Tables - WebmedCentral.com
advertisement
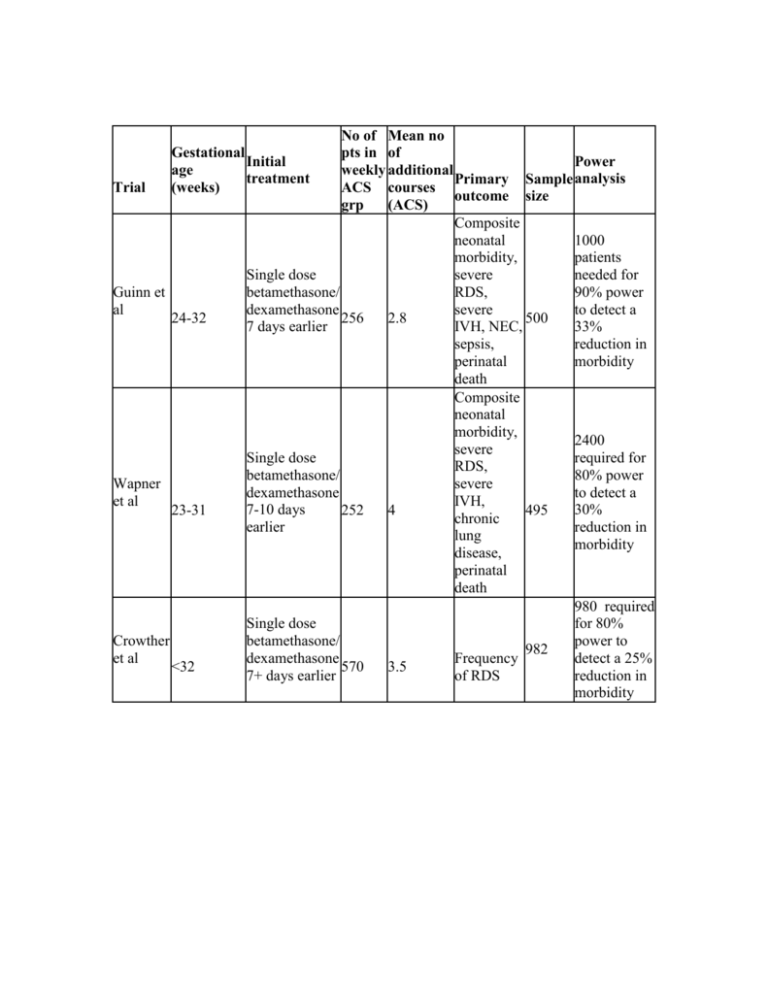
No of Mean no Gestational pts in of Initial Power age weekly additional treatment Primary Sample analysis (weeks) ACS courses Trial outcome size grp (ACS) Composite neonatal 1000 morbidity, patients Single dose severe needed for Guinn et betamethasone/ RDS, 90% power al dexamethasone severe to detect a 24-32 256 2.8 500 7 days earlier IVH, NEC, 33% sepsis, reduction in perinatal morbidity death Composite neonatal morbidity, 2400 severe Single dose required for RDS, betamethasone/ 80% power Wapner severe dexamethasone to detect a et al IVH, 7-10 days 30% 23-31 252 4 495 chronic earlier reduction in lung morbidity disease, perinatal death 980 required Single dose for 80% Crowther betamethasone/ power to 982 et al dexamethasone detect a 25% Frequency <32 570 3.5 7+ days earlier reduction in of RDS morbidity Garite et al <33 Study Guinn et al Single dose dexamethasone 14 days earlier 223 Treatment Composite morbidity Placebo ACS 28% 22.5% Comments Non sig* Placebo 8% Wapner et ACS 9.1% al Comments Placebo Crowther et ACS al Comments Placebo 63.6% Garite et al ACS 43.9% Comments P=0.02 *Non sig= Not statistically significant Composite neonatal morbidity, severe RDS, severe IVH, 437 NEC, perinatal death 1 217 required for 80% power to detect a 40% reduction in morbidity 24.5% 15.3% P=0.01, significant 876 856 Mean head circumferences (cm) 29.4 29.1 Non sig* Non sig* (reduced) Reduced by 95 (not affected) 33% 41% (reduced) (reduced) 2821 2803 32.5 33.0 Severe RDS 61.6% 41.4% P=0.02 Mean birth weights (g) Composite morbidity Guinn et reduced al Severe RDS reduced (better Wapner et No difference pulmonary al outcomes) Crowther et al (better pulmonary outcomes) Garite et reduced al reduced Birth weight Small effect Long term Head circumference concerns Small effect - Age 2-3: concerns reduced reduced over cerebral palsy Age 2: Reduced concerns Reduced (short (short over term) term) attention problems No No difference difference Considerations for Education & Practice Limit the number of absolute courses of ACS given. Only treat babies most likely to deliver at a gestational age where they would benefit mostly from ACS treatment. Best approach is a ‘rescue course’: initial course of ACS administered when preterm birth is likely. If the patient does not deliver over the next 7 or more days, a repeat ACS course can be given up to 32 weeks’ gestation. Considerations for further research Although a great deal of research exists, there is still a need for RCT’s to determine the best possible number of courses of ACS to reduce neonatal RDS without adversely affecting other neonatal outcomes. Searching for the best dosage and timing, and the risk-benefit ratio can only be accomplished through continued research. Well structured RCT’s that evaluate single and multiple courses are needed to answer important questions such as: Do repeat ACS doses maintain the production of surfactant in the foetal lung? Do the effects of ACS change with time to delivery? What are possible long-term consequences of repeat ACS in terms of behaviour? The primary goal of perinatal medicine is to minimize neonatal morbidity and mortality, but we need a better understanding of the mechanisms of preterm birth for more effective prevention, in order to prevent all complications associated with premature birth, including RDS.