FEB: 09/01 - MyM Supply
advertisement

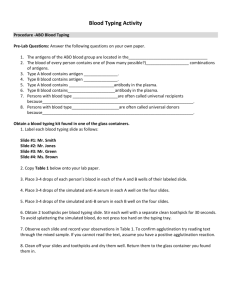
FEBRILE ANTIGENS INTENDED USE SPECIMEN COLLECTION AND PREPARATION MYM Febrile Antigens are bacterial suspensions for use as an aid in the diagnosis of certain febrile diseases such as brucellosis, rickettsial, and salmonellosis diseases. These bacterial suspensions may be used in either slide (qualitative) or tube (semi-quantitative) agglutination tests to detect for the presence of bacterial agglutinins (antibodies) associated with bacterial infections. 1. 2. 3. 4. Collect 5 - 10mL whole blood samples aseptically from the patient. Allow blood to clot and remove serum as soon as possible to prevent excess hemolysis. If the serum is turbid or contains erythrocytes, centrifuge to clarify. Store serum at 2 - 8°C until testing can be performed. Do not heat the serum since significant antibodies may be thermolabile. SUMMARY Titration of patient’s antibodies by agglutination of known bacteria suspensions has proven to be of value in the evaluation of certain diseases. The classic example is the Widal test. This method is based upon the identification of the greatest dilution of the patient’s serum, which will cause agglutination of a known bacterial suspension, which was prepared in a standard way1. Antibodies produced as a response to a “febrile” infection can be detected in a similar fashion. The term “febrile” is associated with a number of organisms, which produce a fever in the host. PRINCIPLES OF THE TEST In the course of human infection with any pathogenic microbiological agent, a variety of antibodies are formed. Among these antibodies are the agglutinins. An agglutinin, when combined with homologous antigen (agglutinogen) under properly controlled conditions, is capable of causing agglutination. For example, a suspension of Brucella abortous possessing active antigen, will agglutinate when exposed to homologous brucella antibody. This agglutination forms clumps of bacteria, which become macroscopically visible. REAGENTS MYM Febrile Antigens: Brucella Antigens Francisella tularensis Antigen Proteus Antigens Salmonella H Antigens Salmonella O Antigens Brucella Abortus Antiserum Brucella Melitensis Antiserum Brucella suis Antiserum Brucella Poly Antiserum Francisella tularensis Antiserum Proteus OX2 Antiserum Proteus OX19 Antiserum Proteus OXK Antiserum Proteus Poly Antiserum Salmonella O Poly Antiserum Salmonella H Poly Antiserum Salmonella Vi Antiserum Febrile Positive Control Febrile Negative Control MATERIALS REQUIRED BUT NOT PROVIDED For Slide Tests Applicator sticks or wooden toothpicks, Glass slides, Light source, Pipettes, Wax pencil MYM Febrile Antigens can be used in testing either with the slide agglutination test or the tube agglutination test. The rapid slide test is recommended as a screening procedure only to establish the presence or absence of homologous antibody. The tube test establishes antibody titer and verifies results found using the slide method3. For Tube Test Glass dilution flask, Light source, Pipettes, Water bath, Test tubes, Test tube rack, Sodium chloride (0.85% NaCl, no preservatives). PRECAUTIONS All antigens, antisera and test sera should be at room temperature before testing. 1. 1. 2. 3. 4. 5. 6. 7. 8. 9. For greater proficiency in test interpretation, always include positive and negative control sera as well as a saline control in each test batch. All sera and antisera to be tested should be clear and free from bacterial contamination and unheated. If not, centrifuge to clarify. Mix antigen vial well before use to ensure a smooth, uniform suspension. Do not use antigens, which fail to give a uniform suspension after gentle mixing, or which produce agglutination in the saline control. Specimens found reactive using the slide procedure should be verified and checked for titer using the table test procedure. 3 In some cases, sera may demonstrate a prozone (inability of an antigen to react in higher serum concentrations). It is advised that all 5 sera volumes be used in the rapid slide test procedure (rather than just 1 volume) to eliminate the possibility of missing positive reactions due to prozone. All specimens should be considered potentially hazardous and handled in the same manner as an infectious agent. The color intensity of the antigen suspension may vary from lot to lot. This variance is normal and will not affect test results. All Brucella, Proteus, and Salononella O antigens contain 0.5% phenol. In case of contact with eyes and skin, immediately flush with water for at least 15 minutes. In case of eye contact, call a physician. Wash clothing before reuse. Use only with adequate ventilation. Salmonella H Antigens contain 0.5% formalin, which may cause cancer. Repeated or prolonged exposure increases the risk. In case of contact with eyes or skin, immediately flush with water for at least 15 minutes. In case of eye contact, call a physician. Wash clothing before reuse. Use only with adequate ventilation. SLIDE TEST PROCEDURE (Qualitative) 2. 3. 4. 5. 6. 7. Obtain a clear, transparent glass slide and divide it into 1 1/2 inch squares with a wax pencil. A small windowpane can be used for this purpose. Using a suitable pipette, add the following amounts of test sera to consecutive squares from left to right: 0.08ml; 0.04ml; 0.02ml; 0.01ml; 0.005ml. Serum should be clear and unheated. Repeat this procedure with febrile positive and negative control sera. Mix the antigen bottle gently to insure a uniform suspension. Add one drop of antigen suspension just below each quantity of serum. Mix the test serum and antigen composites using a piece of applicator stick or toothpick. Use separate applicator sticks for each specimen mixture. Gently rock the slides back and forth for one minute. Observe for agglutination using a good indirect light against a dark background. INTERPRETATION OF SLIDE TEST RESULTS The degree of agglutination is recorded as follows: 4+ 100% of the organisms are agglutinated 3+ 75% of the organisms are agglutinated 2+ 50% of the organisms are agglutinated 1+ 25% of the organisms are agglutinated Neg. No agglutination is observed Positive Results - are reported if at least 2+ (50%) agglutination is observed at any serum volume. STORAGE Negative Results - are reported if agglutination is less than 2+ (50%) in all serum volumes. All febrile antigens and control sera must be stored at 2 - 8°C when not in use. Bring reagents to room temperature (20 - 30°C) before use. Do not freeze. Stability of Reactions in the Slide Test- The Slide Test should be read at one minute. Reactions occurring later may be due to components drying on the slide. TUBE TEST PROCEDURE (Semi-Quantitative) 2. All antigens, antisera and test sera should be at room temperature before testing. 3. 1. 2. 3. 4. 5. 6. 7. 8. Re-suspend the antigen by gentle swirling the vial. Prepare a 1:50 dilution in 0.85% sodium chloride solution. Place ten test tubes (13x100mm) in a test tube rack. Add 0.9ml of 0.85% sodium chloride solution to the first tube. Add 0.5ml of 0.85% sodium chloride solution to the remaining tubes. Add 0.1ml of the serum to be tested to the first tube. Mix well and transfer 0.5ml of the diluted serum to the second tube. Mix well and transfer 0.5ml of the diluted serum from the second tube to the third tube. Repeat this procedure until all 10 tubes contain serial two-fold serum dilutions from 1:10 through 1:5120. Remove 0.5ml of diluted serum from tube 10 and discard. Repeat this procedure with positive and negative control sera. Place one empty tube at the end of the series of dilution tubes and add 0.5ml of the 0.85% sodium chloride solution. Label the tube, “Saline Control.” Add 0.5ml of the diluted antigen to all tubes. (Final serum dilutions will be 1:20 through 1:10240). Shake the rack well to mix the antigen and serum and place in a water bath. Recommended time and temperature of incubation are shown below. Antigen Brucella antigens F. tularensis antigen Proteus antigens Salmonella O antigens Salmonella H antigens 9. Temperature 37°C 37°C 45-50C 45-50°C 45-50°C Time of Incubation 20-24 hours 20-24 hours 18 hours 16-18 hours 1 hour After incubation, carefully remove the test tube rack with the test tubes and observe for agglutination. The use of indirect light source against a black background will give optimal conditions for reading the tube tests. INTERPRETATION OF TUBE TEST RESULTS The degree of agglutination is recorded as follows: 4+ All organisms appear agglutinated on the bottom of the tube and supernatant fluid is clear. 3+ 75% of organisms are agglutinated and supernatant fluid is slightly cloudy. 2+ 50% of organisms are agglutinated and supernatant fluid is moderately cloudy. 1+ 25% of organisms are agglutinated and supernatant fluid is cloudy. Neg. No agglutination is observed and suspension appears turbid. The titer of the serum is recorded as the last dilution of the specimen in which at least a 2+ (50%) agglutination occurs. 4. 5. 6. 7. Reporting results from a single specimen is of no clinical use because of possible heat exposures, cross-reactions or interfering substances. Results should not be used as a complete substitute for conventional isolation and serological identification of the etiologic agent. Isolation of the organism is required for definitive diagnosis. This test provides a presumptive diagnosis. Brucella abortus, Brucella melitensis, and Brucella suis are antigenically related and will cross react. Cross-reactions may occur in certain diseases. For instance, Tularemia infections may produce agglutinins capable of reacting with Brucella antigen. Vaccinations may produce agglutinins capable of reacting with febrile antigens. Typhus vaccinations may produce antibodies to Proteus antigens and Typhoid vaccinations may give rise to antibody specific for Salmonella antigens. It is necessary to test several serum specimens from the same patient taken at different intervals to detect semi-quantitative differences in agglutinin content. A four-fold increase in titer between the acute phase specimen and a convalescent phase specimen should be completely evaluated by the physician. All clinical and laboratory results should be evaluated before making a definitive diagnosis. EXPECTED VALUES When viable bacteria invade a susceptible host, an immune response generally occurs. For example, when a human becomes infected with Salmonella, an immune response occurs which is capable of producing agglutinins. These agglutinins are capable of specifically reacting with the suspensions of Salmonella species responsible for the infection. Agglutinins are produced slowly during the acute phase of infection and continue to form during the convalescent phase of infection. The titer of antibody rises considerably between acute infection and convalescence. Therefore, a rise in titer between serum collected during the acute or febrile stage of infection and serum collected during the convalescent stage can be of diagnostic significance. The following table indicates the agglutinin titer normally expected during the course of infection with several bacterial species: Febrile Antigen used to test for Agglutinins Antibodies appear within Peak Titer appears within Significant Titer Brucellosis suis, melitensis Brucella abortus 2-3 Weeks 3-5 Weeks 1:80 Rocky Mountain Spotted Fever Proteus OX19 1-2 Weeks 2-3 Weeks 1:160 Disease Typhus Proteus OX19 1-2 Weeks 2-3 Weeks 1:160 Positive Results - report the titer as the last dilution in which at least a 2+ (50%) agglutination occurs. Paratyphoid Fever Salmonella H a 2-3 Weeks 4-5 Weeks 1:80* Negative Results - report the titer as less than 1:20. Paratyphoid Fever Salmonella H b 2-3 Weeks 4-5 Weeks 1:80* Stability of Reactions in the Tube Test The tube test should be read immediately after the incubation period. Care should be taken to avoid disturbing tubes when removing racks from water bath. Excessive shaking of the tubes may tend to disperse clumps of cells thereby giving a false negative results. Typhoid Fever Salmonella H d 2-3 Weeks 4-5 Weeks 1:80* Typhoid Fever Salmonella O Group D 1-2 Weeks 3-5 Weeks 1:80* Francisella tularensis 2 Weeks 4-8 Weeks 1:160 Tularemia QUALITY CONTROL Incorporating controls in the test procedure and obtaining the expected results confirm correct procedural technique and test performance. Each positive control contains agglutinins for the corresponding antigen and should produce agglutination. The negative control should produce negative results (no agglutination). It is recommended that when a new shipment of product is received, or when product performance are to be validated, positive and negative controls should be used. LIMITATIONS OF THE PROCEDURE 1. Detectable agglutinins are not always produced in bacterial infection. In some instances, non-specific agglutinins may appear which will react with the febrile antigens. For example, serum from acme narcotic addicts has been reported to contain significant agglutinins to the febrile antigens6. * Significant in non-vaccinated individuals The end point titer may vary (plus or minus) 1 dilution when retesting samples or when testing samples collected at different times from the same patient7. PERFORMANCE CHARACTERISTICS Febrile Antigens: The antigenicity of all febrile antigens has been verified with control antiserum of established titer. The antigens are prepared according to the guidelines outlined in Recommended Specifications for Microbiological Reagents8. Febrile Controls: The homologous antibody titer of the Febrile Controls have been verified to be reactive at the dilution representative of the significant titer of an infected individual. The Febrile Negative Control has been found to be non- reactive with B. abortus, Proteus OX19, Salmonella H a, b, d and Salmonella O Group D. BIBLIOGRAPHY 1. 2. 3. Vogel, H., el. al Am. J. Clin. Path.,53-932, (1970). Diamond, B.E., Pub. Health Lab. V6, 74, (1948). Spink, W.W., McCullough, N.B., Hutchings, L.H., Amer. J. Clin. Path., 24:486, (1954). 4. Bacterial and Mycotic Infections of Man; 2nd Edition, jRene J. Dubos, I.B. Lippincott, Philadelphia, (1952). 5. “Laboratory Techniques in Brucellosis:”, 2nd E.d Alson, G.G., et al., World Health Organization, Geneva (1975). 6. Preparation of Suspension of Proteus for the Weil-Felix Test, Rocky Mount. Lab. Hamilton, MT, Dec. (1949). 7. Quality Control in Clin. Micro., Revised, ASCP Comm. on Continuing Education, Council on Micro., (1968). 8. Recommended Specifications for Microbiological Reagents, 3rd Edition, U.S. Department of Health, Education, and Welfare, Atlanta, GA, Jan (1968). 9. Specifications and evaluation Methods for Immuno. and Micro. Reagents, Vol. 1, Bacterial Fungal, and Parasitic. 4th Ed., Centers for Disease Control, Atlanta, GA (1975). FEB: 09/01