THE EYE
advertisement

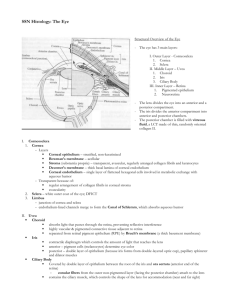
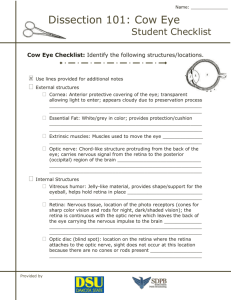
THE EYE Judianne Kellaway, MD, MEd Learning Objectives: Label anatomical components of the eye Know how components regulate light into the eye Know how components regulate focus Know layers and functions of cornea, iris, ciliary body, and retina Key Words: Cornea, limbus, iris, ciliary body, choroids, retina, pigmented retinal epithelium, lens, accommodation and eyelids INTRODUCTION The eye is a complex photosensitive organ, which conveys the form, light intensity, and color of an environmental image to a photoreceptive layer, the retina, which transmits a corresponding electrical image to the brain. MAJOR ANATOMIC COMPARTMENTS OF THE EYE Anterior segment -Anterior chamber -Posterior chamber Posterior segment -Vitreous body [N.B. Terminology: Outer refers to structures nearer the surface of the eyeball, while inner refers to a structure nearer the midpoint of the globe.] Tunics Fibrous tunic (tunica fibrosa)-outermost layer Cornea Transparent, very tough, can withstand force of 5 kg/cm2 ~12mm in diameter Thickness ranges between 0.8-0.9mm centrally to 1.1mm peripherally Refractive power twice as high as lens Five layers Epithelium ~10% of corneal thickness (~50µm) avascular stratified squamous epithelium, nonkeratinizing 5-7 cell layers thick very smooth, bathed in lacrimal fluid Bowman’s layer 8-14 µm thick Condensation of anterior stroma Mostly collagen fibers, randomly disposed Stroma or substantia propria 90% of corneal thickness (~500 µm) collagen fibrils arranged in lamellae 200-250 lamellae in regular layers collagen turnover slow, ~12 months Descemet’s membrane basement membrane of corneal endothelium ~10 µm thick increasing thickness with age Endothelium monolayer of squamous epithelium facing the anterior chamber Critical pump function. Na, K ATPase to dehydrate cornea Sclera Posterior five-sixths of globe Thickness ranging from 0.3mm at equator to 1mm posteriorly Lamina cribosa posteriorly at site of optic nerve exit Primarily collagen in highly complex orientation Terminates at limbus At optic nerve, outer ½ of sclera is continuous with the dural sheath Limbus Narrow (~1 ½ mm) zone between sclera and cornea Provides nourishment for peripheral cornea and removes aqueous humor Aqueous humor passes through trabecular meshwork into Schlemm’s canal, then into episcleral veins Mean intraocular pressure ~20mm Hg Episcleral venous pressure ~10mm Hg Limbus Components Conjunctiva (has two components) Epithelium Stroma Ciliary muscle Schlemm’s canal Internal trabecular meshwork (spaces of Fontana) Uveal meshwork Iris Anterior chamber Posterior chamber Vascular tunic (tunica vasculosa or uvea) – middle layer Iris Circular diaphragm anterior to lens Central aperture = pupil Peripheral border = ciliary border Central border = papillary border Separates anterior segment into anterior and posterior chambers Stroma consists of loose, pigmented, highly vascularized connective tissue with pigment epithelium lining posterior surface. Eye color determined by relative member of melanocytes in stroma. Sphincter muscle (parasympathetic fibers of the oculomotor nerve); contraction causes decreased papillary aperture Dilator muscle (sympathetic postganglionic fibers from superior cervical ganglion); contraction causes increased papillary aperture Pupil changes from 1.5 8mm diameter Components of the Iris/Cornea Angle Cornea Anterior chamber Posterior chamber Stroma Pupillary sphincter muscle Pupillary dilator muscle Pigmented epithelium Trabecular meshwork Canal of Schlemm Ciliary Body Ring like structure anterior to ora serrata (border where retina begins). Contains large smooth muscle group… Ciliary muscle, which regulates tension on lens for accommodation for near vision (parasympathetic innervation). Composed of radial muscles, meridional muscles (Brucke’s muscle) and circular muscles (Muller’s muscle) Lined by double layer of epithelial cells Non-pigmented epithelium: Inner layer continuous with neural retina; Produces aqueous humor Pigmented epithelium: Outer layer continuous with retinal pigmented epithelium Ciliary processes are radially arranged ridges from which the zonular fibers extend to insert on the lens capsule. Choroid Thin pigmented region adjacent to inner surface of sclera Composed of three layers 1. Vessel layer (stratum vasculosum): Outermost layer, contains large vessels and melanocytes 2. Choriocapillary layer (lamina choriocapillaries): Middle layer with small vessels to supply outer retina 3. Bruch’s membrane (lamina vitrea): Inner layer, actually basement membrane of the retinal pigmented epithelium Retina Retinal pigmented epithelium (RPE) Outer layer of retina (next to choroid) Simple columnar epithelium containing abundant melanin granules Apical processes interdigitate with outer segments of photoreceptor cells Functions: synthesis of Vitamin A, phagocytosis of shed outer rod and cone segments; metabolic and physical support for outer segments; absorbs light after photoreceptors stimulated. Neural retina Photoreceptors. Inner and outer segments of cone and rod cells. Rods (visual pigment rhodopsin) most numerous (120 million). Cones (visual pigment iodopsin) 6 million. Cones concentrated in fovea for highest visual acuity. Cones’ outer segment disks are folds of plasma membrane. Rod disks are separate stacks. Rods are sensitive to light for low illumination vision. Cones are responsible for color vision. Outer limiting membrane. Junctional complexes between Muller cells and photoreceptor cells. Outer nuclear layer. Nuclei of photoreceptors. Outer plexiform layer. Synapses of photoreceptor axons and dendrites of bipolar cells and horizontal cells. Inner nuclear layer. Nuclei of bipolar, amacrine, horizontal and Muller cells. Inner plexiform layer. Synapses between bipolar, ganglion and amacrine cells. Ganglion cell layer. Ganglion cells of the neural retina. Nerve fiber layer. Axons of ganglion cells Inner limiting membrane. Basal lamina of the connected Muller cells. Lens Biconvex transparent structure suspended by zonular fibers. Posterior side is “more convex” than anterior. Capsule is 10-20 µm thick, made of transparent type IV collagen. Surround entire lens for zonular attachment. Basement membrane = capsule Lens epithelium is made up of large cuboidal cells one thick. Found only on the anterior aspect of the lens. Lens proper is made up of tightly packed cells containing crystalline. Highly elastic with an inherent tendency to return to a more globular shape. New lens cells are added from the periphery: those in the center of the lens are the oldest and have lost their nuclei. Other Anatomic Considerations Adult globe is about 24mm in diameter. The optic disc does not contain rods or cones and thus represents the blind spot. It lies about 4 mm from the nasal to the macula The macula contains the fovea, the region that allows the greatest visual acuity; only cone photoreceptors are present in the fovea. Blood-retina barrier is composed of tight junctions between the RPE cells (outer barrier) as well as impermeable retina vessels (inner barrier). Blood supply: Outer retinal layers receive blood supply from choriocapillaries (via diffusion) while inner retinal layers are supplied by the central retinal artery, which enters the eye with optic nerve. The vitreous body, which fills the vitreous cavity, is a transparent, colorless, structureless, gelatinous mass composed of hyaluronic acid, collagen, and water. Lids Skin- very thin: contains numerous small hairs, sebaceous and sweat glands. Eyelashes-arranged in 3-4 rows along lid edge. Follicles associated with sebaceous glands. Glands of Moll – specialized sweat glands Orbicularis oculi – striated muscle fibers Tarsal plate – dense connective tissue, which impart support and structure to the lid; contain numerous specialized sebaceous glands called the Meibomian glands. Conjunctiva- innermost layer of the lid, stratified columnar epithelium containing numerous goblet cells. Tarsal conjunctiva lines the inner aspect of the lid Bulbar conjunctiva lines the external surface of the globe Tears Most of the liquid in tears comes from the lacrimal glands, one per eye, in the upper lateral region of the orbit. The aqueous secretion contains, in addition to serum components and ions: Lactoferrin - bacteriostatic agent, which binds iron for bacterial metabolism. Lysozyme - bacteriolytic agent Secretory IgA Tear specific albumin – unknown function A “cross-section” of the tear on the surface scleral epithelium reveals three layers: Outer layer of phospholipid from the meibomian glands. Prevents evaporation of underlying fluid. Middle layer is the largest amount of saline/serum fluid from the lacrimal glands. Inner layer is comprised of mucin like substance from the conjunctival goblet cells. This spreads out on the microplicae of the external epithelium to help break surface tension and allow aqueous portion to spread over the eye. Accommodation The mechanism by which the eye changes focus from distant to near images is called accommodation. Accommodation is produced by a change in lens shape as a result of the action of the ciliary muscle on the zonular fibers. The lens substance is most malleable during childhood and the young adult years, and it progressively loses its ability to change shape with age. After approximately 40 years, the rigidity of the lens nucleus clinically reduces accommodation. Most of the change in lens shape that takes place during accommodation occurs at the central anterior lens surface. The central anterior capsule is thinner than the peripheral capsule, and the anterior zonular fibers insert slightly closer to the visual axis than do the posterior zonular fibers, resulting in a central anterior bulge with accommodation. The central posterior capsule is the thinnest area of the capsule and tends to bulge posteriorly to the same extent regardless of zonular tension. The ciliary muscle is a ring that, upon contraction, has the opposite effect from that intuitively expected of a sphincter. When a sphincter muscle contracts, it usually tightens its grip. However, when the ciliary muscle contracts, the diameter of the muscle ring is reduced, thereby relaxing the tension on the zonular fibers and allowing the lens to become more spherical. Thus, when the ciliary muscle contracts, the axial thickness of the lens increases its diameter decreases and its dioptric power increases, producing accommodation. When the ciliary muscle relaxes, the zonular tension increases, the lens flattens, and its dioptric power decreases. Changes with Accommodation With Accommodation Ciliary muscle action Contraction Zonular tension Decreases Lens Shape More Spherical Without Accommodation Relaxation Increases Flatter The accommodative response may be stimulated by the known or apparent size and distance of an object, or by blur, chromatic aberration, or a continual oscillation of ciliary tone. Accommodation is mediated by the parasympathetic fibers of cranial nerve III (oculomotor). Parasympathomimetic drugs (e.g. pilocarpine) induce accommodation, while parasympatholytic medications (e.g. atropine) block accommodation. Drugs that cause relaxation of the ciliary muscle are called cycloplegics. The amplitude of accommodation is the amount of change in the eye’s refractive power that is produced by accommodation. It diminishes with age and may be affected by some medications and diseases. Adolescents generally have 12-16 diopters of accommodation, while adults at age 40 have 4-8 diopters. After age 50 accommodation decreases to less than 2 diopters. Hardening of the lens with age is the principal cause of accommodation, which is called presbyopia. OPHTHALMIC SYSTEM LABORATORY Introduction The eye is a high specialized, photosensitive organ which is housed in a bony orbit and glides in a bed of orbital fat. Associated skeletal muscles aid in controlling eye movements. The eye is able to focus on near objects (accommodation) and far images as well. Each of you has one slide of the eye. Some of these slides demonstrate a section of the retina only; some slides are hemisections of the eye showing all major structures. If you have a slide which shows retina only, please borrow the more complete slide from a neighbor. You will also have access to excellent commercial slides. These must be returned at the end of the session but can be checked out from HEO. Slide 62 Human eye: Locate the following structures: 1. Locate the cornea. Note that the external, convex surface is covered by about 5 layers of stratified epithelium and the inner, concave surface is covered by a simple squamous epithelium, the endothelium. Identify Bowman’s membrane underlying the stratified epithelium and Descemet’s membrane underlying the endothelium. Locate the relatively acellular stroma. 2. Identify the iris. It looks like a leaf cut in cross section. Note that the external portion contains scattered melanocytes (pigmented cells) and smooth muscle cells which form the papillary sphincter muscle. The inner surface contains two layers of epithelial cells; the innermost one is fully pigmented, the outer most is a layer of partly pigmented smooth muscle and the remainder of the cell contains melanin granules. The Myoepithelial cells form the papillary dilator muscle. 3. Locate the lens. This transparent, refractive structure is suspended by zonular fibers arising from the ciliary processed. Note that it stains very acidophilic because of its high protein content. The lens is encased in a thick basement membrane which serves as a capsule and is composed of an anterior layer of subcapsular epithelium and densely packed, anucleate lens fibers (cells). Lens changes shape as tension is increased or decreased on zonule. Lens often appears disrupted in histologic section because low water content makes sectioning difficult. 4. Locate the zonular fibers. Collectively these form the zonule. In histologic section, the fibers are wispy and pink; they extend from the ciliary processes and insert into the lens capsule. 5. Ciliary body. The ciliary body encircles the inner aspect of the eyeball like a belt. In histologic section it is a triangular shaped are with small finger-like extensions radiating toward the lens. The zonular fibers arise from the ciliary processes. Identify the ciliary processes. Note that they are covered by two layers of simple, cuboidal epithelium. The innermost layer is non-pigmented, but the outermost layer contains abundant melanin. Note the pink-staining smooth muscle cells in the ciliary body. These form the ciliary muscle that contracts to EASE tension on the zonule and allow the lens to thicken. 6. Locate the three cavities of the eye. The anterior chamber is formed by posterior surface of cornea and the anterior surfaces of the iris and lens. The posterior chamber is small and is formed by posterior surface of iris, anterior surface of lens and ciliary processes. These two chambers contain aqueous humor. The vitreous chamber is the large space posterior to the lens that contains the vitreous body. It appears as a space in histologic section. 7. Identify the sclera. This outer tunic of the eyeball is composed of compact, fibrous connective tissue and stains acidophilic due to high type I collagen content. It begins interiorly at the limbos, its side of junction with the cornea. The canal of Schlemm is located in this region. The sclera extends posteriorly to the region of the blind spot (optic disc or papilla) where the optic nerve exits the eyeball. 8. Find the choroid coat. The tissue layer lies just internal to the sclera. It contains numerous vessels and melanocytes. Identify the pigment-containing cells and the blood vessels. The choroid vessels provide nutrients to the retina. 9. Find the retina. The outer layer of the retina is the pigment epithelium, a simple columnar (cuboidal) epithelium which is the highly pigmented and lies sandwiches between the choroid and the rod and con layer of the retina. Find the pigment epithelium. Locate the neural retina, the photosensitive layer of the retina. The neural retina lies between the vitreous cavity and the pigment epithelium. Please identify 6 of the neural retina layers: 1) the rods and cones. The acidophilic rod and cone outer segments lie adjacent to the pigment epithelium. Their basophilic nuclei are just internal to the outer segment layer. 2) Outer (external) plexiform layer. This thick layer is site of synapse of rod and cones with bipolar cells. It stains slightly acidophilic. 3) Bipolar cell layer. This layer can be identified by locating the middle layer of nuclei. 4) Inner (internal) plexiform layer. Again, a lightly acidophilic layer just internal to the layer of bipolar ganglion cells. 5) Ganglion cell layer. Identify this layer by locating the innermost layer of basophilic nuclei. 6) Inner limiting membrane. Pale acidophilic, innermost layer of neural retina. 10. Find the optic nerve. Note that it exits through the lamina cribrosa at the blind spot near the posterior pole of the eyeball. Also notice that all layers of the retina disappear at the blind spot except the inner limiting membrane. Fold your lower eyelid down and have your lab friends look for yellowish stripes on the inside. If you look carefully you’ll see that these stripes end in small pores at the root of your eyelashes. These are the Meibomian glands and their ducts empty onto the cornea to help make part of the tear. There should be a slide of the human eyelid on the demo microscope. You should check this for the large Meibomian glands as well as the obicularis muscle. In part of the conjunctiva (inside the eyelid) way up from the eyelash, try to find the goblet cells. The secretions of the Meibomian glands and goblet cells help break the surface tension of the lacrimal fluid (you can’t see the lacrimal gland in this slide) as well as provide an “outer coat” for the tear to inhibit evaporation.