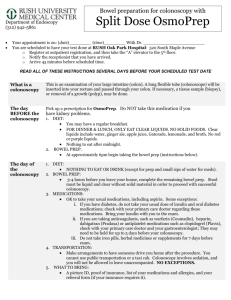
For patients taking TriLyte: (reduced volume)
advertisement

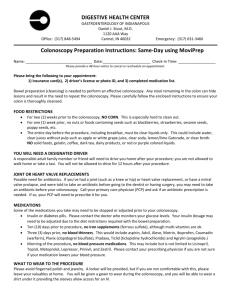
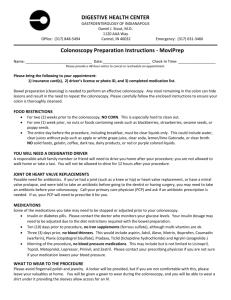
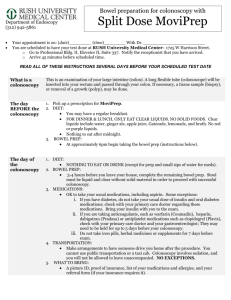
GASTRO ASSOCIATES Mukul Khandelwal MD and Mahmood Solaiman MD Gastroenterology & Hepatology 8109 Ritchie Highway Pasadena, MD 21122 & 8186 Lark Brown Road, Ste. 104, Elkridge, MD 21075 Phone: (410) 590-8920 FAX: (410) 553-2345 __________________www.mdgastro.net________________ Understanding Colonoscopy WE PROVIDE FOUR CHOICES FOR PREPARATIONS. THE FIRST, THIRD, AND FOURTH CHOICES REQUIRE PRESCRIPTIONS. PREPARATION #3 SHOULD NOT BE USED IF YOU HAVE HEART OR KIDNEY DISEASE. IF YOU WISH TO TAKE THE OSMOPREP PILLS, PLEASE CALL OUR OFFICE SO THAT WE CAN CALL IN A PRESCRIPTION. ALL OF THESE PREPARATIONS ARE EQUALLY EFFECTIVE, BUT THERE COULD BE INDIVIDUAL DIFFERENCES IN EFFECTIVENESS JUST AS THERE ARE WITH ANY MEDICATION. What is a colonoscopy? Colonoscopy enables your doctor to examine the lining of your colon (large intestine) for abnormalities by inserting a flexible tube as thick as your finger into your anus and slowly advancing it into the rectum and colon. If your doctor has recommended a colonoscopy, this brochure will give you a basic understanding of the procedure - how it's performed, how it can help, and what side effects you might experience. It can't answer all of your questions since much depends on the individual patient and the doctor. Please ask your doctor about anything you don't understand. What preparation is required? Your doctor will tell you what dietary restrictions to follow and what cleansing routine to use. In general, the preparation consists of either consuming a large volume of a special cleansing solution and clear liquids and special oral laxatives. You must drink plenty of Gatorade type liquids on the day before the test in addition to the preparation. The colon must be completely clean for the procedure to be accurate and complete, so be sure to follow your doctor's instructions carefully. Can I take my current medications? Most medications can be continued as usual, but some medications can interfere with the preparation or the examination. Inform your doctor about medications you're taking, particularly aspirin products, arthritis medications, anticoagulants (blood thinners), insulin or iron products. Please take all blood pressure medications on the morning of the procedure. Also, be sure to mention allergies you have to medications. It is not recommended to take antibiotics if you have mitral valve prolapse or joint replacement. What happens during colonoscopy? Colonoscopy is well tolerated and rarely causes much pain. You might feel pressure, bloating or cramping during the procedure. Your doctor will give you a sedative to help you relax and better tolerate any discomfort. You will lie on your side or back while your doctor slowly advances a colonoscope through your large intestine to examine the lining. Your doctor will examine the lining again as he or she slowly withdraws the colonoscope. The procedure itself usually takes 15 to 60 minutes, although you should plan on two to three hours for waiting, preparation and recovery. In some cases, the doctor cannot pass the colonoscope through the entire colon to where it meets the small intestine. Although another examination might be needed, your doctor might decide that the limited examination is sufficient. What if the colonoscopy shows something abnormal? If your doctor thinks an area needs further evaluation, he or she might pass an instrument through the colonoscope to obtain a biopsy (a sample of the colon lining) to be analyzed. Biopsies are used to identify many conditions, and your doctor might order one even if he or she doesn't suspect cancer. If colonoscopy is being performed to identify sites of bleeding, your doctor might control the bleeding through the colonoscope by injecting medications or by coagulation (sealing off bleeding vessels with heat treatment). Your doctor might also find polyps during colonoscopy, and he or she will most likely remove them during the examination. These procedures don't usually cause any pain. What are polyps and why are they removed? Polyps are abnormal growths in the colon lining that are usually benign (noncancerous). They vary in size from a tiny dot to several inches. Your doctor can't always tell a benign polyp from a malignant (cancerous) polyp by its outer appearance, so he or she might send removed polyps for analysis. Because cancer begins in polyps, removing them is an important means of preventing colorectal cancer. How are polyps removed? Your doctor might destroy tiny polyps by fulguration (burning) or by removing them with wire loops called snares or with biopsy instruments. Your doctor might use a technique called "snare polypectomy" to remove larger polyps. That technique involves passing a wire loop through the colonoscope and removing the polyp from the intestinal wall using an electrical current. You should feel no pain during the polypectomy. What happens after a colonoscopy? Your physician will explain the results of the examination to you, although you'll probably have to wait for the results of any biopsies performed. You must arrange for someone to drive you home and stay with you. Even if you feel alert after the procedure, your judgment and reflexes could be impaired for the rest of the day. You might have some cramping or bloating because of the air introduced into the colon during the examination. This should disappear quickly when you pass gas. You should be able to eat after the examination, but your doctor might restrict your diet and activities, especially after polypectomy. What are the possible complications of colonoscopy? Colonoscopy and polypectomy are generally safe when performed by doctors who have been specially trained and are experienced in these procedures. One possible complication is a perforation, or tear, through the bowel wall that could require surgery. Bleeding might occur at the site of biopsy or polypectomy, but it's usually minor. Bleeding can stop on its own or be controlled through the colonoscope; it rarely requires follow-up treatment. Some patients might have a reaction to the sedatives or complications from heart or lung disease. Although complications after colonoscopy are uncommon, it's important to recognize early signs of possible complications. Contact your doctor if you notice severe abdominal pain, fever and chills, or rectal bleeding of more than one-half cup. Note that bleeding can occur several days after polypectomy. To The Patient Because education is an important part of comprehensive medical care, you have been provided with this information to prepare you for this procedure. If you have questions about your colonoscopy, alternative tests, the cost of the procedure, methods of billing, or insurance coverage, do not hesitate to speak to your doctor or your office staff. Most endoscopists are highly trained specialists and welcome your questions regarding their credentials and training. If you have questions that have not been answered, please discuss them with the endoscopy nurse or your physician before the examination begins. My Colonoscopy is scheduled for: Place:________________________________________________ Date:_________________________________________________ Arrival Time:____________ Procedure Time:_________________ Colonoscopy Preparation: All patients drink clear liquids the entire day before the exam. If you have a procedure scheduled in the morning, please do not take anything by mouth except for medications. If your procedure is scheduled from 12 noon and afterwards, you may have a very light clear liquid breakfast before 7 AM. Please do not take dairy products or coffee in the morning. Please do not drink anything red. It dyes your colon red and looks like there has been bleeding. Morning of the exam: You may take your regular medications unless instructed otherwise by your doctor. If you take insulin, take half your nighttime dose, the night before the colonoscopy, and do not take your insulin on the morning of your procedure. If you are taking pills for your diabetes, do not take that medication on the morning of your procedure. Preparation 1: For patients taking TriLyte: (reduced volume) Items needed: 1. Small box of Dulcolax/bisacodyl (no prescription needed, store brand is fine). You will need 2 Dulcolax/bisacodyl. 2. One container of Trilyte (prescription attached) Follow this schedule: 1. The day before the exam: Drink Clear liquids the entire day. 2. At 4 PM, take 2 bisacodyl tablets with water. Do not crush or chew. 3. Mix the TriLyte with water. Fill to the “Fill line” or 4-liter mark on the container. You may add a flavor pack of your choice to the solution. Refrigerate after mixing. 4. Between 4 pm and 9 pm, begin drinking TriLyte. ONLY DRINK HALF OF THE CONTENT IN THE CONTAINER. YOU SHOULD FINISH AT THE 2 LITER MARK ON THE BOTTLE. Remember you have 5 hours to drink the solution. If you start feeling nauseated please stop for one hour, and then try to restart. If you are unable to restart, please follow the secondary prep enclosed in this packet. IF YOUR BOWEL MOVEMENT IS NOT COMPLETELY CLEAR AFTER THE PREPARATION, THEN CONTINUE DRINKING THE SOLUTION UNTIL YOU ARE CLEAR. 5. Approximately 9pm: You should be finished with your TriLyte. Drug interactions: Oral medications taken within one hour of the start of administration of the TriLyte may be flushed from the gastrointestinal tract and not absorbed. Recommend: After you have mixed the TriLyte you may wish to drink it with ginger ale on ice to help the taste. Colonoscopy Prep for patients that cannot finish TriLyte: (If you have started TriLyte and cannot finish it) 1. Begin TriLyte at 4 pm the day before the colonoscopy. Stay on clear liquids the entire day before the procedure. 2. If you develop nausea or vomiting from TriLyte, Please go to the pharmacy and take the following: Magnesium citrate take 1 bottle at 4 p.m., 7 p.m., and 9 p.m. or any time afterward to clean yourself out. You may mix with ginger ale and keep chilled for improved taste. Alternative Preparation #2 for patients not taking TriLyte: (Instead of TriLyte Preparation) These can be obtained over the counter from any pharmacy. 1. Clear Liquids the day before the examination. 2. Drink 1 bottle of magnesium citrate each at 4pm, 7pm and at 9pm the day before the examination. You may mix with ginger ale and keep chilled for improved taste. Alternative Preparation #3 for patients taking Osmoprep tablets THIS SHOULD NOT BE USED FOR PATIENTS WITH CONGESTIVE HEART FAILURE OR RENAL FAILURE 1. Take clear liquids the day before the procedure and drink plenty of liquids. 2. Starting at 4 PM the day before the procedure, take 4 tablets of Osmoprep with at least 8 oz of clear liquids every 15 minutes for a total of 20 tablets. 3. Starting at 7 PM, take 4 tablets of Osmoprep with at least 8 oz of clear liquids every 15 minutes for a total of 12 tablets. Alternative Preparation #4 using MoviPrep 1. Take clear liquids the day before the procedure. 2. The MoviPrep carton contains 4 pouches and a disposable container for mixing. You must complete the entire prep to ensure the most effective cleansing. If preferred, mix the MoviPrep solution ahead of time and refrigerate prior to drinking. (The mixed MoviPrep solution should be used within 24 hours) 3. First prepare the MoviPrep solution. Empty 1 pouch A and 1 Pouch B into the disposable container. Add lukewarm drinking water to the top line of the container. Mix to dissolve. You may wish to chill the preparation after dissolving. 4. At 4 pm begin drinking the solution. YOU may wish to add Ginger Ale to help with the taste. The MoviPrep container is divided by 4 marks. Every 15 minutes, drink the solution down to the next mark (approximately 8 oz), until the full liter is complete (at approximately 6 pm). Now drink 16 oz of the clear liquid of your choice. 5. At 6 pm repeat step # 2, and refrigerate if preferred. 6. At 7:00 pm begin drinking the solution. Every 15 minutes, drink the solution down to the next mark (approximately 8 oz.), until the full liter is complete. You may continue to drink clear liquids until midnight, then NOTHING AFTER MIDNIGHT except medications if your procedure is before 12 Noon. If your procedure is scheduled from 12 noon and afterwards, you may have a very light clear liquid breakfast before 7 AM. Please do not take coffee or dairy products in morning. DRS. KHANDELWAL OR SOLAIMAN WILL WRITE THE FINDINGS ON THE DISCHARGE SHEET AND DISCUSS THE FINDINGS WITH YOUR DESIGNATED DRIVER AND YOURSELF. PLEASE UNDERSTAND THAT YOU MAY NOT REMEMBER THE DISCUSSION WITH THE DOCTOR BECAUSE OF THE SEDATIVES THAT ARE ADMINISTERED DURING THE PROCEDURE. IF YOU HAVE QUESTIONS ABOUT THE RESULTS, PLEASE CALL THE OFFICE. THE WEEK BEFORE THE PROCEDURE No aspirin or aspirin like products like naprosyn, motrin, excedrin. You may take Tylenol or Celebrex or Vioxx. The day before the procedure, please avoid dairy products and red juices. You may take non-dairy creamer at least 6 hours before procedure. THINGS THAT YOU MAY EAT THE DAY BEFORE THE PROCEDURE Jellos (not red jello) Popsicle Freeze Pop Chicken Broth Beef Broth Vegetable Broth 7-UP Sprite Ginger Ale Coke Tea Black Coffee Orange Juice Gatorade Apple Juice All patients drink clear liquids the entire day before the exam. The list of liquids is at the back of this form. If you have a procedure scheduled in the morning, you should not eat or drink after midnight except for medications. If your procedure is scheduled from 12 noon and afterwards, you may have a very light clear liquid breakfast before 7 AM. Please do not take coffee or dairy products in morning.