothes. There are four kinds of these plumbing problems, according to the Mayo Clinic: Stress incontinence is that little leak that happens when you cough, laugh, sneeze -- any motion that stresses or puts too much pressure on the bladder. Stress incontinence can result from pregnancy and childbirth, when pelvic muscles and tissues can get stretched and damaged. It can also occur from high-impact sports, as a result of aging, or from being overweight. Urge incontinence aka "overactive bladder," is a bit different - it's the urgent need to go, followed by an involuntary loss of urine -- with anything from a few seconds to a minute's warning. It is thought to be due to spasms of the bladder muscles. Conditions such as multiple sclerosis, Parkinson's disease, or a urinary tract infection can cause urge incontinence. Mixed incontinence means you have more than one type of incontinence, with stress and urge incontinence being the typical mix. "I think most women have both types," adds Brubaker. "I don't believe there's as much distinction between the two types as we might think." Overflow incontinence . If you can't empty your bladder every time you go to the bathroom and experience a frequent or constant dribbling of urine, you have overflow incontinence. Certain medications can cause this problem, and people with nerve damage from diabetes or men with prostate issues can also experience this type of incontinence. It is due to impaired bladder muscle contractions or bladder obstructions. 33 If you think urinary incontinence only affects older women, think again. Bladder control issues affect younger, active women, too -- are you one of them? Incontinence a Big Problem for Young Women -Among teens and young women, incontinence problems are typically related to sports injuries" Women in high-impact sports are at highest risk -- parachuters, gymnasts, runners," "In these sports, you're hitting the ground hard, which can damage pelvic muscles and connective tissue that support the bladder." -Many young women have pre-existing biological reasons putting them at higher risk, "It runs in families," . "Just as bad eyesight runs in families, so can weak pelvic muscles. It's not that they've been overdoing it with exercise. It's just that they've reached the tolerance of their own tissues." -For these girls and women, simply wearing a tampon or pessary -- a device similar to a diaphragm -- during exercise is a good solution,. "They just need a little something to support those pelvic tissues, something to put pressure on the urethra." Coping With Incontinence: Lifestyle Changes -But for most women, a little absorbent pad is their first weapon, a lifestyle change their second. -For many women the change may be as simple as drinking less water. "You can't drink two big bottles of water at one time, because it comes through your system as one big [wave] of fluid," "If you have a little at a time, it's much easier for the bladder." -"Also, caffeine is a diuretic, so Cokes, coffee, any drink with caffeine make you leak more," . Perhaps you just need to urinate more frequently - especially before getting onto the tennis court, for example. -You may also simply learn to brace yourself when you laugh or cough, tightening your pelvic muscles to prevent leaks. "Women are smart...". "They try a bunch of things on their own before they get the gumption to talk to someone about it." Incontinence Treatments -When basic changes aren't enough, several treatments are available. "Start with the most conservative, least-expensive treatment," Options include: Muscle training: -For stress incontinence, learning muscle control can help manage leakage. That means regularly practicing pelvic muscle (Kegel) exercises. "You learn to feel the muscle that controls the bladder, and build strength in that muscle," says . "If you're going to play tennis, and it's your backhand that makes you leak, you learn to tighten those muscles at that instant." 34 -There's also a traditional Chinese therapy involving vaginal weights, which Galloway says are very effective. Related to Incontinence & Overactive Bladder America Asks About OAB Bladder Control Diabetes Menopause Multiple Sclerosis Parkinson’s Disease Side Effects of Diuretics Common Treatments for Incontinence & Overactive Bladder Biofeedback Bladder Surgery Detrol Ditropan Enablex Flomax Kegel Exercises More Drugs Pessary Incontinence Treatments -"They are a means to strengthen muscles in the pelvis that control urination. The patient puts the egg in her vagina, and works to hold it there without dropping it," he says. "As her pelvic muscles strengthen, she uses a heavier weight to increase that strength." -Bladder training: By lengthening the time between trips to the bathroom, bladder training can help women with urge incontinence. -You start by urinating frequently -- every 30 minutes or so -- and increasing the time gradually until you're going every three to four hours. -Relaxation exercises -- breathing slowly and deeply when the urge strikes -- may also help. Once the urge passes, wait five minutes and go to the bathroom even if you don't feel like you need to anymore. Slowly increase the amount of waiting time. -Electrical stimulation: This can be used to strengthen muscles with stress incontinence or calm overactive muscles with urge incontinence. -A small probe inserted in the vagina gives quick doses of electrical stimulation to the vaginal wall, Brubaker explains. "It has the same effect as Kegel exercises... and it works as well as medication but without side effects." 35 -Biofeedback: This involves becoming attuned to your body's functioning, to gain control over muscles to suppress urges. -Biofeedback typically involves wearing sensors to track certain bodily functions such as muscle tension, then learning how to control those functions. It can be very effective in controlling bladder muscles, says Brubaker. -Hormone Creams: Estrogen creams are intended to restore the tissue of the vagina and urethra to their normal thickness, says Galloway - but they don't really help incontinence. -"Hormone creams are more effective with vaginal dryness than they are with resolving incontinence," he tells WebMD. "Some [studies] demonstrate significant improvements using hormone creams and others have not shown a benefit." -Bladder Training With Scheduled Toilet Trips: With this technique the clock dictates your toilet visits, not your bladder. Using this method you take routine, planned bathroom trips, usually every two to four hours. -Implants: When collagen or other materials are injected into tissues around the urethra, it provides pressure that helps prevent leakage. "These injectables have significantly lower side effects and complications compared to medications," Brubaker explains. "The injection needs to be repeated every 12 to 18 months. Some insurance covers injectables, depending on the material used." -Medications: No drug helps with stress incontinence, but a class called anticholinergics does help with urge incontinence. These drugs include Detrol, Oxytrol, , all with similar effectiveness and similar side effects, like dry mouth and constipation A transdermal patch called Oxytrol has also been effective, , who adds that skin irritation at the patch site does occur in some patients. -Surgery: There are 300 surgical options to treat incontinence. -"The hard part is picking the surgery that has the best chance of working well for that woman long-term," he says. "Surgery can create problems. It can cause difficulty in urinating, worsen an urge incontinence problem, or it can do nothing to solve the problem." -A large NIH study is examining the use of a sling -- a medical device that is surgically inserted into the vagina and positioned underneath the urethra, says Brubaker. -"It helps the urethral sphincter remain closed when abdominal pressure tries to open it. At least, we think that's how it works," he says. "We have only five-year outcomes on one group of these devices. But they look promising." -"Before having any surgery, ask your doctor for names of other patients who have had the procedure in question," says Galloway. 36 -"Talk to them, find out how it worked. You'll be in a much better position to decide what to do." Pelvic inflammatory disease: - (PID) is a generic term for inflammation of the uterus, fallopian tubes, and/or ovaries as it progresses to scar formation with adhesions to nearby tissues and organs. -This may lead to infections. PID is a vague term and can refer to viral, fungal, parasitic, though most often bacterial infections. PID should be classified by affected organs, the stage of the infection, and the organism(s) causing it. Although an STI is often the cause, many other routes are possible, including lymphatic, postpartum, postabortal(either miscarriage or abortion) or intrauterine device (IUD) related, and hematogenous spread. Two thirds of patients with laparoscopic evidence of previous PID were not aware they had PID. Epidemiology In the United States, more than a million women are affected by PID each month, and the rate is highest with teenagers and first time mothers. PID causes over 100,000 women to become infertile in the US each year. N. gonorrhea is isolated in 40-60% of women with acute salpingitis. trachomatis is estimated to be the cause in about 60% of cases of salpingitis, which may lead to PID. However, not all PID is caused solely by STIs; organisms that are considered normal vaginal flora can be involved, and individual cases of PID can be due to either a single organism or a co-infection of many different species. 10% of women in one study had asymptomatic Chlamydia trachomatis infection and 65% had asymptomatic infection with Neisseria gonorrhoeae. It was noted in one study that 10-40% of untreated women with N. gonorrhoea develop PID and 20-40% of women infected with C. trachomitis developed PID. PID is the leading cause of infertility. "A single episode of PID results in infertility in 13% of women, This rate of 37 infertility increases with each infection. Diagnosis Symptoms in PID range from sub clinical (asymptomatic) to severe. If there are symptoms then fever, cervical motion tenderness, lower abdominal, new or different discharge, painful intercourse, or irregular menstrual bleeding may be noted. It is important to note that even asymptomatic PID can and does cause serious harm. Laparoscopic identification is helpful in diagnosing tubal disease, 6590% positive predictive value in patients with presumed PID. Regular Sexually Transmitted Infection (STI) testing is important for prevention. Treatment is usually started empirically because of the serious complications that may result from delayed treatment. Definitive criteria include:histopathologic evidence of endometritis, thickened filled fallopian tubes, or laparoscopic findings. Gram-stain/smear becomes important in identification of rare and possibly more serious organisms. Differential diagnosis; -Appendicitis, ectopic pregnancy, septic abortion, hemorrhagic or ruptured ovarian cysts or tumors, twisted ovarian cyst, degeneration of amyoma, and acute enteritis must be considered. Pelvic inflammatory disease is more likely to occur when there is a history of pelvic inflammatory disease, recent sexual contact, recent onset of menses, or an IUD in place or if the partner has a sexually transmitted infection. -Acute pelvic inflammatory disease is highly unlikely when recent intercourse has not taken place or an IUD is not being used. A sensitive serum pregnancy test should be obtained to rule out ectopic pregnancy. Culdocentesis will differentiate hem peritoneum (ruptured ectopic pregnancy or hemorrhagic cyst) from pelvic sepsis (salpingitis, ruptured pelvic abscess, or ruptured appendix). -Pelvic and vaginal ultrasounds are helpful in the differential diagnosis of ectopic pregnancy of over six weeks. Laparoscopy is often utilized to diagnose pelvic inflammatory disease, and it is imperative if the diagnosis is not certain or if the patient has not responded to antibiotic therapy after 48 hours. 38 -Although the PID infection itself may be cured, effects of the infection may be permanent. This makes early identification by someone who can prescribe appropriate curative treatment very important in the prevention of damage to the reproductive system. Since early gonococcal infection may be asymptomatic, regular screening of individuals at risk for common agents (history of multiple partners, history of any unprotected sex, or people with symptoms) or because of certain procedures (post pelvic operation, postpartum, miscarriage or abortion). Prevention is also very important in maintaining viable reproduction capabilities. -If the initial infection is mostly in the lower tract, after treatment the person may have few difficulties. If the infection is in the fallopian tubes or ovaries, more serious complications are more likely to occur. Complications; -PID can cause scarring inside the reproductive organs, which can later cause serious complications, including chronic pelvic pain, infertility,ectopic pregnancy (the leading cause of pregnancyrelated deaths in adult females), and other dangerous complications of pregnancy. Occasionally, the infection can spread to in the peritoneum causing inflammation and the formation of scar tissue on the external surface of the liver (Fitz-Hugh-Curtis syndrome). Multiple infections and infections that are treated later are more likely to result in complications. -Fertility may be restored in women affected by PID. Traditionally tuboplastic surgery was the main approach to correct tubal obstruction or adhesion formation, however success rates tended to be very limited. In vitro fertilization (IVF) has been used to bypass tubal problems and has become the main treatment for patients who want to become pregnant. Treatment: -Treatment depends on the cause and generally involves use of antibiotic therapy. If the patient has not improved within two to three days after beginning treatment with the antibiotics, they should return to the hospital for further treatment. Drugs should also be given orally 39 and/or intravenously to the patient while in the hospital to begin treatment immediately, and to increase the effectiveness of antibiotic treatment. Hospitalization may be necessary if the patient has Tuboovarian abscesses; is very ill, immunodeficient, pregnant, or incompetent; or because a life-threatening condition cannot be ruled out. Treating partners for STIs is a very important part of treatment and prevention. Anyone with PID and partners of patients with PID since six months prior to -diagnosis should be treated to prevent reinfection. Psychotherapy is highly recommended to women diagnosed with PID as the fear of redeveloping the disease after being cured may exist. It is important for a patient to communicate any issues and/or uncertainties they may have to a doctor, especially a specialist such as a gynecologist, and in doing so, to seek follow-up care. -A systematic review of the literature related to PID treatment was performed prior to the 2006 CDC sexually transmitted infections treatment guidelines. Strong evidence suggests that neither site nor route of antibiotic administration affects the short or long-term major outcome of women with mild or moderate disease. Data on women with severe disease was inadequate to influence the results of the study. -Regimens :include cefoxitin or cefotetan plus, doxycycline, clindamycin plus, gent amicin, ampicillin and sulbactam plus doxycycline, andceftriaxone or cefoxitin plus doxycycline. Prevention; Risk reduction against sexually transmitted infections through barrier methods such as condoms or abstinence; see human sexual behavior for other listings. Going to the doctor immediately if symptoms of PID, sexually transmitted infections appear, or after learning that a current or former sex partner has, or might have had a sexually transmitted infection. Getting regular gynecological (pelvic) exams with STI testing to screen for symptom less PID. 40 Discussing sexual history with a trusted physician in order to get properly screened for sexually transmitted diseases. Regularly scheduling STI testing with a physician and discussing which tests will be performed that session. Getting a STI history from your current partner and insisting they be tested and treated before intercourse. Understanding when a partner says that they have been STI tested they usually mean Chlamydia and gonorrhea in the US, but that those are not all of the sexually transmissible infections. Treating partners to prevent reinfection or spreading the infection to other people. Diligence in avoiding vaginal activity, particularly intercourse, after the end of a pregnancy (delivery, miscarriage, or abortion) or certain gynecological procedures, to ensure that the cervix closes. Salpingitis, any inflammation of the fallopian tubes Tubo-ovarian abscess an abscess of the fallopian tube and ovary Endometritis Pelvic peritonitis -An ovarian cyst: - is any collection of fluid, surrounded by a very thin wall, within an ovary. -Any ovarian that is larger than about two centimeters is termed an ovarian cyst. An ovarian cyst can be as small, or large. -Most ovarian cysts are functional in nature, and harmless (benign) In the US, ovarian cysts are found in nearly all premenopausal women, and in up to 14.8% of postmenopausal women. -Ovarian cysts affect women of all ages. 41 - They occur most often, however, during a woman's childbearing years. -Some ovarian cysts cause problems, such as bleeding and pain. - Surgery may be required to remove cysts larger than 5 centimeters in diameter. Classification: Non-functional cysts There are several other conditions affecting the ovary that are described as types of cysts, but are not usually grouped with the functional cysts. (Some of these are more commonly or more properly known by other names.) These include: Dermoid cyst Chocolate cyst of ovary: An endometrioma, endometrioid cyst, endometrial cyst, or chocolate cyst is caused by endometriosis, and formed when a tiny patch of endometrial tissue (the mucous membrane that makes up the inner layer of the uterine wall) bleeds, sloughs off, becomes transplanted, and grows and enlarges inside the ovaries. A polycystic-appearing ovary is diagnosed based on its enlarged size — usually twice normal —with small cysts present around the outside of the ovary. It can be found in "normal" women, and in women with endocrine disorders. An ultrasound is used to view the ovary in diagnosing the condition. Polycysticappearing ovary is different from the polycystic ovarian syndrome, which includes other symptoms in addition to the presence of ovarian cysts. Signs and symptoms: 42 Some or all of the following symptoms may be present, though it is possible not to experience any symptoms: Dull aching, or severe, sudden, and sharp pain or discomfort in the lower abdomen (one or both sides), pelvis, vagina, lower back, or thighs; pain may be constant or intermittent— this is the most common symptom Fullness, heaviness, pressure, swelling, or bloating in the abdomen Breast tenderness Pain during or shortly after beginning or end of menstrual period. Irregular periods, or abnormal uterine bleeding or spotting Change in frequency or ease of urination (such as inability to fully empty the bladder), or difficulty with bowel movements due to pressure on adjacent pelvic anatomy Weight gain Nausea or vomiting Fatigue Infertility Increased level of hair growth Increased facial hair or body hair Headaches Strange pains in ribs, which feel muscular Bloating Strange nodules that feel like bruises under the layer of skin Diagnosis Ovarian cysts are usually diagnosed by either ultrasound or CT scan. treatment -About 95% of ovarian cysts are benign, meaning they are not cancerous. 43 -Treatment for cysts depends on the size of the cyst and symptoms. For small, asymptomatic cysts, the wait and see approach with regular check-ups will most likely be recommended. Pain caused by ovarian cysts may be treated with: pain relievers, including acetaminophen/paracetamol (Tylenol), no steroidal anti-inflammatory drugs such as ibuprofen (Motrin, Advil), or narcotic pain medicine (by prescription) may help reduce pelvic pain. NSAIDs usually work best when taken at the first signs of the pain. a warm bath, or heating pad, or hot water bottle applied to the lower abdomen near the ovaries can relax tense muscles and relieve cramping, lessen discomfort, and stimulate circulation and healing in the ovaries. combined methods of hormonal contraception such as the combined oral contraceptive pill – the hormones in the pills may regulate the menstrual cycle, prevent the formation of follicles that can turn into cysts, and possibly shrink an existing cyst. -Also, limiting strenuous activity may reduce the risk of cyst rupture or torsion. -Cysts that persist beyond two or three menstrual cycles, or occur in post-menopausal women, may indicate more serious disease and should be investigated -through ultrasonography and laparoscopy, especially in cases where family members have had ovarian cancer. Such cysts may require surgical biopsy. Additionally, a blood test may be taken before surgery to check for elevated CA-125, a tumor marker, which is often found in increased levels in ovarian cancer, although it can also be elevated by other conditions resulting in a large number of false positives. -For more serious cases where cysts are large and persisting, doctors may suggest surgery. 44 - Some surgeries can be performed to successfully remove the cyst(s) without hurting the ovaries, while others may require removal of one or both ovaries. -Ovarian cysts are fluid-filled sacs, similar to blisters, that are common among women during their reproductive years. They form on the ovaries, the almond-sized organs on each side of the uterus. Most types of ovarian cysts are harmless and go away without any treatment. What Causes Ovarian Cysts? The normal function of the ovaries is to produce an egg each month. During the process of ovulation, a cyst-like structure called a follicle is formed inside the ovary. The mature follicle ruptures when an egg is released during ovulation. A corpus luteum forms from the empty follicle, and if pregnancy does not occur, the corpus luteum dissolves. Sometimes, however, this process does not conclude appropriately, causing the most common type of ovarian cyst -- functional ovarian cysts. Abnormal ovarian cysts, such as polycystic ovarian disease, may occur as the result of an imbalance of female hormones (estrogen and progesterone). Types of Ovarian Cysts 45 Functional Cysts These normal cysts will often shrink and disappear within two or three menstrual cycles. Because this type of cyst is formed during ovulation, it rarely occurs in menopausal women because eggs are no longer being produced. Dermoid Cysts These are ovarian cysts that are filled with various types of tissues, including hair and skin. Endometrioma Cysts These cysts are also known as the "chocolate cysts" of endometriosis, and they form when tissue similar to the lining of the uterus attaches to the ovaries. Cyst adenoma Cysts These are ovarian cysts that develop from cells on the outer surface of the ovaries. Polycystic Ovarian Disease This disease refers to cysts that form from a build up of follicles. These cysts cause the ovaries to enlarge and create a thick outer covering, which may prevent ovulation from occurring, and are often the cause of fertility problems. What are the Symptoms of Ovarian Cysts? Ovarian cysts often cause no symptoms; however, when symptoms are present, ovarian cysts may cause a dull ache or a sense of fullness or pressure in the abdomen. Pain during intercourse and at other times can also indicate the presence of ovarian cysts. Pain or pressure is caused by a number of factors, such as size, bleeding or bursting of a cyst, which irritates the abdominal tissues. Pain can also be caused when a cyst is twisted (called torsion), which can block the flow of blood to the cyst. Other possible symptoms of ovarian cysts include delayed, irregular, or unusually painful periods. If you experience any of these symptoms, notify your doctor as soon as possible. How are Ovarian Cysts Diagnosed? Unless symptoms are present, ovarian cysts are typically diagnosed during an annual pelvic examination. Other diagnostic tests, such as ultrasound and laparoscopy, may be done if your physician detects any abnormalities. What are the Treatments for Ovarian Cysts? Treatment of ovarian cysts depends on several factors, including: the size and type of cyst the woman's age and general health her future pregnancy plans what symptoms she is experiencing -The earlier ovarian cysts are found, the less invasive the treatment. -Often, young women who are not experiencing any symptoms are advised to wait two or three months to see if the cysts dissolve on their own. In most cases, functional ovarian cysts will dissolve without any medical intervention or treatment. -Occasionally, physicians opt to prescribe oral contraceptives or hormones to shrink functional ovarian cysts. (Functional cysts are rare in women who use oral contraceptives since this method of birth control prevents ovulation.) Oral contraceptives are not an effective treatment for other types of benign ovarian cysts, but they do offer some protection against malignant ovarian cysts (ovarian cancer). Surgery is sometimes necessary to treat ovarian cysts that are unresponsive to hormonal treatment. Cases that could require surgery 46 include ovarian cysts that do not disappear after a few menstrual cycles and extremely large cysts. Ovarian cysts that are found in post menopausal women, cause symptoms such as severe pain or bleeding, or have become twisted often require a surgical procedure. The specific surgical procedure required depends on a number of factors, but typically the earlier ovarian cysts are discovered, the less extensive the surgery. Surgery can involve anything from simply removing the cyst to removing the ovary. In some severe cases, hysterectomy is recommended. Although your physician will discuss the planned procedure with you, you should keep in mind that the exact extent of the surgery may be unknown until the operation is in progress. -Things to Remember About Ovarian Cysts Because ovarian cysts often cause no symptoms, it is especially important for women who have previously had cysts to have regular pelvic examinations. Women who have previously had ovarian cysts are at a greater risk of developing further cysts. In addition, endometriosis may be worsened by the presence of ovarian cysts, and your chance of needing to have your ovaries removed increases. In the unusual case of malignant ovarian cysts, early treatment offers the best hope for recovery. Women who develop ovarian cysts after menopause are more likely to have malignancies. Remember, if you experience any fullness, pressure, or discomfort in your pelvic region phone your physician immediately for his advice. The earlier ovarian cysts are discovered and treated, the better your chance of complete recovery. Polycystic Ovary Syndrome (PCOS) - is one of the most common female endocrine disorders affecting approximately 5%-10% of women of reproductive age (12–45 years old) and is thought to be one of the leading causes of female infertility. The exact cause of polycystic ovary syndrome is unknown. -PCOS can present in any age during the reproductive years. Due to its often vague presentation it can take years to reach a diagnosis. Symptoms:Signs and symptoms vary from person to person, in both type and severity. 47 *Menstrual abnormality This is the most common characteristic. Examples of menstrual abnormality include Oligomenorrhea, amenorrhea — irregular, few, or absent menstrual periods *Excess androgen Elevated levels of male hormones (androgens) may result in physical signs, such as excess facial and body hair (hirsutism); adult acne or severe adolescent acne . *Polycystic ovaries Enlarged ovaries containing numerous small cysts can be detected by ultrasound. Despite the condition's name, polycystic ovaries alone do not confirm the diagnosis. To be diagnosed with PCOS, you must also have abnormal menstrual cycles or signs of androgen excess. *Infertility Women with polycystic ovary syndrome may have trouble becoming pregnant because they experience infrequent ovulation or a lack of ovulation. PCOS is the most common cause of female infertility. *Obesity About half the women with polycystic ovary syndrome are obese women with PCOS are more likely to be overweight or obese. *type 2 diabetes. Many women with polycystic ovary syndrome are insulin resistant, which impairs the body's ability to use insulin effectively to regulate blood sugar. This can result in high blood sugar and type 2 diabetes. *Acanthosis Nigerians. This is the medical term for darkened, velvety skin on the nape of your neck, armpits, inner thighs, vulva or under your breasts. This skin condition is a sign of insulin resistance. Causes:The exact cause of polycystic ovary syndrome is unknown. -normal reproductive cycle is regulated by changing levels of hormones produced by the pituitary gland in brain and by ovaries. The pituitary gland produces follicle-stimulating hormone (FSH) and luteinizing hormone (LH), which control the growth and release of eggs (ovulation) in the ovaries. During a monthly cycle, ovulation occurs about two weeks before period. ovaries secrete the hormones estrogen and progesterone, which prepare the lining of the uterus to receive a fertilized egg. The ovaries also produce some male hormones (androgens), such as testosterone. If pregnancy doesn't occur, estrogen and progesterone secretion decline and the lining of the uterus is shed during menstruation. -In polycystic ovary syndrome, the pituitary gland may secrete high levels of LH and the ovaries may make excess androgens. This disrupts 48 the normal menstrual cycle and may lead to infertility, excess body hair and acne. these factors likely play a role: Excess insulin. Insulin is the hormone produced in the pancreas that allows cells to use sugar (glucose), your body's primary energy supply. If you have insulin resistance, your ability to use insulin effectively is impaired, and your pancreas has to secrete more insulin to make glucose available to cells. The excess insulin is thought to boost androgen production by your ovaries. Low-grade inflammation. body's white blood cells produce substances to fight infection in a process called inflammation. Eating certain foods can trigger an inflammatory response in some predisposed people. When this happens, white blood cells produce substances that can lead to insulin resistance and cholesterol accumulation in blood vessels (atherosclerosis). Atherosclerosis causes cardiovascular disease. Research has shown that women with PCOS have low-grade inflammation. Heredity. If mother or sister has PCOS, you might have a greater chance of having it. Abnormal fetal development. New research shows that excessive exposure to male hormones (androgens) in fetal life may permanently prevent normal genes from working the way they're supposed to — a process known as gene expression. This may promote a male pattern of abdominal fat distribution, which increases the risk of insulin resistance and low-grade inflammation. Research continues to establish to what extent these factors might contribute to PCOS. Tests and diagnosis :There's no specific test to definitively diagnose polycystic ovary syndrome. The diagnosis is one of exclusion, which means your doctor considers all of your signs and symptoms and then rules out other possible disorders. 49 Medical history. Your doctor may ask questions about your menstrual periods, weight changes and other symptoms. Physical examination. During your physical exam, your doctor will note several key pieces of information, including your height, weight and blood pressure. Pelvic examination. During a pelvic exam, your doctor visually and manually inspects your reproductive organs for signs of masses, growths or other abnormalities. Blood tests. Your blood may be drawn to measure the levels of several hormones to exclude possible causes of menstrual abnormalities or androgen excess that mimic PCOS. Additional blood testing may include fasting cholesterol and triglyceride levels and a glucose tolerance test, in which glucose levels are measured while fasting and after drinking a glucose-containing beverage. Pelvic ultrasound. A pelvic ultrasound( abdominal and transvaginal ultrasound ) can show the appearance of the ovaries and the thickness of the lining of the uterus. Treatments and drugs :Polycystic ovary syndrome treatment generally focuses on management of individual main concerns, such as infertility, hirsutism, acne or obesity. Schedule regular checkups Long term, managing cardiovascular risks, such as obesity, high blood cholesterol, type 2 diabetes and high blood pressure, is important. To help guide ongoing treatment decisions. Adjusting lifestyle habits Making healthy-eating choices and getting regular exercise is the first treatment approach your doctor might recommend, particularly if you're overweight. Obesity makes insulin resistance worse. Weight loss can reduce both insulin and androgen levels, and may restore ovulation. Regulate menstrual cycle doctor may prescribe low-dose birth control pills that contain a combination of synthetic estrogen and progesterone. They decrease androgen production and give your body a break from the effects of continuous estrogen. This decreases risk of endometrial cancer and corrects abnormal bleeding. An alternative approach is taking progesterone for 10 to 14 days each month. This regulates periods and offers protection against endometrial cancer, but it doesn't improve androgen levels. doctor also may prescribe metformin (Glucophage, Glucophage XR), an oral medication for type 2 diabetes that lowers insulin levels. This drug improves ovulation and leads to regular menstrual cycles. Metformin also slows the progression to type 2 diabetes Reduce excessive hair growth doctor may recommend birth control pills to decrease androgen production, or another medication called spironolactone (Aldactone) that blocks the effects of androgens on the skin. Because spironolactone can cause birth defects, effective contraception is required when using the drug, and it's not recommended if you're pregnant or planning to become pregnant. Eflornithine (Vaniqa) is another medication possibility; the cream slows facial hair growth in women. 50 Shaving, waxing and depilatory creams are nonprescription hair removal options. Results may last several weeks, and then you need to repeat treatment. For longer lasting hair removal, your doctor might recommend a procedure that uses electric current (electrolysis) or laser energy to destroy hair follicles and control unwanted new hair growth. -Use medication to induce ovulation If woman trying to become pregnant, may need a medication to induce ovulation. Clomiphene citrate (Clomid, Serophene) is an oral anti-estrogen medication that taken in the first part of your menstrual cycle. If Clomiphene citrate alone isn't effective, may add metformin to help induce ovulation. Also may recommend using gonadotropins — follicle-stimulating hormone (FSH) and luteinizing hormone (LH) medications that are administered by injection. surgery If medications don't help you become pregnant, an outpatient surgery called laparoscopic ovarian drilling is an option for some women with PCOS In this procedure, a surgeon makes a small incision in the abdomen and inserts a tube attached to a tiny camera (laparoscope). The camera provides the surgeon with detailed images of the ovaries and neighboring pelvic organs. The surgeon then inserts surgical instruments through other small incisions and uses electrical or laser energy to burn holes in follicles on the surface of the ovaries. The goal is to induce ovulation by reducing androgen levels. Complications Having polycystic ovary syndrome makes the following conditions more likely, especially if obesity also is a factor: 51 Type 2 diabetes High blood pressure Cholesterol abnormalities, such as high triglycerides or low highdensity lipoprotein (HDL) cholesterol, the so-called "good" cholesterol Elevated levels of C-reactive protein, a cardiovascular disease marker Metabolic syndrome, a cluster of signs and symptoms that indicate a significantly increased risk of cardiovascular disease Sleep apnea Abnormal uterine bleeding Cancer of the uterine lining (endometrial cancer), caused by exposure to continuous high levels of estrogen Gestational diabetes or pregnancy-induced high blood pressure, if you do become pregnant Nomenclature Other names for this syndrome include polycystic ovarian syndrome (also PCOS), polycystic ovary disease (PCOD), functional ovarian hyperandrogenism, Stein-Leventhal syndrome (original name, not used in modern literature), ovarian hyperthecosis and sclerocystic ovary syndrome. Dysfunctional uterine bleeding: -Abnormal uterine bleeding is a common presenting problem . (DUB) is defined as abnormal uterine bleeding in the absence of organic disease. Dysfunctional uterine bleeding is the most common cause of abnormal vaginal bleeding during a woman's reproductive years. Dysfunctional uterine bleeding can have a substantial financial and quality-of-life burden. It affects women's health both medically and socially. - Terms frequently used to describe abnormal uterine bleeding: Menorrhagia - Prolonged (>7 d) or excessive (>80 mL daily) uterine bleeding occurring at regular intervals Metrorrhagia - Uterine bleeding occurring at irregular and more frequent than normal intervals Menometrorrhagia - Prolonged or excessive uterine bleeding occurring at irregular and more frequent than normal intervals Intermenstrual bleeding - Uterine bleeding of variable amounts occurring between regular menstrual periods Midcycle spotting - Spotting occurring just before ovulation, typically from declining estrogen levels Postmenopausal bleeding - Recurrence of bleeding in a menopausal woman at least 6 months to 1 year after cessation of cycles Amenorrhea - No uterine bleeding for 6 months or longer -Dysfunctional uterine bleeding is a diagnosis of exclusion. It is ovulatory or anovulatory bleeding, diagnosed after pregnancy, medications, iatrogenic causes, genital tract pathology, malignancy, and systemic disease have been ruled out by appropriate investigations. Approximately 90% of dysfunctional uterine bleeding cases result from an ovulation, and 10% of cases occur with ovulatory cycles. -Anovulatory dysfunctional uterine bleeding results from a disturbance of the normal hypothalamic-pituitary-ovarian axis and is particularly common at the extremes of the reproductive years. When ovulation 52 does not occur, no progesterone is produced to stabilize the endometrium; thus, proliferative endometrium persists. Bleeding episodes become irregular, and amenorrhea, metrorrhagia, and menometrorrhagia are common. Bleeding from anovulatory dysfunctional uterine bleeding is thought to result from changes in prostaglandin concentration, increased endometrial responsiveness to vasodilating prostaglandins, and changes in endometrial vascular structure. -In ovulatory dysfunctional uterine bleeding, bleeding occurs cyclically, and menorrhagia is thought to originate from defects in the control mechanisms of menstruation. It is thought that, in women with ovulatory dysfunctional uterine bleeding, there is an increased rate of blood loss resulting from vasodilatation of the vessels supplying the endometrium due to decreased vascular tone, and prostaglandins have been strongly implicated. Therefore, these women lose blood at rates about 3 times faster than women with normal menses.4 -Mortality/Morbidity Morbidity is related to the amount of blood loss at the time of menstruation, which occasionally is severe enough to cause hemorrhagic shock. Excessive menstrual bleeding accounts for two thirds of all hysterectomies and most endoscopic endometrial destructive surgery. Menorrhagia has several adverse effects, including anemia and iron deficiency, reduced quality of life, and increased healthcare costs.1 -Race Dysfunctional uterine bleeding has no predilection for race; however, black women have a higher incidence of leiomyomas and, as a result, they are prone to experiencing more episodes of abnormal vaginal bleeding. -Age Dysfunctional uterine bleeding is most common at the extreme ages of a woman's reproductive years, either at the beginning or near the end, but it may occur at any time during her reproductive life. 53 Most cases of dysfunctional uterine bleeding in adolescent girls occur during the first 2 years after the onset of menstruation, when their immature hypothalamic-pituitary axis may fail to respond to estrogen and progesterone, resulting in an ovulation. Abnormal uterine bleeding affects up to 50% of perimenopausal women. In the perimenopausal period, dysfunctional uterine bleeding may be an early manifestation of ovarian failure causing decreased hormone levels or responsiveness to hormones, thus also leading to anovulatory cycles. In patients who are 40 years or older, the number and quality of ovarian follicles diminishes. Follicles continue to develop but do not produce enough estrogen in response to FSH to trigger ovulation. The estrogen that is produced usually results in late-cycle estrogen breakthrough bleeding. -History 54 Patients often present with complaints of amenorrhea, menorrhagia, metrorrhagia, or menometrorrhagia. The amount and frequency of bleeding and the duration of symptoms, as well as the relationship to the menstrual cycle, should be established. Ask patients to compare the number of pads or tampons used per day in a normal menstrual cycle to the number used at the time of presentation. The average tampon or pad absorbs 20-30 mL or vaginal effluent. Personal habits vary greatly among women; therefore, the number of pads or tampons used is unreliable. The patient should be questioned about the possibility of pregnancy.3 A reproductive history should always be obtained, including the following: o Age of menarche and menstrual history and regularity o Last menstrual period (LMP), including flow, duration, and presence of dysmenorrhea o Postcoital bleeding o Gravida and para o Previous abortion or recent termination of pregnancy o Contraceptive use, use of barrier protection, and sexual activity (including vigorous sexual activity or trauma) o History of sexually transmitted diseases (STDs) or ectopic pregnancy Questions about medical history should include the following: o Signs and symptoms of anemia or hypovolemia (including fatigue, dizziness, and syncope) o Diabetes mellitus o Thyroid disease o Endocrine problems or pituitary tumors o Liver disease o Recent illness, psychological stress, excessive exercise, or weight change o Medication usage, including exogenous hormones, anticoagulants, aspirin, anticonvulsants, and antibiotics An international expert panel including obstetrician/gynecologists and hematologists has issued guidelines to assist physicians to better recognize bleeding disorders, such as von Will brand disease, as a cause of menorrhagia and postpartum hemorrhage and to provide disease-specific therapy for the bleeding disorder.5Historically, a lack of awareness of underlying bleeding disorders has led to under diagnosis in women with abnormal reproductive tract bleeding. The panel provided expert consensus recommendations on how to identify, confirm, and manage a bleeding disorder. If a bleeding disorder is suspected, evaluation for a coagulation problem is required and consultation with a hematologist is suggested. An underlying bleeding disorder should be considered when a patient has any of the following: o Menorrhagia since menarche o Family history of bleeding disorders o Personal history of 1 or several of the following: Notable bruising without known injury Bleeding of oral cavity or GI tract without obvious lesion Epistaxis >10 min duration (possibly necessitating packing or cautery) -Physical 55 Vital signs, including postural changes, should be assessed. Initial evaluation should be directed at assessing the patient's volume status and degree of anemia. Examine for pallor and absence of conjunctival vessels to gauge anemia. An abdominal examination should be performed. Femoral and inguinal lymph nodes should be examined. Stool should be evaluated for the presence of blood. Patients who are hemodynamically stable require a pelvic speculum, bimanual, and rectovaginal examination to define the etiology of vaginal bleeding. A careful physical examination will exclude vaginal or rectal sources of bleeding. The examination should look for the following: o The vagina should be inspected for signs of trauma, lesions, infection, and foreign bodies. o The cervix should be visualized and inspected for lesions, polyps, infection, or intrauterine device (IUD). o Bleeding from the cervical os o A rectovaginal examination should be performed to evaluate the cul-de-sac, posterior wall of the uterus, and uterosacral ligaments. Uterine or ovarian structural abnormalities, including leiomyoma or fibroid uterus, may be noted on bimanual examination. Patients with hematologic pathology may also have cutaneous evidence of bleeding diathesis. Physical findings include petechiae, purpura, and mucosal bleeding (eg, gums) in addition to vaginal bleeding. Patients with liver disease that has resulted in a coagulopathy may manifest additional symptomatology because of abnormal hepatic function. Evaluate patients for spider angioma, palmar erythema, splenomegaly, ascites, jaundice. Women with polycystic ovary disease present with signs of hyperandrogenism, including hirsutism, obesity, acne, palpable enlarged ovaries, and acanthosis nigricans (hyper pigmentation typically seen in the folds of the skin in the neck, groin, or axilla) Hyperactive and hypoactive thyroid can cause menstrual irregularities. Patients may have varying degrees of characteristic vital sign abnormalities, eye findings, tremors, changes in skin texture, and weight change. Goiter may be present. -Causes; Systemic disease, including thrombocytopenia, hypothyroidism, hyperthyroidism, C ushing disease, liver disease, diabetes mellitus, and adrenal and other endocrine disorders, can present as abnormal uterine bleeding. Pregnancy and pregnancy-related conditions may be associated with vaginal bleeding. Trauma to the cervix, vulva, or vagina may cause abnormal bleeding. Carcinomas of the vagina, cervix, uterus, and ovaries must always be considered in patients with the appropriate history and physical examination findings. Endometrial cancer is associated with obesity, diabetes mellitus, anovulatory cycles, nulliparity, and age older than 35 years. Other causes of abnormal uterine bleeding include structural disorders, such as functional ovarian cysts,cervicitis, endometritis, salpingitis, leiomyomas, and adenomyosis. Cervical dysplasia or other genital tract pathology may present as postcoital or irregular bleeding. Polycystic ovary disease results in excess estrogen production and commonly presents as abnormal uterine bleeding. Primary coagulation disorders, such as von Will brand disease, myeloproliferative disorders, and immune thrombocytopenia, can present with menorrhagia. Excessive exercise, stress, and weight loss cause hypothalamic suppression leading to abnormal uterine bleeding due to disruption along the hypothalamus-pituitary-ovarian pathway. Bleeding disturbances are common with combination oral contraceptive pills as well as progestin-only methods of birth control. However, the incidence of bleeding decreases significantly with time. Therefore, only counseling and reassurance are required during the early months of use. Contraceptive intrauterine devices (IUDs) can cause variable vaginal bleeding for the first few cycles after placement and intermittent spotting subsequently. The progesterone impregnated IUD (Mirena) is associated with less menometrorrhagia and usually results in secondary amenorrhea . Differential Diagnoses Abortion, Complete 56 Fibroids (leiomyomata) Abortion, Incomplete Foreign body Abortion, Inevitable Hydatidiform Mole Abortion, Missed Hyperthyroidism Abortion, Threatened Hypothyroidism Abruptio Placentae Intrauterine devices Adenomyosis Liver disease An ovulation Mullerian Duct Anomalies Anticoagulants Oral contraceptives Antipsychotic Ovarian Cysts Arteriovenous Malformations Pelvic Inflammatory Disease Cervical Cancer Placenta Previa Cervicitis Platelet Disorders Coagulopathies Polycystic Ovarian Syndrome Cushing Syndrome Pregnancy, Ectopic Endocervical Polyp Prolactinoma Endometrial Carcinoma Renal disease Endometrial Polyp Trauma Endometriosis von Will brand Disease Estrogen Therapy Vulvovaginitis Laboratory Studies When evaluating a woman of reproductive age with vaginal bleeding, pregnancy must always be ruled out by urine or serum human chorionic gonadotropin. In a patient with any hemodynamic instability, excessive bleeding, or clinical evidence of anemia, a complete blood count is essential. Coagulation studies should be considered when indicated by the history or physical examination findings and in patients with underlying liver disease or other coagulopathies. In patients with suspected endocrine disorders, other laboratory studies such as thyroid function tests and prolactin levels may be helpful, although these results may not be available from the ED. Imaging Studies 57 Pelvic ultrasonography is an important imaging modality for nonpregnant patients with abnormal vaginal bleeding. It may determine the etiology of the bleeding such as a fibroid uterus, endometrial thickening, or a focal mass. o Thickened endometrium may indicate an underlying lesion or excess estrogen and may be suggestive of malignancy. An endometrial stripe measuring less than 4 mm thick is unlikely to have endometrial hyperplasia or cancer, and biopsy is often considered unnecessary before treatment. Women with a normal endometrial stripe (5–12 mm) may require biopsy, particularly if they have risk factors for endometrial cancer. When the endometrial stripe is larger than 12 mm, a biopsy should be performed.6 o Depending on the urgency to determine the etiology of bleeding and on the reliability of outpatient follow-up, ultrasonography may be deferred for outpatient evaluations because for the majority of nonpregnant patients, ultrasonographic findings do not immediately affect ED decision-making.3 Transvaginal ultrasonography may be particularly helpful in further delineating ovarian cysts and fluid in the cul-de-sac. Computed tomography is used primarily for evaluation of other causes of acute abdominal or pelvic pain. Magnetic resonance imaging is used primarily for cancer staging. Procedures Before instituting therapy, many consulting gynecologists perform endometrial sampling or biopsy to diagnose intrauterine pathology and to exclude endometrial malignancy. Endometrial biopsy is indicated for the following patients with abnormal uterine bleeding6 : o Women older than 35 years o Obese patients o Women who have prolonged periods of unopposed estrogen stimulation o Women with chronic an ovulation Hysteroscopy is the definitive way to detect intrauterine lesions. It offers a more complete examination of the surface of the endometrium. However, it is usually reserved for treating lesions that were detected by other less invasive means. Treatment Emergency Department Care 58 Hemodynamically unstable patients with uncontrolled bleeding and signs of significant blood loss should have aggressive resuscitation with saline and blood as with other types of hemorrhagic shock. o Evaluate ABCs and address the priorities. o Initiate 2 large-bore intravenous lines (IVs), oxygen, and cardiac monitor. o If bleeding is profuse and the patient is unresponsive to initial fluid management, consider administration of IV 59 conjugated estrogen (Premarin) 25 mg IV every 4-6 hours until the bleeding stops. o In women with severe, persistent uterine bleeding, an immediate dilation and curettage (D&C) procedure may be necessary. Combination oral contraceptive pills may be used in women who are not pregnant and have no anatomic abnormalities. An oral contraceptive with 35 mcg of ethinyl estradiol can be taken twice a day until the bleeding stops for up to 7 days, at which time the dose is decreased to once a day until the pack is completed. They provide the additional benefits of reducing dysmenorrhea and providing contraception. Side effects include nausea and vomiting. Progesterone alone can be used to stabilize an immature endometrium. It is usually successful in the treatment of women with anovulatory dysfunctional uterine bleeding (DUB) because these women have unopposed estrogen stimulation. Medroxyprogesterone acetate 10 mg is taken orally once daily for 10 days, followed by withdrawal bleeding 3-5 days after completion of the course. Currently, there is not enough evidence comparing the effect of either progesterone alone or in combination with estrogens for the treatment of dysfunctional uterine bleeding.7 No steroidal anti-inflammatory drugs (NSAIDs) are generally effective for the treatment of dysfunctional uterine bleeding and dysmenorrhea. NSAIDs inhibit cyclooxygenase in the arachidonic acid cascade, thus inhibiting prostaglandin synthesis and increasing thromboxane A2 levels. This leads to vasoconstriction and increased platelet aggregation. These medications may reduce blood loss by 20-50%. NSAIDs are most effective if used with the onset of menses or just prior to its onset and continued throughout its duration. Danazol creates a hypoestrogenic and hyper androgenic environment, which induces endometrial atrophy resulting in reduced menstrual loss. Side effects include musculoskeletal pain, breast atrophy, hirsutism, weight gain, oily skin, and acne. Because of the significant androgenic side effects, this drug is usually reserved as a second-line treatment for short-term use prior to surgery. Gonadotropin-releasing hormone agonists may be helpful for short-term use in inducing amenorrhea and allowing women to rebuild their red blood cell mass. They produce a profound hypoestrogenic state similar to menopause. Side effects include menopausal symptoms and bone loss with long-term use. Tranexamic acid is an antifibrinolytic drug that exerts its effects by reversibly inhibiting plasminogen. It diminishes fibrinolytic activity within endometrial vessels to prevent bleeding. It has been shown effective in reducing bleeding in up to half of women with dysfunctional uterine bleeding. Tranexamic acid is not approved for the treatment of dysfunctional uterine bleeding in the United States.6 Consultations Seek an emergency gynecologic consultation for patients requiring hemodynamic stabilization. If parenteral therapy does not completely arrest vaginal bleeding in the hemodynamically unstable patient, an emergency D&C may be warranted. Consultation with or urgent referral to a gynecologist for surgical treatment may be necessary for patients who do not desire fertility and in whom medical therapy fails. Both endometrial ablation and hysterectomy are effective treatments in women with dysfunctional uterine bleeding with comparable patient satisfaction rates. o Endometrial ablation may be performed using laser, electrocautery, or roller ball. Amenorrhea is seen in approximately 35% of women treated, and decreased flow is seen in another 45%; although, treatment failures increase with time following the procedure due to endometrial regeneration. A substantial number of patients receiving endometrial ablation require reoperation (30% by 48 months). o Hysterectomy is the most effective treatment for bleeding. However, it is associated with more frequent and severe adverse events compared with either conservative medical or ablation procedures. Operating time, hospitalization, recovery times, and costs are also greater. Hence, hysterectomy is reserved for selected patient populations. Medication The goals of pharmacotherapy are to control the bleeding, reduce morbidity, and prevent complications. Steroid hormones These agents may help control bleeding. Some of them are used when bleeding is profused and the patient is unresponsive to initial fluid management. Ethinyl estradiol 35 μg and norethindrone 1mg (Necon 1/35, Nortrel 1/35, Ortho-Novum 1/35, Norinyl 1 + 35) Reduces secretion of LH and FSH from pituitary by decreasing amount of GnRH. Contraceptive pills containing estrogen and progestin have been advocated for nonsmoking patients with DUB who desire contraception. Therapy also used to treat acute hemorrhagic uterine bleeding but not 60 as effective as other treatments perhaps because may take longer to induce endometrial proliferation when progestin is present. Suggested mechanisms by which hormonal therapy might affect bleeding include improvement in coagulation, alterations in the microvascular circulation, and improvements in endothelial integrity. In long-term management of DUB, combination oral contraceptives are very effective. Dosing Interactions Contraindications Precautions Adult 1 tab PO bid for 1 wk until bleeding stops, followed by 1 tab PO qd for 2 wk; followed by a week of inactive pills, during which a withdrawal bleed generally occurs. Pediatric Not established Danazol Synthetic steroid analog, derived from ethisterone, with strong antigonadotropic activity (inhibits LH and FSH) and weak androgenic action without adverse virilizing and masculinizing effects. Increases levels of C4 component of the complement. May push the resting hematopoietic stem cells into cycle, making them more responsive to differentiation by hematopoietic growth factors. May also stimulate endogenous secretion of erythropoietin. May impair clearance of immunoglobulin-coated platelets and decreases autoantibody production. Certain androgenic preparations have been used historically to treat mild-to-moderate bleeding, particularly in ovulatory patients with abnormal uterine bleeding. These regimens offer no real advantage over other regimens and might cause irreversible signs of masculinization in the patient. They seldom are used for this indication today. Use of androgens might stimulate erythropoiesis and clotting efficiency. Androgens alter endometrial tissue so that it becomes inactive and atrophic. Dosing Interactions Contraindications Precautions Adult 100-200 mg/d PO in divided doses Pediatric Not established 61 Estrogens, conjugated (Premarin) Causes vasospasm of uterine arteries and initiates several coagulationrelated functions, which decrease uterine bleeding. Use in pharmacologic doses also causes rapid growth of endometrial tissue over denuded and raw epithelial surface. Dosing Interactions Contraindications Precautions Adult Severe uncontrolled bleeding with problems of hemostasis: 25 mg IV slowly over 10-15 min q4-6h until bleeding stops; not to exceed 4 doses Moderate bleeding: 2.5 mg PO qd for days 1-25, followed by progesterone on days 16-25 Pediatric Not established; use judiciously in children whose bone growth is not yet complete because of effects on epiphyseal closure Medroxyprogesterone acetate (Provera) DOC for most patients with anovulatory DUB. After acute bleeding episode controlled, can be used alone in patients with adequate amounts of endogenous estrogen to cause endometrial growth. Progestin therapy in adolescents produces regular cyclic withdrawal bleeding until positive feedback system matures. Progestins stop endometrial growth and support and organize endometrium to allow organized sloughing after their withdrawal. Bleeding ceases rapidly because of an organized slough to the basalis layer. These drugs usually do not stop acute bleeding episodes, yet produce a normal bleeding episode following their withdrawal. Dosing Interactions Contraindications Precautions Adult 10 mg PO qd for first 10-12 d of menstrual cycle Depo-medroxyprogesterone (Depo-Provera) as 150 mg IM q3mo Progestin-only oral contraceptive pills: Daily after acute phase of bleeding For acute moderate bleeding: Oral contraceptive pills qid for 5-7 d or until bleeding stops Pediatric Not recommended 62 Nonsteroidal Anti-inflammatory Drugs (NSAIDs) These agents can decrease DUB through inhibition of prostaglandin synthesis. NSAIDs only need to be taken during menstruation. Naproxen (Naprosyn, Aleve, Naprelan) For relief of mild to moderate pain; inhibits inflammatory reactions and pain by decreasing activity of cyclooxygenase, which is responsible for prostaglandin synthesis. NSAIDs decrease intraglomerular pressure and decrease proteinuria. Dosing Interactions Contraindications Precautions Adult For moderate bleeding: 500 mg PO bid (with foods) Pediatric <12 years: Not established >12 years: 2.5 mg/kg/dose PO; not to exceed 10 mg/kg/d Gonadotropin Releasing Hormone Analog These agents are generally used for short-term use to induce amenorrhea and allow the rebuilding of the red blood cell mass. Leuprolide acetate (Lupron, Eligard) Suppresses ovarian and testicular steroid genesis by decreasing LH and FSH levels. Works by reducing concentration of GnRH receptors in the pituitary via receptor down regulation and induction of post receptor effects, which suppress gonadotropin release. After an initial gonadotropin release associated with rising estradiol levels, gonadotropin levels fall to castrate levels, with resultant hypogonadism. This form of medical castration is very effective in inducing amenorrhea, thus breaking ongoing cycle of abnormal bleeding in many anovulatory patients. Because prolonged therapy with this form of medical castration is associated with osteoporosis and other postmenopausal side effects, many practitioners add a form of low-dose hormonal replacement to the regimen. Because of the expense of these drugs, they usually are not used as a first-line approach but can be used to achieve short-term relief 63 from a bleeding problem, particularly in patients with renal failure or blood dyscrasia. Dosing Interactions Contraindications Precautions Adult 3.5-7.5 mg IM qmo; not to exceed 6 mo without addition of low-dose estrogen and progestin therapy Pediatric Not established Follow-up Further Inpatient Care Patients with severe, acute abnormal uterine bleeding and hemodynamic instability will require urgent gynecologic consultation and hospitalization. Further Outpatient Care Most patients with abnormal uterine bleeding without hemodynamic compromise should be referred to a gynecologist for definitive management on an outpatient basis. Inpatient & Outpatient Medications Patients with bleeding heavy enough to decrease hematocrit may be given ferrous sulfate tablets (325 mg tid). Hormone regimens, including combination oral contraceptives and cyclic progestins, may be continued for several months under the supervision of the consulting gynecologist. Complications Anemia (may become severe) Adenocarcinoma of the uterus (if prolonged, unopposed estrogen stimulation) Prognosis 64 Hormonal contraceptives reduce blood loss by 40-70% when used long term. Although medical therapy is generally used first, over half of women with menorrhagia undergo hysterectomy within 5 years of referral to a gynecologist.[2 ] Patient Education Instruct patients to continue prescribed medications, although bleeding may still be occurring during the early part of the cycle. Also, patients should be told to expect menses after cessation of the regimen. Young patients with small amounts of irregular bleeding need reassurance and observation only prior to instituting a drug regimen. Express to patients that pharmacologic intervention will not be necessary once menstrual cycles become regular. Discuss ways the patient can avoid prolonged emotional stress and maintain a normal body mass index. For excellent patient education resources, visit medicine's Women's Health Center. Also, see medicines' patient education articles Vaginal Bleeding and Mittelschmerz. Uterine Prolapse -Uterine prolapse ("dropped uterus") is a condition in which a woman's uterus (womb) sags or slips out of its normal position. The uterus may slip enough that it drops partially into the vagina (the birth canal), creating a perceptible lump or bulge. This is called incomplete prolapse. In a more severe case—known as complete prolapse—the uterus slips to such a degree that some of the tissue drops outside of the vagina. -Prolapse Definition Prolapse literally means "to fall out of place." In medicine, prolapse is a condition where organs, such as the uterus, fall down or slip out of place. It is generally reserved for organs protruding through the vagina, or for the misalignment of the valves of the heart. -Anatomy of the Vagina -The vaginal vault has three compartments: an anterior compartment (consisting of the anterior vaginal wall), a middle compartment (cervix), 65 and a posterior compartment (posterior vaginal wall). Uterine prolapse involves the cervix. Signs & Symptoms -Women with mild cases of uterine prolapse may have no obvious symptoms. However, as the slipped uterus falls further out of position, it can place pressure on other pelvic organs—such as the bladder or bowel—causing a variety of symptoms, including: Pelvic pressure: a feeling of heaviness or pressure in the pelvis Pelvic pain: discomfort in the pelvis, abdomen or lower back Pain during intercourse A protrusion of tissue from the opening of the vagina Recurrent bladder infections Unusual or excessive discharge from the vagina Constipation Difficulty with urination, including involuntary -loss of urine (female incontinence), or urinary frequency or urgency 1 Symptoms may be worsened by prolonged standing or walking, due to added pressure placed on the pelvic muscles by gravity. Causes of Uterine Prolapse -Trauma incurred during the birthing process, particularly with large babies or after a difficult labor and delivery, is one of the main causes of the muscle weakness that leads to uterine prolapse. Reduced muscle tone from aging, as well as lowered amounts of circulating estrogen after menopause, may also form contributing factors in pelvic organ prolapses. In rare circumstances, uterine prolapse may be caused by a tumor in the pelvic cavity. Genetics also may play a role; women of Northern European descent experience a higher incidence of uterine prolapse than do women of Asian and African heritage. Finally, increased intra-abdominal pressure, stemming from such diverse conditions as obesity, chronic lung disease and asthma, can be contributing factors in uterine prolapse. Risk Factors One or more pregnancies and vaginal births Giving birth to a large baby Increasing age Frequent heavy lifting Chronic coughing Frequent straining during bowel movements 4 -Stages of Uterine Prolapse Four stages of uterine prolapse are commonly defined: Staging Definitions Eversion: A turning outward or turning inside out 66 Procidentia: A prolapse or falling down Stage I of uterine prolapse is defined as descent of the uterus to any point in the vagina above the hymen (or hymenal remnants). Stage II of uterine prolapse is defined as descent to the hymen. Stage III of uterine prolapse is defined as descent beyond the hymen. Stage IV of uterine prolapse is defined as total eversion or procidentia.6 -Uterine prolapse always is accompanied by some degree of vaginal vault prolapse. Screening & Diagnosis -Diagnosing uterine prolapse requires a pelvic examination. You may be referred to a doctor who specializes in conditions affecting the female reproductive tract (gynecologist). The doctor will ask about your medical history, including how many pregnancies and vaginal deliveries you've had. He or she will perform a complete pelvic examination to check for signs of uterine prolapse. You may be examined while lying down and also while standing. Sometimes imaging tests, such as ultrasound or magnetic resonance imaging (MRI), might be performed to further evaluate the uterine prolapse. 7 Treatment -Losing weight, stopping smoking and getting proper treatment for contributing medical problems, such as lung disease, may slow the progression of uterine prolapse. -If you have very mild uterine prolapse, either without symptoms or with symptoms that aren't highly bothersome, no treatment is necessary. However, without treatment, you may continue to lose uterine support, which could require future treatment. Non-Surgical Options Surgical Options Hysterectomy is a way of treating problems that affect the uterus. Many conditions can be cured with hysterectomy. Because it is major surgery, you may want to explore other treatment options first. For conditions that have not responded to other treatments, a hysterectomy may be the best choice. You should be fully informed of all options before you decide. This pamphlet explains 67 reasons for having a hysterectomy how hysterectomy is performed risks of hysterectomy recovery after surgery Reasons for Hysterectomy -Hysterectomy is the surgical removal of the uterus. It is the second most common type of major surgery performed on women of childbearing age (the most common is cesarean delivery). Hysterectomy may be done to treat many conditions that affect the uterus: Uterine fibroids Endometriosis Pelvic support problems (such as uterine prolapsed) Abnormal uterine bleeding Cancer Chronic pelvic pain Types of Hysterectomy 68 -Hysterectomy is major surgery, and as with any major surgery, it carries risks. For many of the problems listed previously, other treatments can be tried first. After hysterectomy, you no longer are able to become pregnant. Discuss all of the treatment options for your specific condition with your health care provider. There are several kinds of hysterectomy: Total hysterectomy— The entire uterus, including the cervix, is removed. In a total radical hysterectomy, the entire uterus and support structures around the uterus are removed. It often is done to treat certain types of cancer. Supracervical (also called subtotal or partial) hysterectomy—The upper part of the uterus is removed but the cervix is left in place. Hysterectomy with removal of the fallopian tubes and ovaries—A hysterectomy does not include removal of the ovaries and fallopian tubes. Surgery to remove the ovaries is called an oophorectomy. Surgery to remove the fallopian tubes is called a salpingectomy. One or both of these procedures can be done at the same time as a hysterectomy. Sometimes, only one ovary or tube is removed. How Hysterectomy Is Performed A hysterectomy can be done in different ways. The way a hysterectomy is performed depends on the reason for the surgery and other factors, including your general health. You and your doctor will decide which route is safest and best for your situation Sometimes it is not possible to know before the surgery how the hysterectomy will be performed. In these cases, the decision is made after the surgery begins and the surgeon is able to see whether other problems are present. Vaginal Hysterectomy In a vaginal hysterectomy, the uterus is removed through the vagina. With this type of surgery, you will not have an incision (cut) on your abdomen. Because the incision is inside the vagina, the healing time may be shorter than with abdominal surgery. There may be less pain during recovery. Vaginal hysterectomy causes fewer complications than the other types of hysterectomy and is a very safe way to remove the 69 uterus. It also is associated with a shorter hospital stay and a faster return to normal activities than abdominal hysterectomy. A vaginal hysterectomy is not always possible. For example, women who have adhesions from previous surgery or who have a very large uterus may not be able to have this type of surgery. Laparoscopic Hysterectomy Abdominal Hysterectomy In an abdominal hysterectomy, the doctor makes an incision through the skin and tissue in the lower abdomen to reach the uterus. The incision may be vertical or horizontal. This type of hysterectomy gives the surgeon a good view of the uterus and other organs during the operation. This procedure may be chosen if you have large tumors or if cancer may be present. Abdominal hysterectomy may require a longer healing time than vaginal or laparoscopic surgery, and it usually requires a longer hospital stay. Laparoscopic Hysterectomy In a laparoscopic hysterectomy, laparoscope is used to guide the surgery. A laparoscope is a thin, lighted tube with a camera that is inserted into the abdomen through a small incision in or around the navel. It allows the surgeon to see the pelvic organs on a screen. Additional small incisions are made in the abdomen for other instruments used in the surgery. 70 There are three kinds of laparoscopic hysterectomy: 1. Total laparoscopic hysterectomy—A small incision is made in the navel for the laparoscope, and one or more small incisions are made in the abdomen for other instruments. The uterus is detached from inside the body. It then is removed in small pieces through the incisions, or the pieces are passed out of the body through the vagina. If only the uterus is removed and the cervix is left in place, it is called a supracervical laparoscopic hysterectomy. 2. Laparoscopic ally assisted vaginal hysterectomy (LAVH)—A vaginal hysterectomy is done with laparoscopic assistance. For example, the ovaries and fallopian tubes may be detached using laparoscopy, and then the uterus is detached and all of the organs are removed through the vagina. 3. Robot-assisted laparoscopic hysterectomy—Some surgeons use a robot attached to the laparoscopic instruments to help perform the surgery. Experience using this technology is limited. More information is needed to see if robotic surgery has added benefits over the other methods. Laparoscopic surgery has some benefits over abdominal surgery: The incisions are smaller, and there may be less pain. The hospital stay after laparoscopic surgery may be shorter. You may be able to return to your normal activities sooner. The risk of infection is lower. -There also are disadvantages. It often takes longer to perform laparoscopic surgery compared with abdominal or vaginal surgery. The longer you are under general anesthesia, the greater the risks for certain complications. Also, there is an increased risk for bladder injury in this type of surgery. *What to Expect -It is helpful to know what to expect before any major surgery. You will need to have a physical exam a few weeks before your surgery. Also, you may need lab tests. Depending on your health and your age, a chest X-ray or electrocardiography (ECG) may need to be done. Your doctor may tell you to take a laxative and to eat lightly the day before. On the day of your surgery, the following things may happen: 71 A needle is placed in your arm, wrist, or hand. It is attached to a tube called an intravenous (IV) line that will supply your body with fluids, medication, or blood. You will be given an antibiotic to prevent infection. Special stockings or devices may be placed on your lower legs to prevent deep vein thrombosis (DVT). This condition is a risk with any surgery. Women at high risk of DVT may be given a drug to prevent blood clots from forming in the legs. Monitors will be attached to your body before anesthesia is given. You may be given general anesthesia, which puts you to sleep, or regional anesthesia, which blocks out feeling in the lower part of your body. . Before you are given anesthesia, you likely will be asked to state your name, the type of surgery you are having, or other information. This standard procedure, called a “time-out,” is done to ensure that the right surgery is being done on the right patient. A thin tube called a catheter will be placed in your bladder. The catheter will drain urine from your bladder during the surgery. Risks Hysterectomy is one of the safest surgical procedures. But as with any surgery, problems can occur: Infection Bleeding during or after surgery Injury to the urinary tract or nearby organs Blood clots in the veins or lungs Problems related to anesthesia Death -Some problems related to the surgery may not show up until a few days, weeks, or even years after surgery. These problems include bowel blockage from scarring of the intestines or formation of a blood clot in the wound. These complications are more common after an abdominal hysterectomy. -Some people are at greater risk of complications than others. For example, if you have an underlying medical condition, you may be at greater risk for problems related to anesthesia. Your health care provider will assess your risks for complications and may take preventive measures. You should understand all of your specific risks before you have a hysterectomy and discuss any concerns you have with your health care provider. Your Recovery -If you have a hysterectomy, you may need to stay in the hospital for a few days. The length of your hospital stay will depend on the type of hysterectomy you had and how it was performed. -You will be urged to walk around as soon as possible after your surgery. Walking will help prevent blood clots in your legs. You also may receive medicine or other care to help prevent blood clots. 72 -You can expect to have some pain for the first few days after the surgery. You will be given medication to relieve pain. You will have bleeding and discharge from your vagina for several weeks. Sanitary pads can be used after the surgery. -During the recovery period, it is important to follow your health care provider’s instructions. Be sure to get lots of rest, and do not lift heavy objects until your doctor says you can. Do not put anything in your vagina during the first 6 weeks. That includes douching, having sex, and using tampons. -Work with your health care provider to plan your return to normal activities. As you recover, you may slowly increase activities such as driving, sports, and light physical work. If you can do an activity without pain and fatigue, it should be okay. If an activity causes pain, discuss it with your doctor. -Even after your recovery, you should continue to see your health care provider for routine gynecologic exams and general health care. Depending on the reason for your hysterectomy, you may still need pelvic exams and Pap tests. Effects of Hysterectomy -Hysterectomy can have both physical and emotional effects. Some last a short time. Others may last a long time. You should be aware of these effects before having the surgery. -The ovaries are the glands that produce estrogen, a hormone that affects the body in many ways. Depending on your age, if your ovaries are removed during hysterectomy, you will have signs and symptoms caused by a lack of estrogen Physical Effect -After hysterectomy, your periods will stop. If the ovaries are left in place and you have not yet gone through menopause, they will still produce estrogen and will continue to do so until they stop functioning naturally. Emotional Effects -It is not uncommon to have an emotional response to hysterectomy. How you will feel after the surgery depends on a number of factors and differs for each woman. -Some women feel depressed because they can no longer have children. If depression lasts longer than a few weeks, see your health care provider. Other women may feel relieved because the symptoms they were having have now stopped. 73 Sexual Effects -Some women notice a change in their sexual response after a hysterectomy. Because the uterus has been removed, uterine contractions that may have been felt during orgasm will no longer occur. Removal of the Ovaries During Hysterectomy If the ovaries are removed before menopause, you will experience effects caused by lack of estrogen. These effects are similar to those of menopause and include hot flashes, vaginal dryness, and sleep problems. However, symptoms may be more -Some women feel more sexual intense than what you would pleasure after hysterectomy. This experience if you went through may be because they no longer menopause over a few years, as is have to worry about getting normal. You also may be at risk of a pregnant. It also may be because fracture caused by osteoporosis at they no longer have the an earlier age than women who go discomfort or heavy bleeding through natural menopause. caused by the problem leading to hysterectomy. Most women who have these intense symptoms can be treated with -Some women wish to have a estrogen therapy. Estrogen therapy supracervical hysterectomy is given in several different ways, because they think it will have including as a pill, injection, skin less of an impact on their sexual patch, vaginal cream, or vaginal ring. response compared with a total The form chosen depends on your hysterectomy. Whereas sexual specific symptoms. It is important to response is different for every talk to your health care provider woman, research comparing about all of the options and which women who have had total ones are right for you. hysterectomies with those who have had supracervical hysterectomies has shown that there is no difference in sexual response and orgasms in women who have had the two types of surgery. Finally... -Hysterectomy is just one way to treat uterine problems. It is major surgery and carries some risks. For some conditions, other treatment options are available. For others, hysterectomy is the best choice. Your health care provider can help you weigh the options and make a decision. What is a Pap smear? A Pap smear (also known as the Pap test) is a medical procedure in which a sample of cells from a woman's cervix (the end of the uterus that extends into the vagina) is collected and spread (smeared) on a microscope slide. The cells are examined under a microscope in order to look for pre-malignant (before-cancer) or malignant (cancer) changes. 74 Who should have a Pap smear? Pregnancy does not prevent a woman from having a Pap smear. Pap smears can be safely done during pregnancy. Pap smear testing is not indicated for women who have had a hysterectomy (with removal of the cervix) for benign conditions. Women who have had a hysterectomy in which the cervix is not removed, called subtotal hysterectomy, should continue screening following the same guidelines as women who have not had a hysterectomy. What is the sample checked for? The cells on the slide are checked for signs that they're changing from normal to abnormal. Cells go through a series of changes before they turn into cancer. A Pap smear can show if your cells are going through these changes long before you actually have cancer. If caught and treated early, cervical cancer is not life-threatening. This is why getting regular Pap smears is so important. How is a Pap smear done? A woman should have a Pap smear when she is not menstruating. The best time for screening is between 10 and 20 days after the first day of her menstrual period. For about two days before testing, a woman should avoid douching or using spermicidal foams, creams, or jellies or vaginal medicines (except as directed by a physician). These agents may wash away or hide any abnormal cervical cells. A Pap smear can be done in a doctor's office, a clinic, or a hospital by either a physician or other specially trained health care professional, such as a physician assistant, anurse practitioner, or a nurse midwife. With the woman positioned on her back, the clinician will often first examine the outside of the patient's genital and rectal areas, including the urethra (the opening where urine leaves the body), to assure that they look normal. A speculum is then inserted into the vaginal area (the birth canal). (A speculum is an instrument that allows the vagina and the cervix to be viewed and examined.) A cotton swab is sometimes used to clear away mucus that might interfere with an optimal sample. A small brush called a cervical brush is then inserted into the opening of the cervix (the cervical os) and twirled around to collect a sample of cells. Because this sample comes from inside the cervix, is called the endocervical sample ("endo" meaning inside). 75 A second sample is also collected as part of the Pap smear and is called the ectocervical sample ("ecto" meaning outside). These cells are collected from a scraping of the area surrounding, but not entering, the cervical os. Both the endocervical and the ectocervical samples are gently smeared on a glass slide and a fixative (a preservative) is used to prepare the cells on the slide for laboratory evaluation. What do the results mean? A normal Pap smear means that all the cells in your cervix are normal and healthy. An abnormal Pap smear can be a sign of a number of changes in the cells on your cervix: Inflammation (irritation). This can be caused by an infection of the cervix, including a yeast infection, infection with the human papillomavirus (HPV) the herpes virus or many other infections. Abnormal cells. These changes are called cervical dysplasia. The cells are not cancer cells, but may be precancerous (which means they could eventually turn into cancer). More serious signs of cancer. These changes affect the top layers of the cervix but don't go beyond the cervix. More advanced cancer. What abnormal results mean The Pap smear is a screening test. Abnormal values are based on the test results. The current system divides the results into three main areas: ASCUS or AGUS (atypical cells of uncertain significance) LSIL (low-grade dysplasia) or HSIL (high-grade dysplasia) Possibly cancerous (malignant) When a Pap smear shows abnormalities, further testing or follow-up is needed. The next step depends on the results of the Pap smear, your previous history of Pap smears, and risk factors you may have for cervical cancer. If the Pap smear shows minor cell changes or abnormalities, a colposcopy-directed biopsy probably will NOT be done right away unless there is a reason to believe you may be in a high-risk category. With an ASCUS result, an HPV test is done to check for the presence of the HPV virus types most likely to cause cancer. If the HPV test is negative, then colposcopy will not be needed. For minor cell changes, doctors usually recommend having a repeat Pap smear in 6 months. With a negative HPV test result, it's acceptable to have the repeat Pap done in 1 year. 76 Which women are at increased risk for having an abnormal Pap smear? A number of risk factors have been identified for the development of cervical cancer and precancerous changes in the cervix. HPV: The principal risk factor is infection with the genital wart virus, also called the human papillomavirus (HPV), although most women with HPV infection do not get cervical cancer. About 95%100% of cervical cancers are related to HPV infection. Some women are more likely to have abnormal Pap smears than other women. Smoking: One common risk factor forpremalignant and malignant changes in the cervix is smoking. Although smoking is associated with many different cancers, many women do not realize that smoking is strongly linked to cervical cancer. Smoking increased the risk of cervical cancer about two to four fold. Weakened immune system: Women whose immune systems are weakened or have become weakened by medications (for example, those taken after an organ transplant) also have a higher risk of precancerous changes in the cervix. Medications: Women whose mothers took the drug diethylstilbestrol (DES) during pregnancy also are at increased risk. Other risk factors: Other risk factors for precancerous changes in the cervix and an abnormal Pap testing include having multiple sexual partners and becoming sexually active at a young age. What the risks are There are no risks involved. Special considerations The following drugs may affect Pap smears: Colchicine Compounds in cigarettes Estrogen Podophyllin Progestins Silver nitrate 77 78