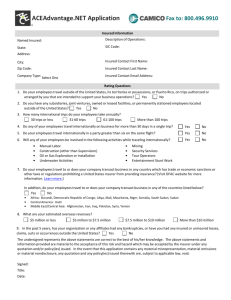
Policy Specimen For Visiting Visa
advertisement

MEDICAL EXPENSES INSURANCE FOR Traveler Health Insurance ISSUED BY HEALTH DEPARTMENT UNION INSURANCE COMPANY PSC P.O BOX 119227 Dubai-UAE WHEREAS the ‘Policy Holder’ named in “The Schedule” agrees hereto to pay the premium set forth in the said “The Schedule" to UNION INSURANCE COMPANY (Hereinafter called the “Company" or “UIC”) THE COMPANY HEREBY AGREES subject to the Schedule, Table of Benefits, Eligibility Definitions, Medical Insurance Clauses, General Provisions and Beneficiary User's Guide contained herein, endorsed or attached hereto or otherwise expressed hereon - to indemnify the Policy Holder up to but not exceeding the amounts specified in the Schedule against the Medical Expenses incurred by the Policy Holder for the treatment of his Employees and their dependents in the manner described hereafter. IN WITNESS whereof this Policy had been signed on behalf of the “Company” and the “Policy Holder” in UAE this --- of ------ 20--. THE COMPANY THE POLICYHOLDER M/s. Union Insurance Co. P.S.C. M/s. xxxxxxxxxxxx _______________________________ AUTHORIZED SIGNATORY HEAD OF HEALTH DEPARTMENT _______________________________ Name: Designation: Company Seal _______________________________ AUTHORIZED SIGNATORY ASSISTANT MANAGER HEALTH UNDERWRITING Page 2 of 18 THE SCHEDULE POLICY NUMBERS Please refer to the certificate number CLASS OF BUSINESS Medical Expenses for Travelers Visa From: from the legal entry stamp date PERIOD OF INSURANCE To: xx days from inception of policy Or until departure from UAE whichever occurs first. CURRENCY Arab Emirates Dirhams INSURANCE CONDITIONS As per the TABLE OF BENEFITS, ELIGIBILITY DEFINITIONS, MEDICAL INSURANCE CLAUSES, GENERAL PROVISIONS, and BENEFICIARY USER’S GUIDE attached Page 3 of 18 Table of Benefits BENEFITS & SERVICES Aggregate Limit COVERAGE AED 25,000/- Area of Cover UAE only Applicable Network Refer to www.unioninsuranceuae.com Mode of Claims Submission Pre-existing and Chronic Conditions INPATIENT Daily Room and Board Class Reimbursement Not Covered COVERAGE Ward Accommodation charges incurred as an In-Patient Covered Specialist Physicians’ Services for In-Patient Treatment Covered In-Patient Specialist Services including consultations and Diagnostic Procedures Covered Surgeon’s and Anesthetists’ Service Covered Local road ambulance Prescribed medicines and drugs combined administered whilst an Inpatient Covered Covered BASIS OF CLAIM SETTLEMENT Within the network Non network (for life threatening cases only) DEDUCTIBLE & COINSURANCE COVERAGE At Actual Up to maximum of customary charges not exceeding AED 7000/- per case COVERAGE Network Deductible 40% coinsurance Non network (for life threatening cases only) 40% coinsurance Page 4 of 18 DEFINITIONS: 1. ACCIDENT: A sudden, violent, unforeseen, unexpected and unintended event which leads to a person’s state of injury and/or ill-health and/or discomfort and/or pain and hence in need of immediate medical attention. 2. ACCIDENTAL INJURY: An Accident which causes acute physical damage to a Beneficiary, excluding underlying health problems, Causes or Pre-Existing Conditions that may aggravate or enlarge the Injury. Accidental Injury excludes chipping or cracking of teeth which is caused by reasons other than external impact. 3. APPLCIABLE NETWORK: The type of NETWORK assigned to the Group / Category as specified in the “Schedule”. 4. CAUSE: A term that broadly describes the reason a Beneficiary seeks healthcare, for an illness the description of the disease, for an accident the description of the accident. 5. CHRONIC CONDITION: A disease, illness or injury (including a mental condition) which has at least one of the following characteristics: Has no known cure, or recurs. Has only symptomatic/palliative cure whereby the state of disease never cured. Leads to permanent disability Is caused by changes to your body which cannot be reversed. Requires you to be specially trained or rehabilitated. Needs prolonged supervision, monitoring or treatment 6. CLAIM ADJUDICATION: The process of placing a claim through a series of administrative, contract and medical edits to determine coverage or non-coverage of a Claim as well as the determination of financial settlement parameters. 7. CLAIM SUBMISSION: A written demand made to the Company by or on behalf of the insured members for the payment of medical expenses under this contract. A claim is submitted on a Claim Form, which is accompanied by supporting billing documentation and medical reports proving that chargeable medical services were or will be rendered to the insured member and the medical reasons for conduction of such services. The insured member submits claim directly to the Company who then pays the Insured member (as per arrangement) Eligible medical expense minus any deductible, coinsurance, limits or other none covered medical expenses. 8. COINSURANCE / CO-PARTICIPATION: The portion of Eligible Medical Expenses, usually a fixed percentage of all services received by the Insured member and which, the insured member is obliged to pay. 9. CONCURRENT REVIEW: The ongoing review of a Beneficiary Illness or Injury during Confinement to determine appropriateness, Medical Necessity and coverage. 10. CONFINEMENT: An uninterrupted stay for a defined period of time in a Hospital followed by discharge. 11. COVERED CLAIM: A Claim that is eligible to be paid in whole or in part by the Insurer according to the Claims Adjudication process and the conditions of this Contract. Covered Claims may be comprised of Eligible Medical Expenses and/or Non-Eligible Medical Expenses and may be inclusive or not of Beneficiary out-of pocket amounts such as Specific Deductible Excess, Aggregate Deductible Excess, Co-Participation and/or Priority Payer shares and/or Limits as defined in the Applicable Scope of Coverage and Contract Schedules. In the event of any claim arising under the policy contract, all the supporting evidence, documents, must be submitted to the Insurer within 7 days after the occurrence of the claim 12. CUSTOMARY CHARGE: In the Company’s sole opinion, a charge or expense for medical care which according to the Company’s experience with their Network Providers does not exceed the general level of charges being made by other Providers of similar standing in the locality where the charge is incurred, when furnishing like or comparable medical Treatment, Services or supplies. 13. DISCHARGE SUMMARY: Summary of the Beneficiary’s Hospitalization course including the History & Physical Examination Report, diagnoses/es or Specific Assessment/s, complications incurred during the course of Hospitalization, therapy or Treatment which was provided, results of the Hospitalization and the discharge status of the Beneficiary including the status of the diagnosis/es or Specific Assessment/s, future medical Treatment, medications and follow-up directions. Page 5 of 18 14. ELIGIBLE MEDICAL EXPENSES: The Medical expenses which are determined by Claims Adjudication as covered by the Contract inclusive or not of Beneficiary out-of pocket amounts such as Specific Deductible Excess, Aggregate Deductible Excess, Co-Participation and/or Priority Payer shares and/or Limits as defined in the Applicable Scope of Coverage and Contract Schedules. 15. EMERGENCY (LIFE THREATENING SITUATION): A health condition sustained as a result of sudden, non-excluded Illness or Injury, raising a legitimate professional concern that there may be a significant medical problem necessitating Treatment (medical or Surgical) to be performed exclusively within the Territory of Occurrence which cannot be delayed and requires immediate Confinement to a Hospital followed by Hospitalization or not. Confinement must be conducted within 24 hours of the Illness or Injury onset. 16. EPISODE OF CARE: All Treatment rendered within a specified time frame for a Specific Assessment. The specified time frame for an In-patient Claim is defined as the period from Provider facility admission to discharge for the same corresponding admission. 17. EXCLUSION: Specified conditions, Illness/es, Treatment/s, Service/s, Cause/s, circumstances or other items that are expressly stated as not covered under this Contract. 18. EXCLUSION VALIDITY PERIOD: The specified number of days following a Contract’s Effective Date where certain Contract benefits for Illnesses, conditions, Treatments, other Services and any complication arising there from are not covered. Validity Periods may be applied to all, some or none of this Contract’s Exclusions and may or may not include a lifetime restriction on coverage in the event the Beneficiary obtains the condition during the Exclusion Validity Period. 19. EXPIRATION DATE: The day (00:00 hrs local time, month and year) this Contract expires. Healthcare expense benefits ends on this date. 20. GENERIC SUBSTITUTION: The method of dispensing the generic version of a drug in place of the original Product. 21. HAZARDOUS ACTIVITY AND PROFESSIONAL SPORTS: Sports All treatment of injuries and sickness consequent to the participation of the insured either as amateur or professional in hazardous sports including but not limited to shooting, motor sports, water sports (Diving, jet-skiing, power boats, water ski), Horse riding activities (hunting, Jumping, polo), Climbing activities (mountaineering and rock-climbing), Sports (bob sleighing, snowboarding, ice-hockey, ski-jumping, skiing outside permissible areas, underwater activities using artificial breathing apparatus, motor-racing, Rugby, boxing etc.) Parachuting hang-gliding Martial arts of all kinds, Dessert buggy rides, Dune bashing of all kinds. 22. HISTORY AND PHYSICAL EXAMINATION REPORT: A report issued by the Beneficiary’s Physician which details two sections of the Beneficiary’s medical profile: 1.) Section related to previous health status including history of previous Hospitalizations, previous Surgeries, previous Illnesses and Injuries, childhood diseases, allergies, medications, habits, etc. and 2.) Section related to the Beneficiary’s current Illness or Injury including date of onset, symptoms, physical examination, test results, diagnosis or Specific Assessment/s and planned therapy. 23. HOSPITAL: Any medical institution, public or private, which is legally licensed and provides medical Treatment to sick and injured persons. The facility must consist of organized premises, possess the necessary technical and scientific equipment for diagnosis and surgical operations and should provide healthcare Services 24hrs/a day by a staff of at least one resident Physician and qualified professional Nurses. The term "Hospital" excludes Outpatient clinics, sanitarium, physiotherapy centers, health clubs, retirement homes, nursing homes and other non-Hospital institutions, including those specialized in substance abuse (drugs, alcohol). 24. HOSPITAL CONFINEMENT or HOSPITALISATION: shall be deemed to refer only Inpatient confinement when a person is registered as bed patient in a hospital and incurs an overnight daily room and board charge. 25. HOSPITALIZATION CLASS: The class of room and board Service to be applied for Inpatient Confinements and which is identified in the Contract Schedule. 26. ILLNESS: A disease, impairment, interruption, cessation or disorder of bodily function/s, system/s or organ/s. 27. INJURY: Physical damage other than Illness, including all related conditions and recurrent symptoms which are usually caused by an Accident. Page 6 of 18 28. INPATIENT: Treatment, diagnostic procedures and or other types of care which are delivered to a Beneficiary in a Hospital and Medically Necessitate the Beneficiary’s Confinement to a Hospital as a registered bed patient for 24 hours or more. Day-Hosp admissions are considered Inpatient. 29. INSURED MEMBER: Any traveler visiting UAE with visit visa. 30. LENGTH OF STAY: The number of consecutive days a Beneficiary is confined. 31. LIMIT/S: A Contract provision that sets a cap on types of Eligible Medical Expenses. Limit/s may be a (1) Monetary amount per lifetime, (2) Quantity amount per lifetime, (3) Monetary amount per year, (4) Quantity amount per year, (5) Monetary amount per Claim, or (6) Quantity amount per Claim. 32. MEDICALLY NECESSARY: Hospitalizations, Confinements, Surgeries, procedures, Treatments, Services, supplies, medications, equipment or other items or expenses requested, provided or charged by a Provider which the Insurer, in its own opinion determines are all of the following: a. b. c. d. e. f. g. Required for the Treatment or management of an Illness or Injury; Appropriate to diagnose or treat the Beneficiary’s Illness or Injury consistent with standards of good medical practice; Are not primarily for the personal comfort or conveniences or the Beneficiary, family or the Provider; Are not or associated with the scholastic education or vocational training of the Beneficiary or primarily for education or experimental purposes; In case of Inpatient care, cannot be provided safely on an Outpatient basis and; Are given in the most cost efficient manner and setting consistent with maintaining safe care. Legally available in the country of prescription. The fact that a Provider has prescribed, recommended or approved a Hospitalization, Confinement, Surgery, procedure, Treatment, Service, supply, medication, equipment or other item or expense does not, in itself, make it Medically Necessary. 33. NETWORK: A group of healthcare Providers. 34. NON-ELIGIBLE MEDICAL EXPENSES: Medical expenses that are determined by Claims Adjudication as not covered by the Contract. 35. NON-NETWORK: Healthcare Service Providers that are not part of the Network list. 36. ORAL & MAXILLOFACIAL SURGERY: Excision of tumors, cysts of jaws, cheeks, lips, tongue, roof, floor of mouth; Reconstructive Surgery for Accidental Injuries to a Sound Natural Tooth, jaws, cheeks, lips, tongue, roof and floor of mouth; excision of jaws and hard palate, external incision and drainage of cellulitis, incision and Surgical Treatment of accessory sinuses, salivary glands or ducts, reduction of dislocations. 37. OUT-OF-POCKET EXPENSE: Eligible or Non-eligible Medical Expenses that must be paid by the Insured. 38. OUTPATIENT: Physician's consultation, prescribed drugs, diagnostic tests and Treatments which do not Medically Necessitate Hospitalization or specialized medical attention and care in a Hospital before, during and/or after the procedure. 39. PHYSICIAN: Shall be deemed to refer only to a Doctor or Surgeon who is a Doctor of medicine or equivalent legally licensed to practice medicine and qualified to render the treatment provided, under the law of jurisdiction in which Treatment is provided. 40. PLAN/PRODUCT: The covered Family of Benefits, Families of Services, covered Causes, Exclusions, the method of Claims handling, territorial Limits, financial restrictions that are offered by the Insurer under a given Product. 41. POLICY HOLDER: The legal entity that applies for this Contract and whose Application Form has been formally accepted by the Insurer. 42. PRE-EXISTING CONDITION: Bodily injuries or medical conditions relating to accidents or illnesses which occurred and/or were declared and/or have been diagnosed and/or have already incepted treatment relating to same prior to the commencement of this initial commencement date of the policy. Page 7 of 18 43. RECONSTRUCTIVE SURGERY: Any operative procedure or portion of a procedure performed to restore functionality or restore appearance which was lost due to Accidental Injury or Surgery or for which proper functionality or proper appearance did not exist due to a Congenital Disease. 44. SCOPE OF COVERAGE: A pre-defined frame which sets and defines the parameters of how a Beneficiary will be covered by the Insurer under a given Contract (e.g. Family of Benefits, territorial, financial Limits, etc.). 45. SPECIFIC EXCLUSIONS: The Exclusions that result from the Underwriting process, which are determined by the Insurer to be applied specifically to a certain Beneficiary. 46. SURGERY / SURGICAL: SURGERY OR SURGICAL OPERATION: shall be deemed to refer to the following: • • • • • • • • • • • 47. A cutting Operation Suturing a wound Treatment of a fracture Reduction of a dislocation Radiotherapy (excluding radioactive isotope therapy) if used in lieu of a cutting operation for the removal of tumor. Electrocatherisation Diagnostic and Therapeutic endoscopic procedures Injection treatment haemorrhoids and varicose veins Organ Transplant Angiography Normal Child birth. TREATMENT: Any Surgical, medical, pharmaceutical or other approach used to cure or rectify a Beneficiary Illness or Injury which is deemed as being Medically Necessary and which must be legally permitted in the country where the Treatment was prescribed and covered under this contract. Page 8 of 18 MEDICAL INSURANCE CLAUSES These Clauses issued in conjunction with the Policy to which it is attached witnesses that the Company has granted a Medical Insurance Cover whereby: CLAUSE 1: BENEFITS If an Insured Member, while insured under the terms of these Clauses, incurs medical expenses, the Company shall reimburse such expenses, subject to the provisions and limitations set forth hereinafter. The medical expenses should be incurred (i.e. Actual medical service rendered by medical service provider and its costs paid by insured member) within the policy expiry date (unless otherwise the policy has been renewed). If the policy lapses, then the costs payable are only those incurred in respect of medical services rendered up to the lapse date. CLAUSE 2: IN-PATIENT BENEFITS If, as a result of bodily injury or sickness, an Insured Member incurs expenses in connection with his hospital confinement, the Company shall pay the following benefits. (A) Daily Room/Board and Nursing: The expense incurred by the Insured Member for reasonable and customary charges made by the hospital for room, board and general nursing care furnished during his hospital confinement, but not to exceed the maximum amount as set forth in the Table of Benefits. (B) Hospital Services: The expense incurred by the Insured Member and directly related to the specific Illness for the services rendered during his confinement, but not to exceed during any one Disability the maximum under Hospital Services set forth in the Table of Benefits, and which are enumerated hereinafter 1. Use of operating room, treatment rooms and equipment. 2. Dressings, ordinary splint and plaster casts but excluding special braces, appliances and equipment. 3. Drugs and medicines prescribed by the attending physician and which are commercially available for purchase by the Hospital in which the Insured Member is confined. 4. When furnished as a regular service customarily provided by the hospital in which the Insured Member is confined, and when performed by an employee of the hospital: Laboratory examinations, electrocardiograms, basal metabolism tests, oxygen and anaesthetic and administration thereof, X-Ray examination, administration of blood and blood plasma, intravenous injections and solutions. 5. Administration of an anaesthetic by a qualified physician subject to maximum reimbursement, during any one Disability at actual costs. Hospital Services shall not include, and no reimbursement shall be made for expenses incurred for the services of technicians not regularly employed or designated by the hospital, or doctors, room, board or general nursing care, or any services furnished by the hospital other than those listed under Hospital Services above. (C) Surgical Fees: If the Insured Member undergoes a surgical operation, the Company shall pay the surgical fees actually charged for such operation (including charges for pre-and-post-operative care by the surgeon) subject to the following: 1. Payment of any surgical operation shall not exceed the amount the Company’s tariff, which reflects current UAE pricing structures for medical and surgical fees. If the intervention carried out is not listed in the mentioned tariff, an amount based on an operation of comparable severity and gravity as determined by the Company shall be paid unless payment for such operation is expressly accepted in such tariff or by the provisions of this Policy. 2. Payment for all surgical interventions performed during any Disability shall not exceed the Maximum Per Case shown in the Table of Benefits. Page 9 of 18 3. Any Surgical expense to be reimbursed must be incurred for services rendered by a physician legally licensed to practice, and qualified to render the service for which claim is made. (D) Doctor's Visits: If an Insured Member incurs expenses for care and treatment by a physician and: 1. Such care and treatment is given during the Insured Member's hospital confinement, and 2. Such confinement is for causes other than maternity The Company shall make reimbursement for such expenses up to the maximum amounts indicated in the Table of Benefits under "In-Hospital Benefits : Hospital Services, Surgical fee and Doctor's visit" section. Page 10 of 18 Policy Exclusions No payment shall be made for any Disability, treatment or service arising directly or indirectly due to, unless benefit option is specifically included in the Table Of Benefits: A) Injury or sickness caused directly or indirectly, wholly or partially by: 1. Self-destruction or intentionally self-inflicted injury or any attempt thereat, while sane or insane, resisting legal arrest, committing an illegal act. 2. War or warlike operations (whether war be declared or not), or invasion, act of foreign enemy, intervention of foreign power, hostilities, mutiny, strikes, riots or civil commotion, civil war, civil uprising or looting, sabotage, rebellion, revolution, insurrection, conspiracy, usurp of power whether by political or military means, state of siege or emergency, martial law, or any of the events or causes which determine the proclamation or maintenance of state of siege or emergency and martial law, every kind of projectile, explosives, including accidental explosion and / or deliberate explosion of weapons of war, during war or directly as a result of previous war, bullets, bombs or other military devices, acts or criminal acts by armed persons whether affiliated or not to any organization or political party, or militia, or military or paramilitary organization and/or the state becoming under the control of “De facto” or “De jure” authorities acting on their own behalf or for and on behalf of other organization(s), also murder or assault or any attempt thereat, and all malicious acts of any nature whatsoever. 3. Terrorism: loss, damage, cost or expense of whatsoever nature directly or indirectly caused by, resulting from or in connection with any act of terrorism regardless of any other cause or event contributing concurrently or in any other sequence to the loss. An act of terrorism means an act, including but not limited to the use of force or violence and/or the threat thereof, of any person or group(s) of persons, whether acting alone or on behalf of or in connection with any organization(s) or government(s), committed for political, religious, ideological or similar purposes including the intention to influence any government and/or to put the public, or any section of the public, in fear. 4. Radioactive contamination, ionizing radiation, radioactive, toxic, explosive or other hazardous properties of nuclear material thereof, and/or polluting hazardous or poisoning chemicals. 5. All treatment of injuries and sickness consequent to the participation of the insured either as amateur or professional in hazardous sports including but not limited to shooting, motor sports, water sports (diving, jetskiing, power boats, water ski), horse riding activities (hunting, jumping, polo), climbing activities (mountaineering and rock-climbing), winter sports (bob-sleighing, snowboarding, ice-hockey, snow-skiing, ski-jumping), martial arts of all kinds, etc. B) Treatment to illnesses in connection with: 1. Psychological and psychiatric illness, mental retardation, attention deficit disorders, developmental delays &/or advances &/or abnormalities whether physical, psychological, emotional, behavioral, speech or intellectual including precocious puberty, hearing difficulties, etc. 2. Senility related conditions including but not limited to Alzheimer’s disease, etc. 3. Pulmonary and/or Extra-pulmonary Tuberculosis and its complications after diagnosis as such, rest cures, custodial, Isolator, Quarantine Sanatorium Care 4. Routine medical examinations & tests including but not limited to preventative checks, screening tests, checkups, prophylactic treatment, routine pap smears, mole mapping, allergy testing, pre-operative infectious disease screenings, heart scans and bone densitometry. 5. Routine Optical Treatment including Eye checkups, Routine Sight Testing unless benefit option is specifically included in the Table Of Benefits. 6. Prostheses, permanent implants, corrective devices, equipment and medical appliances including optical aids (such as glasses, frames, lenses whether external or implanted) hearing aids, walking aids, supports, braces, artificial limbs, syringes, slings, bandages, breast pumps, nebulizers, air chambers, blood monitoring equipment, etc.Eye Surgeries for the sole purpose of correcting refractive errors, nearsightedness, farsightedness, astigmatism, cross-eyes. 7. All gum and dental related treatment unless resulting from an accident occurring during the policy. In such cases, treatment will be limited to coverage conducted within the first 48 hours after the accident. Page 11 of 18 8. Any maternity, prenatal, perinatal &/or postnatal related care, treatment, testing &/or services including any complication such as uterine prolapse, cystocele, rectocele and abortion. 9. All treatment, tests and services related to sexually transmitted diseases and related complications including but not limited to: gonorrhea, syphilis, HPV, all Hepatitis other than Type A, HIV, AIDs, herpes, pubic lice, trichomoniasis whether or not active sexual transmission is documented or known. 10. Male & female reproductive system disorders including impotence, erectile or sexual dysfunction, priaprism, contraception, sterilization or reversal of sterilization, sub-fertility, infertility, in-vitro fertilization, GIFT, surrogacy procedures. Assisted reproduction tests, infertility/fertility tests. Not limited to varicocele, frigidity, menstrual cycle disorders, ovarian cysts, polycystic ovarian disease, endometriosis, uterine fibroids. 11. Menopause and related management including but not limited to Hormone replacement therapy, Growth failure and Growth hormone replacement therapy 12. Routine or Preventive Treatment, Vaccine, Gammaglobulin, Immunomodulators &/or immunotherapy treatment or drugs including but not limited to “Remicade, Interferon unless used as effective therapeutic strategy for radical therapy, enzyme preparations, anti-oxidants, liver tonics, etc.” 13. Expenses of donor in organ transplant/implantation or any kind of organ transplant where insured member is donating an organ. 14. Chronic conditions requiring hemo dialysis or peritoneal dialysis, and related test/treatment or procedure. C) Any medical consultation, prescription or treatment related to: 1. Services or treatment in any long term care facility, rehabilitation centre, spa, hydro clinic, rest cures, sanatorium, home care, nursing home or home for the aged, periods of quarantine. 2. Treatment by alternative medicines and pathies including but not limited to acupuncture, acupressure, homeopath, ayurvedic, osteopath, chiropractic, reflexology, aromatherapy and like. 3. Special diet, Vitamins other than as part of prescribed treatment, Food supplements of all kinds, Children's food, Baby supplies. 4. Depression, Anxiety, Fatigue. 5. Hair falls including alopecia and Dandruff, Scalp treatment, implantation of hairs. 6. Cosmetic Treatment or Cosmetic Surgery, unless required as a result of injury and/or accident where such treatment/surgery is scheduled within a period not exceeding three years from date of such accident and/or injury. 7. Cosmetic Dental reconstruction unless required as a result of injury and/or accident where such reconstruction is scheduled within a period not exceeding six months from the date of such accident/injury which have occurred due to extrinsic factors. 8. Treatment relating to Acne, Warts and Corns. 9. Birth control (Devices, Pills, sterilization, etc.) and its complications thereof. 10. Drug, alcohol, substance abuse and addiction treatment including eating disorders, obesity, sleep apnea/snoring, removal of fat, bulimia, anorexia nervosa and other similar disorders. 11. Treatment for losing or gaining of weight, Obesity, Loss of Appetite, Anorexia, Bulimia and other such eating disorders. 12. Circumcision, bunions, molluscum contagiosum, nevus, mole, pigmentation disorders, etc. and treatment unless resulting from an accident (within 24 hours) that has occurred after the first enrolment date under the policy. 13. Vaccination such as B.C.G., Triple Vaccine, Poliomyelitis etc. Vaccination against communicable diseases such as Meningitis, Cholera, Hepatitis, Tuberculosis etc. 14. Organ, tissue, cell, blood & bone marrow donation or banking including complications related thereto. Page 12 of 18 15. Treatment/Tests and/or Medications of any condition that is cause by natural changes to a person body that cannot be reversed (i.e. hormone replacement therapy for menopause/ osteoporosis, deafness, etc.). 16. All conditions, testing, procedures related to determining, diagnosing or treating congenital diseases or malformations or pre-mature birth as well as complications arising there from. Congenital means all diseases, anomalies, hereditary conditions including neurological disorders, chromosomal &/or genetic, defects and deficiencies whether present at birth in either in an evident manner or in a potential manner triggered at a later stage. Treatment for pre-mature baby is not covered. 17. Naal septum deviation and nasal concha resection. D) Any treatment or test, medication, expenses which: 1. Is not related to a specific symptom and/or disease. 2. Is in the opinion of both the treating physician and Company’s Medical doctor are not medically necessary. 3. Is related to work and/or school application and/or entries and/or residence permits and/or medical reports and alike. 4. Is availed without required prior approval of Company 5. Genetic engineering and cloning. 6. Where the insured goes against medical advice. 7. Any pharmaceutical product not considered as medicine such as lozenges, mouthwashes/ mouth gargles, baby formula, soaps and shampoos (both medicated and non-medicated), cosmetic preparations, antiseptic solutions, dietary supplements, non-injectable vitamins unless medically necessitated, skin care products, slimming products etc., E) Any investigation, test or treatment which directly or indirectly, results from or is related to: 1. 2. Infection by which includes Seropositivity to any Human Immune Deficiency Virus (HIV) or Acquired Immune Deficiency Syndrome (AIDS) or any similar or related condition or Syndrome. or Any conditions or illness directly or indirectly arising from any such Infection, Condition or Syndrome. F) Nor shall payment be made for any part of Disability, treatment or service: 1. Due to injury or sickness arising out of or in the course of any employment for wage or profit, which sickness or injury is covered by a Workmen's Compensation Act or other similar legislation. (Unless specifically mentioned in the Schedule of Benefits as covered) G) Any treatment/test not required that in the sole decision of the insurer are not medically necessary. H) Any drug, device, medical treatment or procedure that in the sole discretion of the Insurer is deemed to be experimental or has not been established as being effective. I) Any disease declared as pandemic and/or epidemic by the World Health Organization and this for the duration of such declaration. J) Drugs without Doctor's prescription. Products / substances not considered as medicines (non-generic), cosmetic related products, products not considered as prescription drugs by Ministry of Health such as but not restricted to mouthwash, toothpaste, lozenges, antiseptic solutions, milk formulas, skin care products and diapers. K) Any treatment/test which preauthorization has not been approved. L) Transportation other than in local licensed ambulances. Hotel Accommodation charges. M) Companion Charges and Expenses except for companion with child under 16 years of age. N) Amounts in excess of UAE reasonable and customary charges admission/procedure/consumables for treatment by visiting doctors from overseas. for inpatient/daycare/outpatient O) Elective treatments outside the Geographical Limits specified in the Policy Schedule. Page 13 of 18 EXCLUDED PHARMACEUTICAL PRODUCTS Fertility, Infertility related Medicines / Agents. Sexual dysfunction medications. Psychotherapeutic Medications (tranquilizers, sedatives, appetite stimulants, appetite suppressants weakness or fatigue medications—etc). Oral Hygiene, Dental and Gum related Medicine and Products. Contraceptive Medicines and Products. Cosmetic Products, Acne Preparations & medications, Lotions, Moisturizers, creams, emollients, lubricants. Enzymes preparations, anti-oxidants, liver tonics. All kinds of Soaps, Shampoos & Cosmetics. Hair & Scalp Preparations. Vaccinations, Immunotherapy. Smoking Cessation, Nicotine / Alcohol Abuse Medications. AIDS/HIV Related Medicines. Orthopedic appliances such as; Collar/support, Jaw / Spine Braces Shoes / inserts, Crutches, Waist belt, Hernia belt, support stockings---etc. Pain Balms. Bandages, alcohol swabs, Band-Aids. Massage Creams, Fadeout Creams, Stretch Marks Creams, Sunscreens, Skin Bleaches, Masks, Face Cleansers. Oils like Castor Oil, Cod Liver Oil, Clove Oil, Eucalyptos Oil, Karvol Calamine Lotion. Hormone replacement therapy. Nappy rash cream. Hearing aids. Artificial tears, Liquifilm, Dura tears. Antiseptics such as cyteal solutions, Betadine alcoholic solution. Glucose Stripes, Lancets. Lozenges. Herbal preparations and other alternative medications. Medications that is not medically necessary and appropriate. Vitamins and Minerals. Supplements. Page 14 of 18 GENERAL PROVISIONS Article 1: INSURANCE POLICY (HEREIN REFERRED TO AS CONTRACT) The Policy, comprising the Schedule, Table of Benefits, Eligibility definitions, the Medical Insurance Clauses, the General Provisions, and Beneficiary User’s Guide attached hereto and the application of the Policy Holder and the Individual Applications, if any, of the Insured Members, shall constitute the entire contract between the parties hereto. This Policy and the Schedule shall be read together as one contract and any word or expression to which a specific meaning has been assigned in any part of this Policy or of the Schedule shall bear such specific meaning wherever it may appear. Special provisions shall be valid only when endorsed on this policy or confirmed in writing by the Company. Utmost Good Faith - The due observance and fulfilment of the Terms and Conditions of this Policy in so far as relating to the Insured's responsibility towards the declaration of all facts material to the Cover as afforded by this Policy and/or the computation of the respective Premium shall constitute conditions precedent to the liability of the Company towards awarding any payment with respect to claims under this Policy. Article 2: JURISDICTION This Policy shall be governed by the Laws of the country of office of issue as better described under the Schedule of the Policy. Article 3: PREMIUMS The Premium is the Gross Premium plus any applicable stamps and/or taxes if any. The Premiums due by the Policyholder to the Insurer as defined in the Contract Schedule are payable in advance by the Policyholder according to the frequency of payment agreed upon between the Policyholder and the Insurer and as specified in the Contract Schedule. The coverage provided by the Insurer under this Contract shall not commence until the first installment is fully paid. Article 4: CURRENCY Unless otherwise mentioned in the Policy Schedule, the currency of this Contract of Cover shall be deemed to be that of the country of the office of issue of the Policy. All payments by the Company under this policy shall be made in the same currency as that in which premiums were received by the Company with respect to the insurance hereunder, unless otherwise arranged by mutual agreement between the Policy Holder and the Company and defined accordingly by endorsement. Article 5: MISSTATEMENT OF AGE Should the age of an Insured Employee exceed that stated in the application, this Policy shall not be void but there shall be an equitable adjustment. If the Misstatement of Age does not alter in any way the outcome of a claim submitted, then the Benefits shall remain unchanged; but if the change in age effects such, then these shall be corrected accordingly and a premium adjustment shall take such corrections into account with effect from inception. With respect to the calculation of age for the calculation of the premium to the policy, in the case where only the year of birth of the insured member is indicated the day of birth shall be considered as the 01st of January of the year indicated as that of birth. Article 6: CONTRACT VALIDITY The validity of this Contract (in regard to each Product selected) begins at the Effective Date and terminates at the Expiration Date as specified in the Contractual Schedule. However, each Beneficiary is covered under this Contract as from his Enrollment Date as specified under the Contract Schedule and/or any related Endorsement up to the Expiration Date of this Contract. Article 7: APPLICATION FORM This Contract and its related Endorsements have been issued by the Insurer on the basis of the Policyholder ’s declarations. The Insurer reserves the right to reject any Subsequent Application that is not in conformity with the provisions of this Contract. Article 8: REPRESENTATION CLAUSE In the event that the Policyholder has provided and confirmed directly or through its appointed insurance representative, a claims experience on the basis of which the company has calculated the premium relating to this contract, the Policyholder takes note that the company reserves the right to amend the premium of this contract, retro-actively form the effective date, if it has proof that the Policyholder has directly or indirectly Page 15 of 18 misrepresented the past claims experience. In such a case the Policyholder acknowledge and agree that it shall be liable for such a premium revision, which payment to the company shall be subjected to the provisions under article 3. Article 9: REPORTING AND SETTLEMENT OF CLAIMS The Company, will require claim forms for filing proof of loss. The forms must be completed and returned to the Company within 7 days after the date of occurrence. Any requirements requested by the company, such as supporting documents or missing information to be provided within 7days from the date of request letter, failing which the company reserves the right to repudiate the claim. All claim forms and supporting documents to be submitted should be either in Arabic or in English. Article 10: SUBROGATION Once the Insurance Claim has been paid in accordance with the current terms, the Policyholder subrogates his/her right to the Insurer to pursue any third party responsible for an Injury the Policyholder and the Beneficiary transfer to the Insurer every relevant substantial and legal right. Both, the Policyholder and the Beneficiary shall provide the Insurer with every possible assistance in case the Insurer exercises the above right of subrogation. Should the Policyholder and the Beneficiary breach this obligation, they shall be responsible for any losses incurred by the Insurer. Article 11: Contribution If any claim covered by the scope of cover of this Policy is also covered by any other Contract of Cover also simultaneously active at the time of occurrence then this Policy shall not be liable to contribute more than its rateable proportion of any payment in respect of such claim. Article 12: ARBITRATION All differences arising out of this Contract shall be referred to the decision of an Arbitrator to be appointed in writing by the parties in difference or if they cannot agree upon a single arbitrator to the decision of two Arbitrators, one to be appointed in writing by each of the parties, or in case the Arbitrators do not agree of an Umpire appointed in writing by the Arbitrators before entering upon the reference. The umpire shall sit with the Arbitrators and preside at their meetings and the making of an award shall be a condition precedent to any right of action against the Company. If the Company shall disclaim liability to the Beneficiary, his/her legal personal representatives or any Claimant for any Claim here under and such Claim is not within 12 calendar months from the date of such disclaimer referred to Arbitration under the provisions here in contained, then the Claim for all purposes shall be deemed to have been abandoned and shall thereafter not be recoverable here under. Article 13: MISREPRESENTATION, ERRORS AND OMISSIONS The Company shall not be liable under the policy in the event of any misrepresentation or nondisclosure by the Insured of any material information at any time during the currency of the Policy. Furthermore it is to be noted that the issue of this Policy Document is effected under the Company's part and obligation towards the governance of utmost good faith. Hence it is to be understood that due care and diligence have been employed in the issue of such Contract. Thus it shall be the onus and responsibility of the Policyholder and/or the Insured to ensure that all facts, circumstances, terms and limitations enlisted under this Contract are as per the agreements intended to be entered into between all Parties to such Contract. Failure to indicate any Errors and Omissions from the part of the Policyholder following the issue of this Contract shall not bind the Company towards any liability arising therefrom. Article14: FORFEITURE If the insured shall lodge any claim or connive in the making of any claim, knowing the claim to be false or fraudulent, the policy shall become void and all claims will stand forfeited. Article 15: WRITTEN COMMUNICATION Page 16 of 18 Any notice and/or other communication to the Company relevant to the Cover as afforded by this Contract of Cover or towards the maintenance of same or claims submitted must be submitted in writing or in printed form and addressed/delivered to the Company at the indicated correspondence channels of same. Article 16: CHANGE OF LAW This Contract is intended to conform to the law of the country in which the Insurer home office is located. if a conflict arises between this Contract and such law becomes effective after the Contract Effective Date, the Insurer may, at its own option, re-negotiate the terms of this Contract from the date such law becomes effective. Article 17: DUTIES Any levies on the Contract, tax or stamp duty shall be borne exclusively by the Policyholder. Page 17 of 18 USERS’ GUIDE Union Insurance Company PSC is pleased to provide you the following guide pertaining to your health insurance benefits. Reimbursement through Union Insurance Company PSC can be obtained through the following: - Your Doctor must complete a reimbursement form. Original itemized invoices and receipts of payment for all expenses must be obtained. Detailed medical reports and results must be obtained including: surgical reports, if any/ discharge summary of inpatient/ lab results/ radiology reports/ prescription copies. Police reports for all RTA claims Passport copy with legal entry stamp date and insurance certificate. The above must be submitted to our office maximum of 7 days of hospital discharged. Page 18 of 18