26.Surgical diseases of the thyroid gland
advertisement

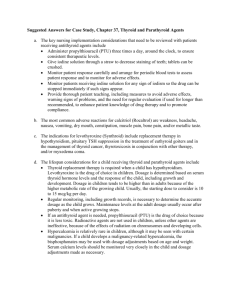
THE KURSK STATE MEDICAL UNIVERSITY DEPARTMENT OF SURGICAL DISEASES № 1 SURGICAL DISEASES OF THE THYROID GLAND Information for self-training of English-speaking students The chair of surgical diseases N 1 (Chair-head - prof. S.V.Ivanov) BY ASS. PROFESSOR M.V. YAKOVLEVA KURSK-2010 1 I. INTRODUCTION The name thyroid is derived from the Greek description of a shield-shaped gland in the anterior neck ("thyreoides"). Classical anatomic descriptions of the thyroid were available in the 16th and 17th centuries, but the function of the gland was not well understood. By the 19th century, pathologic enlargement of the thyroid, or goiter, was described. Medical treatment of this condition was described, using what was most likely iodine-rich seaweed. However, direct surgical approach of thyroid masses had frighteningly high complication and mortality rates. In the late 19th century, two surgeon-physiologists revolutionized treatment of thyroid diseases. Theodor Billroth and Emil Theodor Kocher established large clinics in Europe and, through development of skilled surgical techniques combined with newer anesthetic and antiseptic principles, provided surgical results that proved the safety and efficacy of thyroid surgery for benign and malignant problems. As a result of his pioneering developments in the understanding of thyroid physiology, Kocher received the Nobel Prize in 1909. The 20th century started with the contributions of Kocher and Billroth. In rapid succession, the understanding of altered physiology, including hypothyroidism and hyperthyroidism, thyroid cancer, advances in imaging, epidemiology, and most recently, minimally invasive diagnostic and surgical techniques have taken place. These advances have allowed the diagnosis and treatment of thyroid diseases to become rapid, costeffective, low-morbidity procedures. GENERAL AIM OF THE LESSON General aim of the lesson includes: Acquiring knowledge about etiology and symptomatology of different thyroids’ diseases. Acquiring the practical skills of the patients’ objective examination. Mastering the instrumental examinations main principles. Determining the indications for conservative and surgical treatment of different thyroids’ diseases. TASKS FOR SELF-TRAINING. 2 After individual studying of the material every student must: A/know Etiology of different thyroids’ diseases. Physiology of the thyroid gland. Instrumental methods of thyroid examination, such as: ultrasonography, fine-needle aspiration, computer tomography, radionuclide scan, thyroid functional tests. Advantages and disadvantages of the surgical treatment of different thyroids’ diseases. B/be able to find out main complains and estimate the present state of the patient; to assess the obtained results of the instrumental diagnostical methods; to determine indications and contraindications for different kinds of surgical resection to define indications for conservative (radionuclide therapy, antithyroid medication or replacement therapy) treatment. INITIAL LEVEL OF KNOWLEDGE: Anatomo-physiological and histological data about the thyroid gland and it’s diseases. IV. BRIEF OUTLINE OF THE TOPIC (OBLIGATORY MATERIAL FOR ACQUISITION). DISORDERS OF THYROID METABOLISM. BENIGN THYROID DISEASE. 1. Hypothyroidism A delicate balance between central production and peripheral action of T 3 and T 4 is required for a euthyroid state in the periphery. Clinical hypothyroidism is usually associated with decreased production in the thyroid gland, although states of limited activity in the periphery can also occur. In many underdeveloped countries, lack of sufficient iodine intake explains a large percentage of hypothyroid conditions. In more developed countries, most cases of adult hypothyroidism are caused by Hashimoto's thyroiditis, overaggressive radioactive iodine therapy, or surgical ablation. Other causes of hypothyroidism are becoming increasingly relevant, including drug-related altered thyroid function, particularly in the case of the cardiac antiarrhythmic drug amiodarone. Other rarer causes of hypothyroidism include inherited defects in thyroid hormone 3 synthesis, which include defects in thyroid peroxidase and thyroglobulin production. Additionally, congenital aberrant thyroid development can occur in children, which includes thyroid agenesis or thyroid hypoplasia. Central nervous system abnormalities resulting in either anterior pituitary gland disease or hypothalamic disorders can result in a centrally based hypothyroidism resulting from the lack of either TSH or TRH secretion. Finally, a peripheral tissue resistance to thyroid hormone action, possibly through an altered receptor mechanism, has been described. Endemic Goiter Iodine deficiency can result in a completely preventable disease referred to as endemic goiter, which in its severest form results in endemic cretinism. It may be that as many as one third of the world's population, specifically in underdeveloped countries, are at risk for iodine deficiency, and about 12 million people may suffer from endemic cretinism. Although countries in Southeast Asia, including India, Indonesia, and China, account for most of the total population of the world at risk for iodine deficiency, mild to moderate iodine deficiency can still be seen in a number of European countries, including Italy, Spain, Hungary, Poland, and Yugoslavia. In areas with the most severe iodine deficiency, clinical signs and symptoms of goiter appear at an earlier age. The prevalence increases dramatically in the later childhood years, attaining a peak at puberty. The appearance of goiter decreases during adulthood, remaining slightly greater in women. Metabolic Consequences of Iodine Deficiency The chronic physiologic changes that result from a lifetime of iodine deficiency involve anatomic and metabolic alterations of varying significance. As a result of chronic deficient iodine intake, decreased T 4 and T 3 production occurs. This results in gradually increasing thyroid clearance of iodine and decreased renal excretion. Chronic preferential production of T 3 rather than T 4 occurs as well as enhanced peripheral conversion of T 4 to T 3. By making production of T 3 and clearance of the metabolically active hormone as efficient as possible, clinical hypothyroidism is largely avoided by a biochemical pattern of low serum T 4 with elevated TSH and normal or above-normal levels of T3. In the severest cases, serum T 3 and T 4 concentrations are low, and serum TSH elevations occur. In these situations, endemic cretinism is often found. Accompanying the physiologic changes in response to iodine deficiency, a diffuse enlargement in the thyroid 4 gland often occurs. The thyroid follicles demonstrate a hypertrophic response with reduction in follicular spaces. As the iodine deficiency becomes more severe, follicles can become inactive and then become distended with colloid. Focal areas of nodular hyperplasia may develop and form nodules, some of which may become hot nodules and have autonomous function. Others become inactive and inert. Necrosis, scarring, and intranodal hemorrhage can occur, resulting in a fibrous ingrowth; all these disorders include marked enlargement of the gland, often in an asymmetrical pattern. Hashimoto's Thyroiditis One of the major causes of hypothyroidism in the adult population is Hashimoto's thyroiditis. A complex immunologic phenomenon results in the formation of immune complex and complement in the basement membrane of the follicular cells. Complement fixation results in thyroid cell function alterations, which impair T 3 and T 4 production. A cascade of cytokine production can result in elaboration of products that directly interfere with thyroid function or in exacerbation of immune response, which ultimately has the same effect. These cellular reactions ultimately result in an infiltration of lymphocytes and a resultant fibrosis, which decreases the number and efficiency of individual follicles. [30] As this immune phenomenon continues, the presence of TSHblocking antibodies can be detected. Thyroid microsomal antibodies are produced that are most likely key mediators in the initial complement-fixation process. As the immune process continues, changes in thyroid function can be altered by levels of these antibodies. Ultimately, a hypothyroid clinical state can occur in patients with persistent TSH-blocking antibodies. Postirradiation Therapy Hypothyroidism Planned clinical hypothyroidism can be the result of treatment of certain disorders with 131 I. This treatment has become increasingly popular for patients with hyperthyroid conditions, including Graves' disease. Between 50 and 70% of patients who receive greater than 10 mCi can be predicted to become clinically hypothyroid. For patients undergoing this type of treatment, continued thyroid monitoring is necessary on an annual basis. 5 External-beam irradiation of patients with lymphomatous disease of the mediastinum or head and neck cancers is associated with subclinical hypothyroidism. This becomes particularly important in patients who have had previous thyroid resection for either benign or malignant disease processes. Postsurgical Hypothyroidism In the event that 131 I therapy is not available for patients with hyperthyroidism or Graves' disease, surgical ablation is an effective way to induce permanent hypothyroidism. Subtotal or total thyroidectomy effectively produces postoperative hypothyroidism. The incidence of postoperative permanent hypothyroidism varies with the skill of the operating surgeon and the amount of thyroid that is truly ablated. The rate of complications, however, such as recurrent laryngeal nerve damage and hypocalcaemia, is increased with more aggressive surgical ablation. Other factors affecting postoperative occurrence of hypothyroidism include antithyroid drug administration, dietary iodine availability, and lymphocytic infiltration of the remaining tissue. Pharmacologic Hypothyroidism AMIODARONE Amiodarone is an antiarrhythmic drug that has particular efficacy in treating ventricular arrhythmias. This drug contains a significant amount of iodine, of which a standard dosage can aggravate thyroid dysfunction. Prolonged administration can result in thyroiditis and resultant hyperthyroidism followed by transient hypothyroidism. This thyroiditis is often associated with an increase in serum interleukin-6 levels, suggesting a cytokine inflammatory response. Severe thyroid dysfunction can occur in patients taking amiodarone, especially those with previously documented Hashimoto's thyroiditis. ANTITHYROID DRUGS Common antithyroid drugs (carbimazole, methimazole, and PTU) can, if given in sufficient quantity, result in hypothyroidism. Careful monitoring of patients taking these drugs and understanding the disease process for which they are given are mandatory in following these patients. Peripheral Tissue Hormone Resistance A rare familial disorder resulting in generalized thyroid hormone resistance may be caused by thyroid receptor (TR) abnormalities. Malfunction of the TR results in clinically 6 apparent hypothyroidism in the setting of elevated serum thyroid hormone levels. Two separate TRs, TR-alpha and TR-beta, are coded by separate genes on chromosomes 17 and 3, respectively, in the human genome. Mutations in TR-beta appear to be responsible for a rare familial disorder of thyroid hormone resistance. TR-alpha appears to be unaffected and uninvolved with such mutations. 2. Hyperthyroidism The disease processes associated with increased thyroid secretion result in a predictable hypermetabolic state. Increased thyroid secretion can be caused by primary alterations within the gland (Graves' disease, toxic nodular goiter, toxic thyroid adenoma) or central nervous system disorders and increased TSH-produced stimulation of the thyroid. Most hyperthyroid states occur because of primary malfunction. Graves' Disease Most hyperthyroid states are caused by Graves' disease (diffuse toxic goiter). Most patients are women between the ages of 20 and 40 years. Around 1960, the pathogenesis of Graves' disease was thought to be due to the long-acting thyroid-stimulating antibody, which resulted in exaggerated thyroid hormone secretion. More recently, it has been demonstrated that a wide variety of antibodies result in a thyroid-stimulating process that incorporates the TSH receptor on follicular cells. Thyroid-stimulating immunoglobulins may stimulate TSH receptors at the same time that certain other immunoglobulins may block TSH binding in the same family of receptors. PATHOLOGY Patients with Graves' disease have an enlarged nodular gland with increased vascularity. The size may be diffuse or asymmetrical, resulting in significant enlargement that is grossly visible and that can result in cosmetic deformity and significant tracheal deviation or compression. On microscopic examination, the follicles are small, with hyperplastic columnar epithelium. Increased lymphoid tissue deposition is also demonstrable in many patients with Graves' disease. CLINICAL PRESENTATION The patient with classic Graves' disease usually has a visibly enlarged neck mass consistent with a goiter. Accompanying clinical thyrotoxicosis and exophthalmoses 7 complete the classic triad of the disease. Hair loss, gynecomastia, and splenomegaly can accompany the clinical presentation. Physical examination is remarkable for an enlarged palpable thyroid with bilateral and central enlargement. Tracheal compression can result in airway-obstructive symptoms. The ocular consequences of prolonged and untreated thyrotoxicosis can be severe. Exophthalmos is thought to be due to the stimulation of fatty fibrous tissue behind the orbit causing outward pressure. Proptosis and supraorbital and infraorbital swelling can result. Conjunctival swelling with accompanying congestion and edema are advanced signs of exophthalmos. In its most severe form, spasm of the upper eyelid resulting in retraction and visualization of a larger amount of sclera than normal can lead to a lid lag and exacerbation of the already swollen conjunctiva. All of these pressure-related phenomena can progress to decreased oculomuscular movements, ophthalmoplegia, and diplopia. Optic nerve damage and blindness can be a long-term result if the underlying condition is not corrected. Clinical presentation of hyperthyroidism also includes the protean manifestations of an increased hypermetabolic state. The classic presentation of patients with long-term thyrotoxicosis includes sweating, weight loss, heat intolerance, and thirst. An altered menstrual cycle can be disturbed to the point of amenorrhea. Cardiovascular stress can be demonstrated by high-output cardiac failure and congestive heart failure with peripheral edema. Arrhythmias include ventricular tachycardia or atrial fibrillation. Gastrointestinal signs may include increased bowel frequency to the point of diarrhea and electrolyte wasting. Psychiatric signs may include altered sleep patterns, emotional mood swings, fatigue, excitability, and agitation. DIAGNOSIS Elevated levels of T 3 and T 4, a decreased or undetectable level of TSH are demonstrated. Thyroid antibodies are usually detected in elevated quantities. A 123 I radionuclide scan should demonstrate diffuse uptake throughout an enlarged gland. An ultrasound or computed tomography scan of the neck may be used to evaluate clinical landmarks. TREATMENT 8 There have been three classic methods to treat Graves' disease: radioiodine ablation, surgery, and antithyroid medication. Radionuclide Therapy. The ideal application of radioactive iodine therapy would be for those patients with small to moderate enlargement of the gland and those in whom antithyroid drugs have clearly not worked. Additional candidates would include patients who desire not to have surgery or for whom surgery is contraindicated. Another group includes those who have recurrence after surgical or medical therapy. The advantages of 131 I therapy include avoidance of surgery and the associated risks for recurrent laryngeal nerve damage, hypothyroidism, or postsurgical recurrence. Disadvantages include a 10% initial incidence, with an increasing long-term incidence of hypothyroidism requiring thyroid replacement therapy and a higher relapse rate after primary treatment requiring further 131 I dosage. Additional disadvantages include exacerbation of cardiac arrhythmias, particularly in elderly patients, possible fetal damage in pregnant women, worsening ophthalmic problems, and rare but possibly lifethreatening thyroid storm. Antithyroid Medication. The main antithyroid action of the drugs PTU, methimazole, and carbimazole is through the inhibition of the organification of intrathyroid iodine as well as inhibition of the coupling of iodotyrosine molecules to form T 3 and T 4. It may be that PTU has the additive effect of blocking peripheral conversion of T 4 to T 3. Peripheral excess of T 3 and T 4 has multiple hyperdynamic and hypermetabolic effects. Drugs that block the peripheral conversion of T 4 to T 3 can effectively modulate peripheral effects of thyrotoxicosis. Additionally, peripheral adrenergic effects of thyrotoxicosis can be modulated by the use of beta-blocking agents such as propranolol. In the acute circumstance, steroids and beta-blockers combine both effects to gain rapid control of the hypermetabolic effects of increased peripheral T 4 and T 3 . Treatment of patients with severe thyrotoxicosis initially starts with beta-blockers such as propranolol. This is specifically effective in treating tachycardia. Propylthiouracil, carbimazole, or methimazole may then be added. If, after several weeks, clinical or chemical hypothyroidism has occurred, thyroid replacement should be carefully given. 9 Antithyroid medication is effective in gaining rapid control of thyrotoxicosis; however, the relapse rate after discontinuation of medication may approach 50% 12 to 18 months after cessation. Additionally, these drugs can have major hematologic disorders, which include granulocytopenia and, in rare instances, aplastic anemia. Other side effects include fever, polyarteritis, and skin rashes. Thyroid Resection. The advantages of surgical ablation of the thyroid include rapid, effective treatment of thyrotoxicosis without necessity for medications and accompanying side effects. The amount of residual tissue is a subject of debate. Complete ablation of thyroid tissue requires a total thyroidectomy, which is associated with the highest rates of hypoparathyroidism and recurrent laryngeal nerve damage. Some groups have reported that total thyroidectomy is the most effective way to treat patients with severe Graves' disease because it offers the lowest rate of relapse. It may be that patients, particularly those with ophthalmopathy, are stabilized most successfully by total thyroidectomy. Removal of the entire antigenic focus may be the most likely explanation for this observation. Other subtotal resections include near-total thyroidectomy or subtotal thyroidectomy, in which one would do a complete lobectomy on one side, leaving a rim of tissue on the contralateral side (near-total procedure) or leaving a rim of tissue on both sides (subtotal technique). One to 2 g of thyroid tissue can be left at the discretion of the surgeon, thereby minimizing risk of damage to the recurrent laryngeal nerve but exposing the patient to some risk of recurrence within this remaining tissue. Patients should be considered for surgery who have had obvious failure of medication or radioiodine treatment. Additionally, younger patients, particularly adolescents, pregnant patients, and patients with suspicious masses contained within the large thyroid, should undergo surgical resection. Patients with severe cosmetic deformities or tracheal compression causing discomfort should also be candidates for resection. Before surgery, it is important to counsel the patient on the risks and options of the surgery, including hypoparathyroidism and recurrent laryngeal nerve damage, as well as on the possibility of relapse if less than a total thyroidectomy is contemplated. The patient should be rendered euthyroid before surgery by use of antithyroid medication and, occasionally, 10 beta-blocker medication. The use of Lugol solution has been recommended for about 7 days before surgery to decrease the vascularity of the thyroid parenchyma. If the patient is not properly treated preoperatively, thyroid storm can be life-threatening. Fortunately, this circumstance is rarely encountered if appropriately anticipated. Thyroid storm is manifested by severe tachycardia, fever, confusion, vomiting to the point of dehydration, and adrenergic overstimulation to the point of mania and coma after thyroid resection in an uncontrolled hyperthyroid patient. Treatment of the patient with overt thyroid storm should include rapid fluid replacement and rapid institution of antithyroid drugs, beta-blockers, iodine solutions, and steroids. In life-threatening circumstances, peritoneal dialysis or hemodialysis may be effective in lowering T 4 and T 3 levels. Toxic Nodular Goiter Toxic nodular goiter, also known as Plummer's disease, refers to a nodule contained within an otherwise goitrous thyroid gland that has autonomous function. This usually occurs in the setting of a patient with endemic goiter. Increased thyroid hormone production occurs independent of TSH control. Such patients usually have a milder course and are older than patients with Graves' disease. The thyroid in such patients may be diffusely enlarged or associated with retrosternal goiters. Presenting symptoms are mild, peripheral thyroid hormone levels are elevated, and TSH levels are suppressed. Antithyroid antibody levels are usually decreased. The diagnosis is usually confirmed after clinical suspicion, and a 131 I radionuclide scan is performed that localizes one or two autonomous areas of function while the rest of the gland shows decreased activity. Treatment of toxic nodular goiter is most effectively performed by resection of the area, usually by lobectomy or near-total thyroidectomy, particularly when clinical symptoms are pronounced. Antithyroid medication can control symptoms, but relapse is common. Radioiodine therapy is not as effective as in patients with Graves' disease. Multinodular Goiter Multinodular goiter describes an enlarged, diffusely heterogeneous thyroid gland. Initial presentation may include diffuse enlargement, but the mass often develops asymmetrical nodularity. The cause of this mass is usually iodine deficiency. Initially, the mass is euthyroid; however, with increasing size, elevations in T 3 and T 4 can occur and 11 progress gradually into clinical hyperthyroidism. Work-up and diagnosis include evaluation of thyroid function tests. Ultrasound and radioisotopic scanning demonstrate heterogeneous thyroid substance. Nodules with poor uptake can present as lesions suspicious for malignancy. The incidence of carcinoma in multinodular goiter has been reported as 5 to 10%. Therefore, FNA for diagnosis and resection for suspicious lesions should be considered. Substernal Goiter Substernal goiter is an unusual presentation of an intrathoracic component of an enlarged thyroid, usually as a result of multinodular goiter. The extremely rare (about 1%) "primary" substernal goiter arises as aberrant thyroid tissue within the anterior or posterior mediastinum and is based on intrathoracic vasculature and not supplied by the inferior thyroid artery. Patients classically present with compressive symptoms involving the trachea or esophagus. Occasionally, diagnosis is incidental based on tracheal deviation seen on chest radiographs. In 10 to 20% of cases, nothing abnormal is found on physical examination with a completely intrathoracic lesion. Work-up should include thyroid function tests and image-guided aspiration. Radioiodine scan can be used to document that the mass contains thyroid tissue. Most substernal goiters can be approached through a cervical incision. The requirement for a mediastinal approach by sternotomy is unusual, although it provides excellent exposure. Complications of surgery include intrathoracic bleeding, recurrence in unresected tissue, and recurrent laryngeal nerve damage, although in experienced hands the complication rate should be less than 5%. Radiologic Evaluation of the Thyroid Thyroid Scintigraphy The use of radionuclide agents has been helpful in delineating the presence, size, and function of thyroid nodules. Two radioactive iodine isotopes have been employed in clinical use. Scanning with 123 I has as its advantage low-dose radiation, (30 mrad) and a short half-life (12 to 14 hours). This compares favorably with the use of 131 I with a higher dose of radiation (500 mrad) and a longer half-life (8 to 10 days). Scanning with 12 123 I is usually used for patients with a suspected lingual thyroid or substernal goiter, whereas 131 I is used in patients with well-differentiated thyroid carcinoma to screen for distant metastasis. Thyroid cancers should have little uptake of the radionuclide; however, this deficient area on scanning could be masked by overlying normally functioning tissue. Malignancy has been shown to occur in 15 to 20% of "cold" nodules and, additionally, in 5 to 9% of nodules with uptake that is "warm" or "hot," mandating continued aggressive approach to clinically suspicious nodules even if they are not "cold." Technetium-pertechnetate-99m ( 99m Tc) is also used for evaluation of thyroid nodules. This substance is trapped by the thyroid but not organified, and it has a short half-life and low radiation dose. Screening with 99m Tc also shows uptake in salivary glands and major vascular structures and, therefore, requires a higher sophistication of interpretation. Thyroid Ultrasound The use of directed cervical ultrasound has as its advantages increasing portability, costeffectiveness, and lack of ionizing radiation. Although ultrasound may add little to the diagnosis of a diffusely enlarged gland, it has become increasingly important in the workup of discrete nodules. Ultrasound is sensitive to delineating solid compared with cystic characteristics, diameter, and multicentricity of nodules. Additionally, enlarged cervical lymph nodes can be assessed for staging of malignancy. B-mode ultrasonography can be used preoperatively or intraoperatively, usually before and sometimes in conjunction with fine-needle aspiration (FNA). . Needle biopsy is now accepted as the most precise diagnostic screening procedure for differentiating benign from malignant thyroid nodules. Because it is safe, inexpensive, and accurate, needle aspiration biopsy is used routinely as the initial diagnostic technique in management of thyroid nodules. With experienced physicians performing needle biopsy and experienced cytopathologists interpreting the results, a reported accuracy of 95 to 97 per cent has been achieved. Several different techniques for performing needle biopsy have been described. Fineneedle aspiration biopsy (FNAB) using a 21- to 25-gauge needle provides a specimen for cytologic study. Large-needle biopsy and cutting-needle biopsy provide tissue for histologic study. The FNAB procedure has emerged as the most widely used technique, 13 since it provides reliable information, has few complications, and is well tolerated by patients. THYROID MALIGNANCIES Thyroid cancer represents less than 1% of all malignancies. Ninety to 95% of thyroid cancer cases are categorized as well-differentiated tumors arising from follicular cell origin. These include papillary, follicular, and Hurthle cell carcinomas. Medullary thyroid cancer accounts for about 6% of thyroid cancers (of which about 20 to 30% are on a familial basis--MEN Types 2A and 2B). Anaplastic carcinoma is an aggressive malignancy and is responsible for less than 1% of thyroid carcinomas. These cases occur primarily in iodine-deficient areas. TABLE 4. Malignant Thyroid Neoplasms Well-differentiated neoplasms Papillary adenocarcinoma Mixed papillary-follicular carcinoma Follicular variant of papillary carcinoma Encapsulated variant Follicular adenocarcinoma Minimally invasive, encapsulated follicular carcinoma Widely invasive, angioinvasive follicular carcinoma Hiirthle cell carcinoma Medullary carcinoma Undifferentiated Spindle and giant cell carcinoma Small cell carcinoma Miscellaneous Lymphoma Squamous cell carcinoma 14 Microepidermoid carcinoma Teratoma Sarcoma Metastatic Thyroid carcinoma occurs with an incidence of approximately 36 to 60 cases per million population per year. These tumors are rare in children and increase in frequency with increasing age. ETIOLOGY: goitrogenic drugs, iodide deficiency, external radiation, radioactive iodide, or a combination of these factors. The histologic type of tumor, size, stage, and age and sex of the patient are all factors that influence prognosis. PATHOLOGY. Patients with papillary or mixed papillary-follicular carcinoma have the most favorable prognosis. Prognosis in follicular carcinoma is slightly less favorable than in papillary carcinoma. Prognosis is generally poorer in patients with medullary carcinoma and is least favorable in those with undifferentiated cancer. STAGE OF TUMOR. Stage I: Tumors with single or multiple intrathyroidal foci. Stage II: Tumors with cervical metastases that are not fixed and without invasion. Stage III: Thyroid tumors with local cervical invasion or fixed cervical metastases. Stage IV: Lesions metastatic outside the neck. Patients with Stage I differentiated carcinomas have a very good prognosis. Palpable nodal metastases are present in only 10 to 20 per cent of adults. If age-matched patient groups are compared, however, the prognosis is better at any age for those patients without nodal metastases. Patients with Stage III cancers with invasion into the adjacent 15 neck structures have a poorer prognosis. The presence of distant metastases is likewise associated with the poorest prognosis. TABLE 32-1 -- Thyroid Nodules Factors Factors Associated Factors Associated That With Worse With Diagnosis Confirm Diagnosis Prognosis Multinodular goiter Surgery -- Hyperthyroidism Iodine-131 scan -- Radiation exposure FNA or surgery Male gender, age > BENIGN Colloid FNA shows colloid and macrophages Hyperfunctioning nodule MALIGNANT Papillary carcinoma 40 yr, size > 3 cm, tall cell variant Previous surgery for papillary carcinoma Follicular carcinoma "Follicular cells" by Permanent FNA section Male gender, age > pathology 40 yr, size > 3 cm, poorly differentiated cell type Medullary carcinoma MEN types 2a and Surgery, FNA 2b Elevated MEN type 2b and sporadic calcitonin Calcitonin levels level 16 TABLE 32-1 -- Thyroid Nodules Factors Factors Associated Factors With Diagnosis Associated That With Confirm Diagnosis Worse Prognosis retOncogene Anaplastic Rapid progression of FNA carcinoma tumor mass Pain, hoarseness Diagnosis Surgery Abbreviations: FNA, fine-needle aspiration; MEN, multiple endocrine neoplasia. Papillary Carcinoma Papillary carcinoma is the most common of the thyroid neoplasms and is usually associated with an excellent prognosis. This is particularly true in female patients younger than 40 years. About 70 to 80% of with thyroid carcinoma have papillary carcinoma. Pathologic Classification The pathologic diagnosis of papillary carcinoma depends on the cytologic findings of well-recognized papillary cytomorphology. The neoplasm may form well-defined follicles with only minimal papillary architecture. The latter group can be classified as the follicular variant of papillary carcinoma. Additionally, the finding of calcified clumps of cells is diagnostic for papillary cancer. Other subtypes of papillary carcinoma are more unpredictably aggressive in their biological behavior. Insular, columnar, and tall cell carcinomas represent these forms of papillary carcinoma. Although these subtypes are rare, they tend to occur in older patients, and the prognosis is predictably worse for these groups. These latter groups represent perhaps less than 1% of all papillary carcinomas. Clinical Presentation 17 Most patients with papillary carcinoma can expect an excellent prognosis, approaching a 95% 10-year survival rate for the most favorable stages. Age younger than 40 years is an important prognostic factor of long-term survival. Women may well extend this age cutoff to 50 years. Absence of distant metastasis at the time of initial treatment and size less than 4 cm are likewise important positive predictors. Tumor size greater than 4 cm and extension of the primary tumor through the capsule of the lesion likewise increase the risk for mortality. Papillary carcinoma may be found incidentally in a thyroid sample resected for a benign process. These carcinomas are usually less than 5 mm in size and are not usually associated with clinically apparent cervical or distant metastatic activity. They may be considered appropriately treated if they are contained within a lobectomy and isthmectomy. Presentation of a palpable mass (1 to 2 cm) strongly suggests a malignant diagnosis. Confirmation of the diagnosis may be initiated by ultrasound, which can evaluate multinodularity and whether the nodule is solid or cystic. FNA of a palpable solid lesion is the next step. Multicentricity can be anticipated in as many as 70% of patients with the diagnosis of papillary cancer. Palpable lymphadenopathy should lead to FNA of suspected lesions. Intraoperative evaluation of any suspicious lymph nodes must also be performed by resection or by frozen-section evaluation. The presence of lymph node metastasis in patients with completely contained intrathyroidal primary papillary carcinoma also does not affect long-term survival. If the final pathology demonstrates extension of a primary papillary carcinoma through the thyroid capsule, a poor prognosis and possibly a higher rate of lymph node metastasis may be anticipated. Treatment The main treatment of papillary carcinoma of the thyroid is surgical ablation. For lesions smaller than 1 cm, there is general agreement in the literature that lobectomy plus isthmectomy is the appropriate treatment. This is particularly true for incidentally found papillary carcinomas. Several factors enter into surgical decision making. Younger patients, particularly those 15 years of age or younger, have a high rate of cervical metastasis. Patients in this age group undergo total thyroidectomy and lymph node dissection if palpable cervical lymph 18 nodes occur. Additionally, in older patients with a history of neck irradiation, a more aggressive approach may be taken, including total thyroidectomy and modified neck dissection in the presence of palpable cervical lymph nodes. In patients between the ages of 15 and 40 years with lesions smaller than 2 cm, surgical treatment is more controversial. Some surgeons perform total thyroidectomy in any event; however, there is sufficient literature that shows that lobectomy and isthmectomy may well suffice when the lesion clearly involves only one lobe. For adults with lesions larger than 2 cm, a total or near-total thyroidectomy is favored by most surgeons. In patients of any age in whom there is palpable adenopathy, a modified radical neck dissection on the side affected should be performed in concert with a total thyroidectomy. The advantages of a total thyroidectomy include the efficient use of radioiodine postoperative treatment. Clearly, if residual thyroid exists, radioablation is much less effective and requires a larger dosage. The advantages of the lesser procedure are the decreased rates of bilateral recurrent laryngeal nerve damage and hypoparathyroidism. If the papillary carcinoma presents as a palpable lesion larger than 2 cm, a more aggressive surgical resection, including a total thyroidectomy, should be considered. For patients with lower-stage disease, surgical resection should result in an excellent 5- to 10-year survival rate exceeding 90%. For larger lesions, survival numbers may decrease, especially in older men. For larger lesions, postoperative 131 I therapy has been advocated Follicular Carcinoma Follicular thyroid cancer (FTC) is the second category of well-differentiated thyroid cancers. FTC is a disease of an older population, often 50 years of age or older. It has a predilection for women, with a ratio of about 3:1. Pathologic Classification FTC is a malignant neoplasm of the thyroid epithelium, which can present as a wide spectrum of microscopic changes anywhere from virtually normal follicular architecture and function to severely altered cellular architecture. The histologic diagnosis of FTC depends on the demonstration of what would appear to be normal follicular cells occupying abnormal positions, including capsular, lymphatic, or vascular invasion. If well-differentiated follicular cells are not demonstrated to involve these structures, a 19 diagnosis of a benign follicular adenoma is made. Using these criteria, two types of follicular carcinoma are usually described: minimally invasive and widely invasive. In both cases, lymph node involvement is unusual, occurring in less than 10% of cases. For widely invasive FTC, which frequently disseminates hematogenously, distant spread is more common, often involving lung, bone, and other solid organs, such as brain and liver. Clinical Presentation FTC, like papillary cancer, classically presents as a painless thyroid mass. The coexistence of lymph node involvement is extremely rare and cervical adenopathy even less so, perhaps occurring in less than 5% of patients. Diligent search for aggressive extension into the trachea and distant metastasis, particularly in older patients, should be carried out by use of computed tomography or magnetic resonance imaging evaluation of the neck and chest. Laboratory work-up usually reveals a euthyroid state. Thyroid malignancies are almost never associated with hyperfunctioning or hypofunctioning tissue. Preoperative imaging may be of some assistance to assess the extent of a palpable mass. Ultrasound can determine the size and multicentricity; however, FTC usually presents as a solitary mass. Radionuclide scanning can determine whether a mass has function or is cold, although a minority of cold nodules actually proves to be malignant. The use of FNA cytology has been of immense help in arriving at a cytologic diagnosis before surgery. In the case of FTC, however, FNA is of limited value. The diagnosis of FTC requires the demonstration of cellular invasion of the capsule or of vascular or lymphatic channels. This cannot be determined through the use of preoperative FNA. Additionally, intraoperative frozen section has been notoriously ineffective in making a definitive diagnosis of FTC. Treatment The treatment of follicular carcinoma is primarily surgical. If the lesion is 2 cm or smaller and well contained within one thyroid lobe, an argument may be made for thyroid lobectomy and isthmectomy. If the lesion is larger than 2 cm, the surgeon may well proceed with total thyroidectomy. If the follicular lesion is larger than 4 cm, the risk for cancer is greater than 50%; therefore, total thyroidectomy is an obvious choice. Lymph 20 node dissection is not necessary in the absence of palpable lymph nodes and adds nothing to survival data unless obviously involved. Prognosis after treatment for FTC is dependent on age. Patients younger than 40 years of age have the best prognosis, approaching 95% at 5 and 10 years. Series that compare follicular carcinoma with papillary carcinoma have shown poorer prognosis for FTC, although this disparity is more prominent after 10 to 15 years. Poorly differentiated FTC and well-differentiated FTC have 60% and 80% 10-year survival rates, respectively. Postoperative treatment with T 4 is based on the assumption that TSH suppression minimizes its growth-promoting influence on thyroid cancer. The literature does not completely agree about the efficacy of thyroid suppression. In fact, more recent studies have demonstrated that overaggressive treatment with T 4 may have unproved effects on FTC recurrence and significant enhancement of osteoporotic side effects. Radioiodine treatment is likewise controversial. Obviously, radioiodine treatment is most efficacious in patients who have undergone total thyroidectomy. In patients who have undergone subtotal thyroidectomy or lobectomy and isthmectomy, higher doses of radioiodine are needed for remnant ablation. The use of postoperative radioiodine ablation appears to be warranted in more advanced-stage FTC patients. Additionally, 131 I treatment may be given in older patients (75 years of age or older) or in patients whose thyroglobulin levels have increased later than 3 months after surgery. Hurthle Cell Carcinoma Hurthle cell carcinoma is a subtype of follicular carcinoma that closely resembles FTC both grossly and on microscopic examination. The tumor contains an abundance of oxyphilic cells, or oncocytes. The pathologic criteria for malignancy including vascular and capsular invasion are the same as for follicular carcinoma; in the absence of these changes, Hurthle cell tumors should be considered benign. Some studies have suggested that Hurthle cell carcinoma may have a worse clinical prognosis than standard FTC; however, there is no uniform agreement on these findings. It does appear that Hurthle cell carcinoma may have a higher rate of recurrence, particularly in regional lymph nodes. Most studies consider Hurthle cell carcinoma to be clinically and prognostically equivalent to FTC. 21 Prognosis and Treatment Hurthle cell carcinoma presents in much the same fashion as follicular cell neoplasms. Malignant Hurthle cell lesions are generally considered to be more aggressive than other well-differentiated thyroid carcinomas metastasizing to both regional lymph nodes and distant sites and demonstrating a high local recurrence rate after resection. The treatment is surgical, following the same principles as the work-up of the follicular neoplasm. Management usually requires total thyroidectomy with node dissection. Medullary Carcinoma MCT accounts for 5 to 10% of thyroid malignancies. The malignancy involves the parafollicular cell, or C cell, derived from the neural crest. MCT is associated with the secretion of a biological marker, calcitonin. The excess secretion of calcitonin has been demonstrated to be an effective marker for the existence of MCT. Interestingly, the calcitonin excess is not associated with its exaggerated clinical activity, hypocalcemia. Medullary carcinoma can occur in a sporadic form or as part of MEN Type 2A or 2B. Presentation The patient with a sporadic medullary carcinoma may present in either of two ways: with a palpable mass for which a diagnosis can be made through FNA or with the finding of an elevated calcitonin level. In sporadic MCT, the tumors are usually single and unilateral and have no familial predisposition. The presence of both a mass and an elevated calcitonin level is certainly diagnostic of MCT, whereas the finding of an elevated basal calcitonin level in the absence of a thyroid mass might require a further work-up, including repeat basal calcitonin measurement and the completion of a calciumstimulated or gastrin-stimulated test. The work-up of these patients should include a detailed and in-depth family history inquiring for characteristics of MEN Type 2 in the patient and family members. Treatment The surgical approach to sporadic medullary carcinoma involves at least a total thyroidectomy with or without central lymph node dissection. The total thyroidectomy allows complete removal of the gland and search for multicentricity. The literature has described some uses of basal and stimulated calcitonin tests to follow recurrence because the stimulated calcitonin values may rise before the basal calcitonin levels. 22 Unfortunately, documentation by biochemical means of recurrent MCT is often associated with unresectable recurrence in distant metastatic locations, including lung and liver. Anaplastic Thyroid Cancer Anaplastic thyroid carcinoma represents less than 1% of all thyroid malignancies. It is the most aggressive form of thyroid cancer. A typical presentation is in an older patient who presents with dysphagia, cervical tenderness, and a painful neck mass. Superior vena cava syndrome can also be part of the presentation. The clinical situation deteriorates rapidly into tracheal obstruction and rapid local invasion of surrounding structures. Pathology Grossly, the tumor can appear as locally invasive, with a hard, firm, whitish appearance. On microscopic evaluation, giant cells with intranuclear cytoplasmic invaginations can be seen. There is a wide variety of cell types, ranging from moderately differentiated to extremely poorly differentiated cell types. Occasionally, squamous cell elements or islands of more recognizable differentiated thyroid carcinoma, such as papillary carcinoma, can be identified within the locus of the tumor. This has led to the speculation that anaplastic carcinoma might arise from well-differentiated carcinoma; however, there has been no solid proof of this theory. Treatment The results of any surgical treatment of anaplastic thyroid carcinoma are tempered by the rapidly progressive clinical course. Most reports with resection are not optimistic. If anaplastic carcinoma initially presents with a resectable mass, some small improvement in survival may be made. The finding of distant metastasis or invasion into locally unresectable structures, such as the trachea or vasculature of the anterior mediastinum, should lead to a more conservative surgical approach, such as tracheostomy. Lymphoma Primary thyroid lymphoma, although rare, is being recognized with more frequency. This diagnosis should be considered in patients who present with a goiter, especially one that has apparently grown significantly in a short period of time. Other presenting symptoms include hoarseness, dysphagia, and fever. There is also an increased association between 23 lymphoma and Hashimoto's thyroiditis. There has been no correlation seen in thyroid lymphoma with neck irradiation or with human immunodeficiency virus infection. Work-Up and Diagnosis Because these patients present rarely, the standard work-up for thyroid mass or goiter has usually been completed. There is evidence that ultrasound may have a classic "pseudocystic pattern." The use of FNA can be diagnostic in this situation. The use of flow cytometry for monoclonality can confirm the diagnosis. In some series, FNA is associated with an accurate diagnosis in as many as 78% of cases. If FNA is nondiagnostic, the use of core-needle biopsy or open biopsy can be considered. If the diagnosis is either confirmed or highly suspicious, additional preoperative evaluation should include neck, chest, and abdominal computed tomography or magnetic resonance imaging evaluation to assess extrathyroidal spread. Treatment Treatment philosophies differ with regard to preoperative chemotherapy or surgical ablation. The use of the CHOP regimen (cyclophosphamide, doxorubicin [Adriamycin], vincristine, and prednisolone) has been associated with excellent survival. The use of surgical resection, including a near-total or a total thyroidectomy, is thought to enhance these results. It must be noted that thyroidectomy, especially the near-total or total procedures, is daunting in these cases. There can be a significant amount of pericapsular edema and swelling with loss of normal tissue planes. Bleeding, parathyroid damage, and recurrent laryngeal nerve damage can occur with increased predictability in such cases. LITERATURE Shot Practice of surgery by Charles v. Mann and al. Textbook of surgery by Sabiston. Lections. APPROXIMATE ACTIONS BASE 1. Introduction /5 min/. Teacher short characterizes topic actuality, meets students with main aims of the study and plan. 2. Initial knowledge’s control /15 min/. 24 3. Individual students work with patients /30 min/. The teacher explains some more difficult and important parts of problem. The choice is realized by asking of students and their answers correction. 4. Clinical analyses of topical patients /100 min/. Students observe topical patients under teaches control. After it finishing, the students report about receiving results. 5. Work in dressing-room and operation theater. Teacher and students change the dressings of patients after different surgical procedures on esophagus. 6. Study of X-ray pictures. 7. Final knowledge control. Solution of test-questions /25 min/. 8. Conclusion /5 min/. The teacher concludes the session and gives new task for the next once. TEST – QUESTIONS What factors influence survival in patients with thyroid cancer? Age / Sex / Size of tumor/ Stage/ Histologic type of tumor/ Classic triad of Graves’ disease include the following: Goiter/ Thyrotoxicosis/ Hypothyroidism Exophthalmos/ Cardiac failure What the main ocular consequences of untreated thyrotoxicosis? Proptosis/ Conjunctival swelling/ Spasm of the upper eye lid/ Ophthalmoplegia/ Diplopia/ 25 Choose the main instrumental methods for evaluation of the thyroid pathology: Ultrasound/ Computer tomography/ Esophagoscopy X-ray examination Radionuclide scan/ Thyroid function tests/ What the methods of treatment are employed in patients with Graves’ disease? Radionuclide therapy/ Antithyroid medication/ Replacement therapy Thyroid resection/ Chemotherapy Note the causes of hypothyroidism: Hashimoto’s thyroiditis/ Lack iodine intake/ Aggressive radioactive iodine therapy/ Aggressive surgical ablation/ Inherited defects in thyroid hormone synthesis/ Hypothalamic disorders and anterior pituitary gland disease/ Peripheral tissue hormone resistance/ Drag-related alterations of thyroid function/ Choose the main complications of the total thyroidectomy Hypoparathyroidism/ Hypothyroidism/ Recurrent laryngeal nerve damage/ Cervical esophagus damage Bleeding In case of thyroid storm the urgent treatment should be the following Fluid replacement/ Blood replacement 26 Antithyroid drugs/ Beta-blockers/ Iodine solutions/ Steroids/ Haemostatic drugs What kind of thyroid cancer damage regional lymphnodes more often? Follicular carcinoma Papillary carcinoma/ Medullary carcinoma Anaplastic cancer Distant hematogenous spread of metastasis is more common for: Follicular carcinoma/ Papillary carcinoma Medullary carcinoma Anaplastic cancer What organs are damaged by distant metastasis more often? Lung/ Bone/ Brain/ Liver/ The main principles of thyroid cancer treatment include: Total thyroidectomy/ Thyroid lobectomy Radiodine postoperative treatment/ Postoperative TSH suppressive therapy with T 4/ 27