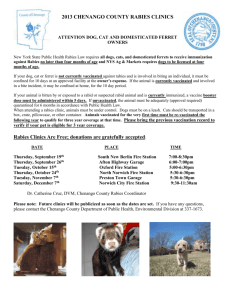
General Rabies Info
advertisement

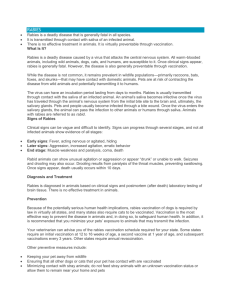
RABIES Rabies is a disease that is transmitted to humans from animals and that is caused by a virus. The disease infects domestic and wild animals, and is spread to people through close contact with infected saliva via bites or scratches. Once symptoms of the disease develop, rabies is nearly always fatal. Symptoms The incubation period for rabies is typically 1-3 months, but may vary from 1 week to 1 year. The early symptoms or rabies are similar to that of many other illnesses, including fever, headache, and general weakness or discomfort. As the disease progresses, more specific symptoms appear and may include insomnia, anxiety, confusion, slight or partial paralysis, excitation, hallucinations, hypersalivation (increase in saliva), difficulty swallowing, and hydrophobia (fear of water). Death usually occurs within days of the onset of these symptoms. Diagnosis No tests are available to diagnose rabies infection in humans before the onset of clinical disease, and unless the rabies-specific signs of hydrophobia are present, the clinical diagnosis may be difficult. Transmission People are infected through the skin following a bite or scratch by an infected animal. Dogs are the main host and transmitter of rabies. They are the source of infection in all of the estimated 55 000 human rabies deaths annually in Asia and Africa. Transmission can also occur when infectious saliva comes into direct contact with fresh skin wounds. Treatment after exposure Effective treatment soon (within a few days, but as soon as possible) after exposure to rabies can prevent the onset of symptoms and death. Post-exposure prevention consists of local treatment of the wound, administration of rabies immunoglobulin and immediate vaccination. Local treatment of the wound Removing the rabies virus at the site of the infection by chemical or physical means is an effective means of protection. Therefore, prompt local treatment of all bite wounds and scratches that may be contaminated with rabies virus is important. Recommended first-aid procedures include immediate and thorough flushing and washing of the wound for a minimum of 15 minutes with soap and water, detergent, or other substances that kill the rabies virus. Recommended treatment The recommended post-exposure prophylaxis depends on the type of contact with the suspected rabid animal: Category of exposure to suspect rabid animal Category I – touching or feeding animals, licks or intact skin Category II - nibbling of uncovered skin, minor scratches or abrasions without bleeding Category III – single or multiple transdermal bites or scratches, licks on broken skin Post-exposure measures None Immediate vaccination and local treatment of the wound Immediate vaccination and administration of rabies immunoglobulin; local treatment of the wound Who is most at risk? People most a risk live in rural areas where human vaccines and immunoglobulin are not readily available or accessible. Although all age groups are susceptible, rabies is most common in children aged fewer than 15. Prevention Rabies is a vaccine- preventable disease. The most effective strategy for preventing rabies in people is by eliminating rabies in dogs through vaccination. Immunization in people is recommended for travelers to high-risk areas in rabies affected countries (rabies is endemic in Afghanistan), and for people in certain high-risk occupations such as laboratory workers, veterinarians and animal handlers in rabiesaffected areas.