P3 SS Chest pain -2
advertisement

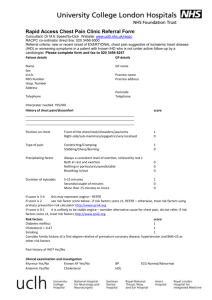
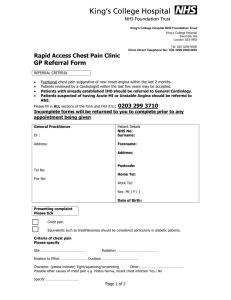
Chest Pain Clinical definition There are many different types of chest pain. These reflect the different associated underlying organs and their pathologies. More than one cause may be present in the same patient and one source or its treatment may trigger another. Clinical Relevance Chest pain is very common. It is responsible for up to fifteen admissions per day to Ninewells Hospital. Myocardial infarction is now the most common causes of death in the UK and other developed countries. Pneumonia, another cause of chest pain, is an important cause of death in the over 70 age group. It may be associated with serious pathology, where medical intervention is required; for example, pain in the chest is the most common symptom associated with ischaemic heart disease. There are a number of causes which may need to be differentiated if the patient is to be managed appropriately. Pain in the chest may present as an emergency where immediate action is required to treat the underlying pathology. The priority is to differentiate acute myocardial infarction, unstable angina and pulmonary embolism from other causes of chest pain. These are potentially fatal conditions whose course may be modified by appropriate early treatment. Angina often presents in an atypical way as a tightness or heaviness. Elderly patients can be very vague in the descriptions of their symptoms. Additionally, patients may present with chest pain in a number of situations such as postoperatively or associated with another illness such as a malignancy. It is important that you can assess how to manage chest pain in various settings and appreciate the potential urgency of the management. Clinical Presentation There are several types of chest pain and they may present in the following ways: Description Tight crushing chest pain Most Likely Source of Pain Heart Sharp pain worse on a deep Pleura breath Burning pain relieved by food Lateral localised chest pain worse on pressing ribs Oesophagus stomach or duodenum Musculoskeletal Common Conditions Responsible Myocardial infarction Unstable angina Angina Pneumonia Pleurisy Pulmonary embolism Reflux oesophagitis Peptic ulcer Muscular strain Fractured ribs Trauma Priorities in assessing the patient with chest pain One of the key priorities in assessing a patient with chest pain is to establish the aetiology of the pain as the pain may be life threatening. This may not always be initially possible from clinical history and simple investigations may need to be considered. Usually an electrocardiogram can assist in the evaluation of chest pain. However, the situation may vary in individual patients and can be complex when patients have had several episodes of pain. Usually when the implications of the pain are unclear, the patient is admitted for a short period of observation. What investigations may be performed? FBC,U/E, glucose, Thyroid function Electrocardiogram Troponin Chest X Ray Echocardiogram Nuclear Medicine Scan (Myocardial Scintigraphy or Lung Ventilation Perfusion Scan) Exercise Electrocardiography Coronary Angiography What are the key differential diagnoses? Myocardial Ischaemia (with or without infarction) Reflux Oesophagitis Musculoskeletal Chest Pain Pulmonary Thromboembolic Disease What is the modern management of Chest pain? The initial management requires immediate identification of those patients with myocardial infarction with transfer to a coronary care unit where appropriate. Other less severe forms of chest pain are often managed in a rapid access chest pain clinic where the various differential diagnoses can be considered and managed in an appropriate way. Where a patient has a clear myocardial infarction, aspirin should be administered and the patient transferred to a coronary care unit for immediate thrombolysis if indicated. Additional specialist investigations may be performed depending on the clinical condition of the patient. Where the chest pain is not as a result of a myocardial infarction, the patient should be observed and additional investigations should be considered to diagnose the underlying cause of the patient’s symptoms. For example, this may include arranging an endoscopy for patients with symptoms more suggestive of oesophagitis. What Should I Do and what practical procedures should I be able to do ? By the end of Phase 3 you should be able to: Take a full history from a patient with chest pain Undertake a physical examination Differentiate between different causes of chest pain in an individual patient Interpret the meaning of cardiac enzyme estimations. Be aware of which investigations are indicated with a view to differentiating the various causes of chest pain. Understand the changes of the ECG in ischaemia Interpret a Chest X-Ray and learn to identify a normal appearance and common abnormalities such as pulmonary oedema, consolidation or pneumothorax. Understand the appropriate management for each cause of chest pain. Communicate the diagnosis, treatment and future course to the patient and family. Communicate appropriate life style advice. Prioritise the urgency of referral, investigation and treatment of different causes of chest pain. To help you achieve this here are some tasks to carry out during Phase 3 In myocardial pain you should see an electrocardiograph (ECG) being performed and eventually carry out the ECG yourself. You should be capable of identifying: a definite myocardial infarction (MI) on the ECG - (an inferior MI and an anterior MI) common arrhythmias’ e.g. atrial fibrillation - (ventricular tachycardia and ventricular fibrillation) 2nd and 3rd degree heart block. You will find good examples of these in the ECG Made Easy, J R Hampton, Churchill Livingstone. In acute coronary syndrome the investigations are for a myocardial infarction. You should know how to differentiate these conditions and the appropriate treatment. The key difference in treatment is that an STelevation MI requires treatment with thrombolysis. You should be aware of the contraindications of thrombolytic therapy. Angina. The investigations are the same as those for an MI. The key management differences is that the patient can be sent home when pain free. Angina patients should have their future risk stratified by an exercise test or a radionuclide scan. They may also require coronary angiography. Pleuritic chest pain. You should clerk in at least 1 patient with pleuritic chest pain and interpret your findings on examination. A CXR is crucial. It is often clear in pulmonary embolism and pleurisy and shows consolidation in pneumonia. You should be able to recognise a localised abnormality on chest x-ray, make a differential diagnosis and suggest further investigations. Look at Cuschieri et al P331 and P349 for further information. If the history is suggestive of PE (post op, history of malignancy, haemoptysis, DVT present) a ventilation perfusion lung scan should be performed. You should be able to interpret the significance of findings on a ventilation/perfusion scan. Out of hours as a house officer if you are convinced this is a likely diagnosis, you should initiate heparin therapy and do the scan later. You should understand the advantages and disadvantages of using low molecular weight heparin.Oesophageal pain. Oesophageal pain is diagnosed by the characteristic history and confirmed by endoscopy, manometry, PH monitoring or contrast radiology. It is important to differentiate cardiac and pleuritic pain from oesophageal pain as if untreated, the first two may have fatal consequences. Additionally heparin/aspirin could have dire consequences in peptic ulceration. Musculoskeletal pain. Diagnosed from the history and from springing the ribs. The treatment is non-steroidal anti-inflammatory drugs (NSAIDs). A chest x-ray should identify bone causes of chest pain and these should be further investigated e.g. with a bone scan. Where Can I Learn About Chest Pain? You are likely to meet patients with chest pain in the following Phase 3 Blocks: A & E department, Ward 15 (acute medical ward), Coronary care unit, Medical wards (wards 1-6), Post op surgical ward and Cardiology outpatient department. You may also meet patients with chest pain during community attachment. Severe unrelenting chest pain despite analgesia requires urgent referral. When MI, PE and unstable angina are suspected, urgent referral is required as with chest pain after trauma. Musculoskeletal and oesophageal pain do not require the same urgency. Advanced age should not be a barrier to this policy. It will also be one of the topics in your preparation for house officer block What is the potential Surgical Managment of Patients with chest pain ? Patients with chest pain and associated 3 vessel coronary artery disease are often managed surgically after evaluation of the coronary anatomy. You should understand the various investigations patients may undergo and how patients are evaluated for coronary artery bypass surgery. In addition to the surgical management, you should know how to advise patients to modify their lifestyle by giving up smoking and participating in regular exercise. What are the rehabilitation considerations for the patient with Chest Pain ? The important aspects include regular exercise and cessation of smoking. Various patient support groups and classes encourage patients to adopt a healthy lifestyle which is an important aspect of treatment as well as pharmacological therapy. What drug treatments are available for patients with chest pain ? The treatments may vary depending on whether the patient has angina or a myocardial infarction. Aspirin, clopidogrel, oral nitrates, B blockers, ACE inhibitors may be used depending on individual patient characteristics. Thrombolytic therapy is recommended in patients with ST elevation myocardial infarction. Recommended Reading There are good descriptions of different types of chest pain in your standard texts: Clinical Medicine by Kumar and Clark (6th edition). Elsevier Saunders, 2005. Davidson’s Principles and Practice of Medicine (20th edition). Churchill Livingstone, 2006. Clinical Surgery (2nd edition). Rowley. Blackwell, 2003. Cuschieri, Grace, Darzi, Borley and Additional information may be obtained via SIGN guidelines 93-7 February 2007. Look up the references noted below. Cause of Chest Pain Angina pectoris Acute coronary syndrome Myocardial infarction Pulmonary embolism Pneumonia Pleurisy Oesophagitis, Gastrooesophageal reflux disease Musculoskeletal Further Description Kumar and Clark P732 Kumar and Clark P808; European Society for Cardiology Acute Coronary Syndrome Guidelines 2007 (on Blackboard, particularly Figs 1 and 14) Kumar and Clark P812 Kumar and Clark P844 Kumar and Clark P922 Kumar and Clark P952– relevant pages Kumar and Clark P277 Kumar and Clark P547 Chest Pain Problem as seen by the Doctor Problem as experienced by your patient System links _____________________ Cardiovascular/Respiratory Gastroenterology/Musculoskeletal What a doctor will be able to do: 1 What aspects of the history and examination in a patient with chest pain help you reach a likely diagnosis to explain the patient’s symptoms? 2 The following are suggested procedures you should be familiar with: CPR Venous Access Electrocardiography What routine investigations are performed in patients who present with chest pain ? 3 4 What are the current guidelines on indication and contraindication for the use of thrombolytic therapy? 5 What issues are important in preventing patients developing myocardial chest pain ? How might patients and their families be educated to prevent them developing coronary artery disease ? What treatments are used in the secondary prevention of myocardial infarction ? 6 How was discussion of the following issues dealt with in talking with the patient and his/her family? Driving Healthy lifestyle changes Stopping smoking What evidence is there for lipid lowering, and for control of blood pressure in the prevention of secondary cardiovascular disease? 7 How a doctor approaches their practice: 8 What are the underlying pathophysiological processes that give rise to the symptom of chest pain in patients who have ischaemic heart disease ? 9 What, if any, are the legal problems in relation to driving? 10 How would you differentiate serious causes of chest pain from the majority of non-serious causes presenting in a primary care setting? Doctor as a professional: 11 12 What were the doctor’s responsibilities in relation to other healthcare providers? Early management of your patient in the Community regarding diagnosis of MI and thrombolysis Initial management in hospital How would you organise an audit of patients receiving thrombolytic therapy ? APPROACHING THE CORE CLINICAL PROBLEM Chest pain Clinical Assessment : Onset, site, character, precipitating factors, relieving factors, nature of the pain. Associated arm pain, vomiting, dizziness. Investigations : Electrocardiogram, Troponin, FBC, U/E, Chest X Ray. Exercise Electrocardiography. Specialist investigations. Differential Diagnoses : Myocardial Ischaemia, Reflux Oesophagitis, Musculoskeletal pain, pulmonary thromboembolic disease. Treatment : Thrombolysis for myocardial infarction, H.Pylori eradication for gastrooesophageal disease, anticoagulation for pulmonary thromboembolic disease. APPROACHING THE CORE CLINICAL PROBLEM Clinical Definition Clinical Relevance Clinical Presentation Priorities in assessing the patient with the CCP What investigations would you perform ? What are the main differential diagnoses ? What is the modern management of the Core Clinical Problem? What are the Medical and Surgical Options for the management of the core clinical problem ? What issues are relevant for the rehabilitation of the patient with the core clinical problem ? What is the recommended drug treatment for the core clinical problem ? Linkage of the Core Clinical Problem to the 12 Curriculum Outcomes. June 2008 Dear We are presently in the process of updating the study guides and the approach to the core clinical problems. In the new curriculum the approach continues to be task based and for phase 3 students, there is an emphasis on developing diagnostic reasoning skills and considering aspects of patient management in more detail. Enclosed are 2 of the core clinical problems which include a task based approach to the assessment, diagnosis and treatment of the core clinical problems. I would be grateful if you could update your present study guide for the core clinical problems associated with your system. A template is enclosed with areas which we would like to include in the upgraded study guides. When reviewing and updating your study guide, we would be grateful if you would consider this approach to facilitate a streamlined evaluation of the core clinical problems. As ever, the schedule is fairly tight. As a result, I would be grateful if you could send back your revised study guide by the ..... This will enable them to be made available to the students for the next academic year. Enclosed are 2 study guide examples and the templates/headings which we plan to utilise for the core clinical problems. Thankyou for your assistance with this. Please do not hesitate to contact me directly if you need further assistance with this. Yours sincerely Neil Gillespie Senior Lecturer in Medicine (Ageing & Health).