Sample Syllabus Practicum/Fieldwork Class
advertisement

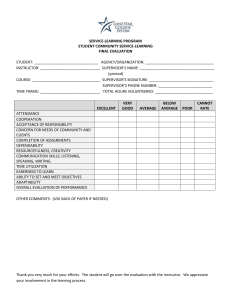
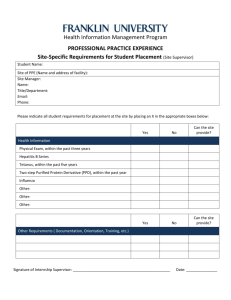
Syllabus Practicum/Fieldwork: [course number] Course Syllabus [semester and year] [course day and time] Instructor: Office: Phone: Email: Office Hours: Units: Prerequisite(s): Catalog/Course Description Course Objectives At the end of this course, students will be able to do the following: Provide competent mental health services in community mental health setting under licensed supervision. o Associated Learning Activities: Finding a field site and completing fieldwork plan; completing a minimum of ____ service hours; Fieldwork Evaluation Form at the end of the semester (to be completed by fieldwork supervisor). Effectively and professionally document psychotherapy treatment provided to clients. o Associated Learning Activities: Progress note, assessment, and treatment plan presentations Conceptualize and assess cases using a theoretical and diagnostic framework. o Associated Learning Activities: Case Presentation with case conceptualization; Assessment presentation Develop professional treatment plans for working with adults, couples, families, and children attending to diversity and ethical issues. o Associated Learning Activities: Case Presentation; Treatment plan presentation Demonstrate ability to effectively utilize supervision at field placement. o Associated Learning Activities: Fieldwork Evaluation Form at the end of the semester (to be completed by fieldwork supervisor). 1 Instructional Format This course will be conducted primarily as an experiential course designed to help you integrate your clinical experiences with your university coursework and curriculum. Thus, our goal is to bridge theory and practice. For this process to be successful, each student must participate fully by attending class, engaging in class exercises, sharing in discussions, and reading assigned materials. Required Text Gehart, D. R. (2014). Mastering competencies in family therapy: A practical approach to theories and clinical case documentation (2nd ed.). Pacific Grove, CA: Cengage/Brooks-Cole. Grading: Credit/No Credit [or describe your policy] Grading Criteria: To receive a grade of “Credit,” all of the following must be satisfactorily completed: List course requirements for the following: 1. Minimum of ____ client contact hours. 2. Membership in at least one of the following professional organizations: of AAMFT, ACA, APA, and/or NASW to provide free legal consultation on clinical cases. 3. Complete sample progress note, assessment, case conceptualization and treatment plans using field site forms and present to class (see schedule and instructions below). 4. No more than ____ absences. Forms to be turned in prior to a passing grade being issued: 5. Provide evidence of professional liability insurance in the amount of $1,000,000 per incident/$3,000,000 aggregate (or highest limit currently available). 6. Log of hours 7. Evaluation from field site supervisor 8. Trainee evaluation of field site 9. Other forms: Supervision and Legal Liability Your onsite site supervisor is your clinical supervisor and thereby assumes full legal responsibility for all of your cases; you are practicing under his/her license. When staffing cases in this class, you should bring any feedback or suggestions back to your field site supervisor for his or her approval before implementing. Your onsite supervisor is your primary supervisor, and you are legally required to follow their direction, especially as it relates to crisis, ethical, and legal issues. In situations where you have received differing recommendations for how to handle a situation from your university course instructor and onsite supervisor, you must follow the instruction of your onsite supervisor. Site Visits I will be making site visits and/or phone calls to speak with your supervisor. Students will be expected to arrange their schedules to be available for the site visit. Guidelines for Protecting Client Confidentiality 2 1. When writing progress notes, use confidential notation to refer to individual family members, i.e., AF (adult female), AM (adult male), CF16 (child female, 16 years old), CM 7 (child male 7 years old). 2. When making phone calls, please ensure that no one can overhear your conversation and that you leave a message that does not indicate that the person is seeing a counselor (unless you have their written permission to do so). If have written permission to leave a message, you should keep it brief and not indicate that the message relates to therapy, such ash, “This is Diane from CCRI or Cal State Northridge, please have Jane Smith call me back at….” 3. Students must use a password on all documents created on a computer. Computer files of documents must be deleted no later than the end of the semester unless otherwise directed by your onsite supervisor. 4. If you record sessions at your site, recordings of sessions must be erased no later than the end of the semester and must be locked at all times when not in use unless otherwise instructed by your supervisor. Policies [Sample Policies are Provide: Amend or Delete as Desired] Confidentiality In this course, you are entering an experience that involves a significant amount of selfdisclosure. Naturally, people will say things that are personally important and confidential. It is your duty to maintain confidentiality and trust. Please study the AAMFT, ACA, APA, and/or NASW ethics codes, particularly paying attention to issues of confidentiality and client's rights. As the course instructor, I have a responsibility to you to act professionally and ethically. I also have a responsibility to the university, profession, and society. Normally, these responsibilities are not in conflict, and confidentiality can be maintained. However, there are times when confidentiality can/must be broken. These times are: 1. If a class member threatens danger to him/herself, I may be required by law and/or university policy to make those limited disclosures necessary to avert that danger; 2. If a class member threatens grave bodily harm or death to another person(s), , I may be required by law and/or university policy to inform the intended victim(s) and appropriate law enforcement agencies; 3. If there is any reasonable suspicion of child abuse or neglect, I may be required by law to report it immediately to the proper authorities; 4. If, in my judgment, a class member is acting unethically or experiencing a disturbance in his/her own life to such an extent that it would hinder his/her ability to work positively with others, I may discuss the situation with the departmental [designated body] to determine what action might be appropriate. Normally, I would discuss the situation with the student before disclosing confidential information to others. 3 Attendance Students manifest their responsibility in the regularity and punctuality of their attendance. Since this course includes significant seminar and experiential components, attendance at each class meeting is mandatory. In cases of absence, any scheduled assignments are due to the professor at the beginning of class unless other arrangements have been made prior to that time. If you are absent from class, it is your responsibility to check online and with fellow classmates regarding announcements made while you were absent: this includes supplemental instructions related to assignments. You are responsible for and may be tested on any and all lecture materials presented in class that are not covered in your readings. Due Dates and Times Due dates are non-negotiable unless an extension is provided to the entire class. All written assignments are due during the first 15 minutes of class on the day they are due. ___ points will be deducted for papers that are turned in _____ late. Requests for Extensions and Incompletes Incompletes and extensions to due dates on specific assignments will only be considered in grave circumstances, such as loss of an immediate family member, hospitalization, or severe illness. Fostering Professionalism As a course in a professional training program, students are expected to consistently demonstrate professional behavior. This includes but is not limited to: Being on time: to class and with assignments Respectful interactions with students and faculty Proactive engagement in learning process and assignments Being organized and prepared Managing paperwork effectively Managing technology effectively (university has extensive computer, printing and internet support; use it in times of technical emergency) Managing personal crises effectively Managing personal information (own and others’) appropriately Students who have trouble in one or more of these areas may have their participation grade lowered and in severe cases may be referred to the department student affairs committee for further review. Students with Disabilities If you have special needs as addressed by the Americans with Disabilities Act (ADA) and need course materials in alternative formats, notify your course instructor within the first two weeks of class. Students interested in accommodations should contact the university’s office for students with disabilities; only this office can recommend and arrange for accommodations. No accommodations may be made without their approval. Any and all reasonable efforts will be made to accommodate your special needs. 4 Policy on Cheating and Plagiarism Cheating and plagiarism are serious offenses in a professional program and may result in expulsion from the program/university on a first offense. See the University Catalog for further information. Additionally, student should refer to the Ethics Codes of AAMFT, ACA, APA, and/or NASW for ethical guidelines regarding plagiarism. For a definition and examples of plagiarism, students can refer to the APA Publication Manual. 5 Tentative Schedule Date Week 1 Week 2 Week 3 Week 4 Week 5 Week 6 Week 7 Week 8 Week 9 Week 10 Week 11 Week 12 Week 13 Week 14 Week 15 Topic Introduction to Practicum/Fieldwork Introduction to Forms; Review contracts with sites; Review ethics How to conceptualize cases How to complete clinical assessment/intake forms Clinical Assessment presentations How to write treatment plans Treatment plans Reading Chp 1-2 Assignments/Forms Due Gehart Chp Paperwork/Contracts for Site 3-4 Due Gehart, Chp 13 Gehart, Chp 14 Gehart, 5-6 Gehart, Chp 15 Gehart, 7-8 How to write progress notes Gehart, Chp. 17 Progress note presentations Gehart, 910 Evaluation of Progress Gehart, Chp. 16 Case conceptualization Gehart, 11presentations 12 Case conceptualization presentations cont. Case conceptualization presentations cont. Working with your supervisor Final Meeting 6 Assessment presentation; bring copies for all Treatment plan presentations: Bring copies for all Progress note presentations; bring copies for all Case conceptualization presentations; bring copies for all Case conceptualization presentations; bring copies for all Case conceptualization presentations; bring copies for all Turn in End of Semester Paperwork: Logs, Evaluations Instructions for Activities Progress Note, Assessment, and Treatment Plan Presentations On the weeks progress note, assessment, and treatment plan presentations are scheduled, you should bring a COMPLETED example of a progress, assessment or treatment plan based on a client you are working with at your fieldsite [or if practicum class, from a video or other source]. Students should complete the forms from the text, available on the Cengage website for this text. DO NOT INCLUDE CONFIDENTIAL INFORMATION. Bring enough copies for the class. Each person will have 5 minutes to discuss his/her example. Case Conceptualization Presentation Towards the end of the semester, each student will give a 20-minute presentation of a client at their site [or other source] using the case conceptualization form with genogram [optional] from the text. Students should complete the forms from the text, available on the Cengage website for this text. DO NOT INCLUDE CONFIDENTIAL INFORMATION. Bring enough copies for the class. 7 Competencies Measured The assignments in this class measure the following AAMFT Marriage and Family Therapy Competencies Competencies measured on the Case Conceptualization 1.1.1 Understand systems concepts, theories, and techniques that are foundational to the practice of marriage and family therapy. 1.1.2 Understand theories and techniques of individual, marital, couple, family, and group psychotherapy 1.2.1 Recognize contextual and systemic dynamics (e.g., gender, age, socioeconomic status, culture/race/ethnicity, sexual orientation, spirituality, religion, larger systems, social context). 1.2.2 Consider health status, mental status, other therapy, and other systems involved in the clients’ lives (e.g., courts, social services). 1.3.1 Gather and review intake information, giving balanced attention to individual, family, community, cultural, and contextual factors. 1.3.7 Solicit and use client feedback throughout the therapeutic process. 1.5.2 Complete case documentation in a timely manner and in accordance with relevant laws and policies. 2.1.1 Understand principles of human development; human sexuality; gender development; psychopathology; psychopharmacology; couple processes; and family development and processes (e.g., family, relational, and system dynamics). 2.1.5 Understand the current models for assessment and diagnosis of mental health disorders, substance use disorders, and relational functioning. 2.2.2 Systematically integrate client reports, observations of client behaviors, client relationship patterns, reports from other professionals, results from testing procedures, and interactions with client to guide the assessment process. 2.2.3 Develop hypotheses regarding relationship patterns, their bearing on the presenting problem, and the influence of extra-therapeutic factors on client systems. 2.2.4 Consider the influence of treatment on extra-therapeutic relationships. 2.2.5 Consider physical/organic problems that can cause or exacerbate emotional/interpersonal symptoms. 2.3.1 Diagnose and assess client behavioral and relational health problems systemically and contextually. 2.3.6 Assess family history and dynamics using a genogram or other assessment instruments. 2.3.7 Elicit a relevant and accurate biopsychosocial history to understand the context of the clients’ problems. 2.3.8 Identify clients’ strengths, resilience, and resources. 2.3.9 Elucidate presenting problem from the perspective of each member of the therapeutic system. 8 2.4.2 Assess ability to view issues and therapeutic processes systemically. 3.2.1 Integrate client feedback, assessment, contextual information, and diagnosis with treatment goals and plan. 3.3.1 Develop, with client input, measurable outcomes, treatment goals, treatment plans, and after-care plans with clients utilizing a systemic perspective. 4.3.3 Reframe problems and recursive interaction patterns. 4.4.1 Evaluate interventions for consistency, congruency with model of therapy and theory of change, cultural and contextual relevance, and goals of the treatment plan. Competencies measured on the Clinical Assessment 1.2.1 Recognize contextual and systemic dynamics (e.g., gender, age, socioeconomic status, culture/race/ethnicity, sexual orientation, spirituality, religion, larger systems, social context). 1.2.2 Consider health status, mental status, other therapy, and other systems involved in the clients’ lives (e.g., courts, social services). 1.2.3 Recognize issues that might suggest referral for specialized evaluation, assessment, or care. 1.3.1 Gather and review intake information, giving balanced attention to individual, family, community, cultural, and contextual factors. 1.3.8 Develop and maintain collaborative working relationships with referral resources, other practitioners involved in the clients’ care, and payers. 2.1.1 Understand principles of human development; human sexuality; gender development; psychopathology; psychopharmacology; couple processes; and family development and processes (e.g., family, relational, and system dynamics). 2.1.2 Understand the major behavioral health disorders, including the epidemiology, etiology, phenomenology, effective treatments, course, and prognosis. 2.1.3 Understand the clinical needs and implications of persons with comorbid disorders (e.g., substance abuse and mental health; heart disease and depression). 2.1.5 Understand the current models for assessment and diagnosis of mental health disorders, substance use disorders, and relational functioning. 2.1.7 Understand the concepts of reliability and validity, their relationship to assessment instruments, and how they influence therapeutic decision making. 2.2.2 Systematically integrate client reports, observations of client behaviors, client relationship patterns, reports from other professionals, results from testing procedures, and interactions with client to guide the assessment process. 2.2.3 Develop hypotheses regarding relationship patterns, their bearing on the presenting problem, and the influence of extra-therapeutic factors on client systems. 2.2.5 Consider physical/organic problems that can cause or exacerbate emotional/interpersonal symptoms. 2.3.1 Diagnose and assess client behavioral and relational health problems systemically and contextually. 2.3.2 Provide assessments and deliver developmentally appropriate services to clients, such 9 as children, adolescents, elders, and persons with special needs. 2.3.4 Administer and interpret results of assessment instruments. 2.3.5 Screen and develop adequate safety plans for substance abuse, child and elder maltreatment, domestic violence, physical violence, suicide potential, and dangerousness to self and others. 2.3.7 Elicit a relevant and accurate biopsychosocial history to understand the context of the clients’ problems. 2.3.9 Elucidate presenting problem from the perspective of each member of the therapeutic system. 2.4.4 Assess the therapist-client agreement of therapeutic goals and diagnosis. 3.1.1 Know which models, modalities, and/or techniques are most effective for presenting problems. 3.1.3 Understand the effects that psychotropic and other medications have on clients and the treatment process. 3.1.4 Understand recovery-oriented behavioral health services (e.g., self-help groups, 12step programs, peer-to-peer services, supported employment). 3.2.1 Integrate client feedback, assessment, contextual information, and diagnosis with treatment goals and plan. 3.3.1 Develop, with client input, measurable outcomes, treatment goals, treatment plans, and after-care plans with clients utilizing a systemic perspective. 3.3.6 Manage risks, crises, and emergencies. 3.3.7 Work collaboratively with other stakeholders, including family members, other significant persons, and professionals not present. 3.3.8 Assist clients in obtaining needed care while navigating complex systems of care. 3.4.3 Evaluate level of risks, management of risks, crises, and emergencies. 4.1.2 Recognize strengths, limitations, and contraindications of specific therapy models, including the risk of harm associated with models that incorporate assumptions of family dysfunction, pathogenesis, or cultural deficit. 4.3.1 Match treatment modalities and techniques to clients’ needs, goals, and values. 4.5.1 Respect multiple perspectives (e.g., clients, team, supervisor, practitioners from other disciplines who are involved in the case). 5.2.1 Recognize situations in which ethics, laws, professional liability, and standards of practice apply. 5.3.4 Develop safety plans for clients who present with potential self-harm, suicide, abuse, or violence. 5.3.5 Take appropriate action when ethical and legal dilemmas emerge. 5.3.6 Report information to appropriate authorities as required by law. 5.4.1 Evaluate activities related to ethics, legal issues, and practice standards. Competencies measured on the Treatment Plan 10 1.1.2 Understand theories and techniques of individual, marital, couple, family, and group psychotherapy. 1.1.4 Understand the risks and benefits of individual, marital, couple, family, and group psychotherapy. 1.2.3 Recognize issues that might suggest referral for specialized evaluation, assessment, or care. 1.3.2 Determine who should attend therapy and in what configuration (e.g., individual, couple, family, extrafamilial resources). 1.3.3 Facilitate therapeutic involvement of all necessary participants in treatment. 1.3.6 Establish and maintain appropriate and productive therapeutic alliances with the clients. 1.3.7 Solicit and use client feedback throughout the therapeutic process. 1.4.1 Evaluate case for appropriateness for treatment within professional scope of practice and competence. 2.1.4 Comprehend individual, marital, couple and family assessment instruments appropriate to presenting problem, practice setting, and cultural context. 2.1.6 Understand the strengths and limitations of the models of assessment and diagnosis, especially as they relate to different cultural, economic, and ethnic groups. 2.3.2 Provide assessments and deliver developmentally appropriate services to clients, such as children, adolescents, elders, and persons with special needs. 2.3.3 Apply effective and systemic interviewing techniques and strategies. 3.1.1 Know which models, modalities, and/or techniques are most effective for presenting problems. 3.2.1 Integrate client feedback, assessment, contextual information, and diagnosis with treatment goals and plan. 3.3.1 Develop, with client input, measurable outcomes, treatment goals, treatment plans, and after-care plans with clients utilizing a systemic perspective. 3.3.2 Prioritize treatment goals. 3.3.3 Develop a clear plan of how sessions will be conducted. 3.3.6 Manage risks, crises, and emergencies. 3.3.9 Develop termination and aftercare plans. 3.5.3 Write plans and complete other case documentation in accordance with practice setting policies, professional standards, and state/provincial laws. 4.1.1 Comprehend a variety of individual and systemic therapeutic models and their application, including evidence-based therapies and culturally sensitive approaches. 4.1.2 Recognize strengths, limitations, and contraindications of specific therapy models, including the risk of harm associated with models that incorporate assumptions of family dysfunction, pathogenesis, or cultural deficit. 4.2.1 Recognize how different techniques may impact the treatment process. 4.2.2 Distinguish differences between content and process issues, their role in therapy, and their potential impact on therapeutic outcomes. 4.3.1 Match treatment modalities and techniques to clients’ needs, goals, and values. 11 4.3.3 Reframe problems and recursive interaction patterns. 4.3.4 Generate relational questions and reflexive comments in the therapy room. 4.3.5 Engage each family member in the treatment process as appropriate. 4.3.6 Facilitate clients developing and integrating solutions to problems. 4.3.8 Empower clients and their relational systems to establish effective relationships with each other and larger systems. 4.3.9 Provide psychoeducation to families whose members have serious mental illness or other disorders. 4.4.1 Evaluate interventions for consistency, congruency with model of therapy and theory of change, cultural and contextual relevance, and goals of the treatment plan. 4.4.5 Evaluate clients’ outcomes for the need to continue, refer, or terminate therapy. 4.5.3 Articulate rationales for interventions related to treatment goals and plan, assessment information, and systemic understanding of clients’ context and dynamics. 5.3.4 Develop safety plans for clients who present with potential self-harm, suicide, abuse, or violence. 6.1.1 Know the extant MFT literature, research, and evidence-based practice. 6.3.2 Use current MFT and other research to inform clinical practice. Competencies measured on the Progress Note 1.2.1 Recognize contextual and systemic dynamics (e.g., gender, age, socioeconomic status, culture/race/ethnicity, sexual orientation, spirituality, religion, larger systems, social context). 1.3.5 Obtain consent to treatment from all responsible persons. 1.3.8 Develop and maintain collaborative working relationships with referral resources, other practitioners involved in the clients’ care, and payers. 1.5.2 Complete case documentation in a timely manner and in accordance with relevant laws and policies. 1.5.3 Develop, establish, and maintain policies for fees, payment, record keeping, and confidentiality. 2.3.1 Diagnose and assess client behavioral and relational health problems systemically and contextually. 2.3.5 Screen and develop adequate safety plans for substance abuse, child and elder maltreatment, domestic violence, physical violence, suicide potential, and dangerousness to self and others. 2.4.4 Assess the therapist-client agreement of therapeutic goals and diagnosis. 2.5.1 Utilize consultation and supervision effectively. 3.1.2 Understand the liabilities incurred when billing third parties, the codes necessary for reimbursement, and how to use them correctly. 3.2.1 Integrate client feedback, assessment, contextual information, and diagnosis with treatment goals and plan. 12 3.3.1 Develop, with client input, measurable outcomes, treatment goals, treatment plans, and after-care plans with clients utilizing a systemic perspective. 3.3.3 Develop a clear plan of how sessions will be conducted. 3.3.6 Manage risks, crises, and emergencies. 3.3.7 Work collaboratively with other stakeholders, including family members, other significant persons, and professionals not present. 3.4.1 Evaluate progress of sessions toward treatment goals. 3.5.3 Write plans and complete other case documentation in accordance with practice setting policies, professional standards, and state/provincial laws. 4.3.1 Match treatment modalities and techniques to clients’ needs, goals, and values. 4.4.4 Evaluate clients’ reactions or responses to interventions. 4.4.6 Evaluate reactions to the treatment process (e.g., transference, family of origin, current stress level, current life situation, cultural context) and their impact on effective intervention and clinical outcomes. 4.5.1 Respect multiple perspectives (e.g., clients, team, supervisor, practitioners from other disciplines who are involved in the case). 4.5.3 Articulate rationales for interventions related to treatment goals and plan, assessment information, and systemic understanding of clients’ context and dynamics. 5.2.2 Recognize ethical dilemmas in practice setting. 5.2.3 Recognize when a legal consultation is necessary. 5.2.4 Recognize when clinical supervision or consultation is necessary. 5.3.4 Develop safety plans for clients who present with potential self-harm, suicide, abuse, or violence. 5.3.5 Take appropriate action when ethical and legal dilemmas emerge. 5.5.1 Maintain client records with timely and accurate notes. 5.5.3 Pursue professional development through self-supervision, collegial consultation, professional reading, and continuing educational activities. 13