22 General lethargy and tiredness
advertisement

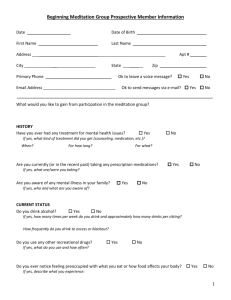
22 General lethargy and tiredness Checklist Appropriate introduction Confirms patient’s name and age Explains reason for consultation Obtains consent Open question to elicit presenting complaint Allows patient to open up, listens carefully, remains silent and does not interrupt the patient Signposts: e.g. ‘Mr Gregory, thank you for telling me about this problem. I would like to ask a few more detailed questions. Is that all right?’ History of presenting complaint: • • • • • • • • • • • • Onset (how it started) Character (what the patient means by tiredness) Time (duration) Alleviating factors Exacerbating factors Severity (in comparison with other episodes of tiredness) Asks if there is a pattern with activities/daily routine Asks about menstrual disturbances (if patient female) Establishes sleep pattern Asks if patient is suffering from any other symptoms Asks about any recent illnesses Previous episodes of lethargy/tiredness Depression screening: asks about mood, previous history of depression and sleeping patterns Asks closed focused questions to rule out specific common causes of lethargy: • Thyroid dysfunction (sweating, tremor, dry hair, neck discomfort, eye symptoms, bowel changes, menstrual irregularities) • Anaemia (shortness of breath, chest pain, palpitations, menorrhagia) • Diabetes mellitus (polydipsia, polyuria, recurrent infection) • Cancer (weight loss, night sweats, family history of cancers, cough, diarrhoea, melaena) • Hypopituitarism (loss of appetite, nipple discharge, loss of libido) • Chronic kidney disease/nephrotic syndrome (ankle swelling, orthopnoea) • Chronic infection (fevers) • Chronic fatigue syndrome symptoms (sore throat, headaches, muscle pains, exacerbated by exertion) • Obstructive sleep apnoea (unrefreshing sleep, feeling sleepy in the day, loud snoring, waking up suddenly in the night, loss P MP F Checklist of libido, irritability) • Depression (mood, anhedonia, sleep, appetite, concentration) Review of systems ‘Red flags’: • Night sweats • Fevers • Weight loss • Loss of appetite • Palpable lymph nodes Past medical history Family history: • Cancers • Endocrine disorders, especially thyroid disorders and diabetes • Depression Drug history: • Over-the-counter medication Allergies Social history: • Smoking • Alcohol • Illicit drug use • Stressors in social life (relationship, financial, etc.) • Change in work/occupation • Symptoms of depression or anxiety • Recent foreign travel Use of non-verbal cues, e.g. good eye contact, nodding head and good body posture Systematic approach Explores and responds to ICE: • Ideas • Concerns • Expectations Shows empathy Non-verbal skills Avoids technical jargon Devises holistic management plan and addresses psychosocial issues as well as medical problems Summarises Offers to answer any questions Thanks patient P MP F OSCEs for Medical Finals, First Edition. Hamed Khan, Iqbal Khan, Akhil Gupta, Nazmul Hussain, and Sathiji Nageshwaran. © 2013 John Wiley & Sons, Ltd. Published 2013 by John Wiley & Sons, Ltd.