Exemplar Q4
advertisement

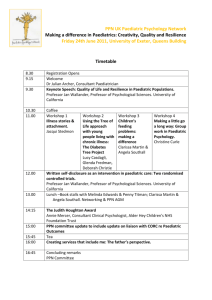
STAFF TRAINING AND PROFESSIONAL DEVELOPMENT QUESTION 4 Please describe the child, youth and whanau-centred specific components of your workforce development plan / framework for staff who provide care for children, young people and their whānau in non–dedicated paediatric areas of your DHB e.g. Emergency Department, Intensive Care Unit, Surgical etc. THE BIG PICTURE This domain has identified current practice that supports the knowledge and skills of staff providing paediatric care in non-dedicated paediatric areas. This was consistently shown in such areas such as ICU, ED, and Public Health Nurses but very little comment was made about other areas such as outpatients, operating theatre. One DHB identified themselves as leaders, while others identified areas of good practice. Regular paediatric specific education that is available across the multidisciplinary teams, including an orientation package, and simulation training, were some of the themes that were identified from the DHB responses. There were a number of courses that were frequently referred to as being useful in empowering staff to care for sick children. DHB feedback however identified that while training was available there was often little evidence of attendance and paediatric knowledge competency being measured. Other ideas included paediatric champions in non-dedicated paediatric areas that liaised with paediatric teams. This helped raise the focus of child and youth health as well as family focused care, in these often, adult orientated areas. Staff rotation through paediatric specific areas was also identified as a method to up skill knowledge on paediatric issues and improved relationships between areas. Throughout the responses, most areas (but not all) identified that all staff completed family violence and child abuse training. This is possibly attributed to Ministry of Health mandatory requirements in relation to this area. So maybe some learning could be taken from this. HOW THIS COMPASS DOMAIN HELPS Some DHBs have identified orientation and training packages that they developed and may be happy to share with other DHBs. These packages could be adapted to other areas, ensuring a more standardised approach to paediatric care competency. Courses that were commonly identified as part of the paediatric specific training were: Advanced paediatric life support (APLS), PALS, Emergency Nurse Paediatric Course (ENPC) These are all nationally and internationally recognized courses and if funding could be made available, they could become a mandatory part of training for areas such as ICU and ED. SUGGESTED GOOD PRACTICE MODEL The Working Group suggested that good practice for staff training and professional development included: Regular training sessions in child anatomy and development, cultural competency, equity, rights of the child and young person and family, whānau and family centered care. These training packages should also include family violence, care and protection, communicating with children, pain assessment and management. Training in basic life support, for all health professionals working with children should be mandatory, with advanced skills also being mandatory for those working in high-risk areas such as ICU, ED and Theatres. These could include nationally and internationally recognized courses such as APLS, PALS and / or ENPC. The Working Group also suggested that having a liaison person working within the nondedicated paediatric area could act as a champion, and advocate for children and youth. This person or persons could liaise with the paediatric service to improve child and youth health EXEMPLARS Canterbury DHB has senior nurses within non-paediatric (ICU, ED) areas that have paediatric portfolios and who are responsible for ensuring child health needs are met. There is also a SMO with a child focus. There are a number of paediatric focused courses run throughout the year that are available for nursing and medical staff. These include such things as: paediatric generic orientation, assessing the acutely unwell child in the acute care setting, (CPIT). In specific areas there are identified courses and training to support paediatric care such as ED has a paediatric foundation course, procedural sedation study day, scenario training that includes medical and nursing staff. In ICU orientation packages with a specific paediatric component and paediatric specific workshops, that includes scenario-based teaching. Rotation of staff to Starship and or PICU or the paediatric ward was identified as useful for ICU nurses. After hours there is a dedicated child health coordinator that provides support to all areas. Counties Manakau DHB identified training packages related to family-centred care and informed consent for child and youth. They also have a compulsory Tikanga best practice and pacific cultural competency program for all staff Waitemata DHB has outlined a 2-day orientation program for staff in ED that includes anatomy and physiology, assessment, common presentations, rights of children, children’s common fears. There is a competency sign off and a paediatric specific drug test requirement. Inclusion of children, involvement of family and whānau and communication is included. Ongoing education around topics related to children occurs throughout the year , and fortnightly paediatric simulations scenarios are also part of ongoing training. During these simulations they have staff acting out the parent role to ensure care of families. A current trial is underway with a paediatric link nurse who coordinates paediatric care, mentors staff and identifies any emerging issues. This has proved very successful. They DHB is also about to implement a new role of paediatric nurse specialist, that will have robust training in association with Starship hospital and is expected to help develop a model of child and family-centred care. Starship, provide learning opportunities nationally with videoconferencing , annual paediatric updates, trauma conferences, and have a strong focus on child-centred care.