5.0 Documentation
advertisement

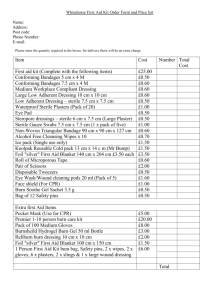
Central Venous Catheter (CVC): Dressing Change & Exit Site Care (Approved Aug 15, 2011/Rev Dec 16, 2011/Rev Jun 17, 2012) Vascular Access Guideline Table of Contents This procedure is posted on the BC Provincial Renal Agency website – Health Professionals Channel – Vascular Access – http://www.bcrenalagency.ca/professionals/VascularAccess/ProvGuide.htm 1.0 2.0 3.0 4.0 5.0 6.0 7.0 8.0 Practice Standard ...........................................................................................................1 Equipment ......................................................................................................................3 Assessment & Interventions ..........................................................................................3 Patient Education & Resources ......................................................................................4 Documentation ..............................................................................................................5 References ......................................................................................................................5 Developed By .................................................................................................................6 Reviewed By ...................................................................................................................6 1.0 Practice Standard Skill Level (Nursing): Specialized The following Registered Nurses (RNs) and Licensed Practical Nurses (LPNs) may perform this procedure: 1. RNs and LPNs who have completed the required hemodialysis (HD) specialty education and who provide nursing care in a BC In-Centre and/or Community Renal Program; & 2. Designated RNs and LPNs who have received the appropriate training for CVC care including dressing changes (e.g., inpatient, home care or ambulatory care RNs or LPNs). Need to Know: 1. Check the exit-site dressing every HD treatment. If required, change the dressing. 2. The frequency of dressing change depends on the type of dressing used. a. Sterile gauze dressing: change every hemodialysis treatment (every 48 hours) or if dressing is damp, loose or soiled. Gauze dressings are recommended if the patient is diaphoretic or the site is bleeding, oozing, or showing signs of infection, or the skin is compromised. Approved Aug 15, 2011/Rev Dec 16, 2011/Rev Jun 17, 2012 Page 1 CVC: Dressing Change & Exit Site Care b. Sterile, transparent dressing: change every 7 days or if the dressing is damp, loose or soiled. 3. When changing the dressing, check the catheter is secure: a. Non-tunneled (temporary uncuffed) catheters: secured by at least one suture for the entire time catheter is in-situ. b. Tunneled (cuffed) catheters: i. Neck sutures are removed on DAY 7 post insertion (or as per unit policy). ii. Anchoring sutures are removed on WEEK 6 post insertion (or as per unit policy). 4. Standard/routine precautions are used for dressing changes to reduce the risk of transmission of blood-borne and other pathogens. Wash hands before and after manipulation of the CVC and administration lines. If hands visibly soiled, wash with antimicrobial soap; if not, may use either an antimicrobial soap or alcohol hand sanitizer. Wear gloves (non-sterile for removal of old dressing and sterile gloves for the rest), non-sterile gown and non-sterile mask/face shield during dressing changes. If institution policy is for a clean “no touch” procedure, then may wear non-sterile gloves and change as indicated. 5. Medical/clean aseptic technique is used for dressing change procedures, with additional precautions as follows: Use sterile equipment and supplies and a “no touch” technique when caring for the exit site and handling the catheter and catheter ports. Maintain a sterile drape/gauze under the catheter ports. 6. Recommended antiseptic solutions, in order of priority: Solution Chlorhexidine gluconate 2% with alcohol Chlorhexidine gluconate without alcohol Sodium hypochlorite 0.11% (ExSept Plus®) or Amuchina 10% Povidone-iodine 10% (Betadine) Required Drying Time 30 seconds (persistent antimicrobial activity, up to 48 hours) 2 minutes 2 minutes 2 minutes 7. If infection is suspected, swab the catheter exit site for culture and sensitivity (C&S) and consult with the physician. Approved Aug 15, 2011/Rev Dec 16, 2011/Rev Jun 17, 2012 Page 2 CVC: Dressing Change & Exit Site Care 2.0 Equipment Non-sterile gloves Non-sterile gown Non-sterile mask/eye protection (2) Sterile gloves (2 pair) Sterile dressing tray Sterile drape/gauze (or sterile 4x4) 4 x 4 sterile gauzes (several) Antiseptic solution, preferably chlorhexidine gluconate 2% with alcohol Dressing (gauze or transparent) Normal saline & C&S swab (if required) Antibiotic ointment (if ordered) Garbage receptacle 3.0 Assessment & Interventions Preparation: 1. Wash hands with antimicrobial soap. 2. Don non-sterile gown (staff). 3. Don non-sterile mask (staff and patient). 4. Open sterile dressing tray and add supplies. 5. Don non-sterile gloves (staff) 6. Remove exit site dressing and examine site for signs and symptoms of infection (e.g., redness and/or discharge). Palpate the site for tenderness using a sterile 4x4 gauze. If signs and symptoms of infection are present, cleanse the exit site area with normal saline and swab for culture and sensitivity (C&S). 7. Check that the catheter is secured. 8. Discard the dressing. 9. Remove gloves and wash hands with antimicrobial soap. 10. Place the patient supine in as flat a position as the patient can comfortably tolerate. 11. Don sterile gloves. 12. Using a dry, sterile 4x4 gauze, grasp the catheter ports with one hand and place a sterile drape under the ports with the other hand. Discard 4x4 that was used to grasp the ports. Approved Aug 15, 2011/Rev Dec 16, 2011/Rev Jun 17, 2012 Page 3 CVC: Dressing Change & Exit Site Care Care of exit site: 13. Using a sterile 4x4 gauze soaked in an antiseptic solution, cleanse the catheter exit site skin using a back and forth friction motion that covers a 5 cm x 5 cm area. Discard used gauze. 14. Air dry (see point #6 under “need to know” for drying time). Apply dressing: 15. Apply sterile gauze or transparent occlusive dressing as per unit policy. 16. If C&S taken, send to the laboratory and notify the physician of suspected infection. Once results are available, consult with the physician re next steps. 4.0 Patient Education & Resources Keep dressing clean and dry – a tub bath is the best way to wash. If the dressing peels off or gets wet, wash hands well and remove what is left of the dressing. Put on a clean, dry 4x4 gauze and tape in place. Come to dialysis unit to have a proper dressing applied unless given explicit instructions from health care team on changing own dressing. Notify kidney doctor (nephrologist) or dialysis unit for any of the following: Redness, warmth, or pain along the catheter. Oozing or drainage from catheter exit site. Noticeable swelling or itching around catheter or neck. Feverish and any of the above symptoms. Part of the catheter that is outside the skin seems to be getting longer. Catheter is accidentally pulled and there is bleeding around the exit site. If the gauze around the ports is damp for an unknown reason. Resource: Care of Your Catheter http://www.bcrenalagency.ca Approved Aug 15, 2011/Rev Dec 16, 2011/Rev Jun 17, 2012 Page 4 CVC: Dressing Change & Exit Site Care 5.0 Documentation Document exit site status and dressing change as per unit protocol. Document that physician was notified (also input into PROMIS) if a swab is sent for C&S. Document actions following receipt of C&S results. 6.0 References 1. Besarab, A., and Brouwer, D. (2004). Aligning hemodialysis treatment practices with the National Kidney Foundation’s K/DOQI vascular access guidelines. Dialysis & Transplantation, 33 (11): 694 – 702. 2. BC Provincial Renal Agency Guideline, Prevention, Treatment, & Monitoring of VA Related Infection in HD Patients (March 2008). http://www.bcrenalagency.ca 3. BC Provincial Renal Agency Patient Teaching Pamphlet, Your Catheter (2008). http://www.bcrenalagency.ca 4. Canadian Society of Nephrology Guidelines: Vascular access. (2006). Journal of American Society of Nephrology, 17: S18 - S21. 5. O’ Grady et al. (2011). Guidelines for the prevention of intravascular catheter- related infections. Centre for Disease Control (US). 51 (RR-10): 1-26. 6. Count, Caroline. (Ed). (2008). Core Curriculum for Nephrology Nursing. American Nephrology Nurses’ Association; Pitman, NJ. 7. Marschall, Jonas et al. (2008). Strategies to Prevent Central Line-Associated Bloodstream Infections in Acute Care Hospitals, Infection Control and Hospital Epidemiology, 29: supp 1, S22-S30. 8. National Kidney Foundation (2006). KDOQI Clinical Practice Guidelines and Clinical Practice Recommendations for 2006 Updates: Hemodialysis Adequacy, Peritoneal Dialysis Adequacy and Vascular Access. Am J Kidney Dis 48:S1-S322, 2006 (suppl 1). 9. O’Grady, Naomi et al. (2002). Prevention Guidelines for Catheter-Related Infections, Clinical Infection Diseases, 24: 1281-307 Approved Aug 15, 2011/Rev Dec 16, 2011/Rev Jun 17, 2012 Page 5 CVC: Dressing Change & Exit Site Care 10. Registered Nurses Association of Ontario, Care and Maintenance to Reduce VA Complications. (2008). http://www.rnao.org/Storage/39/3381_Care_and_Maintenance_to_Reduce_Vascular_ Access_Complications._with_2008_Supplement.pdf 11. Safer Healthcare Now! Campaign. (2006). How-to-Guide: Prevent Central Line Infections. http://www.saferhealthcarenow.ca 7.0 Developed By 1. BCs Vascular Access Educators Group (VAEG). 2. Adapted from Fraser Health and Providence Health Care Renal Program guidelines/standards. 8.0 Reviewed By 1. British Columbia Renal Educators Group (BCREG) 2. BC Provincial Renal Agency – Medical Advisory Committee (MAC) Approved Aug 15, 2011/Rev Dec 16, 2011/Rev Jun 17, 2012 Page 6