TRIGGERS FOR INTERDISCIPLINARY REFERRALS
advertisement
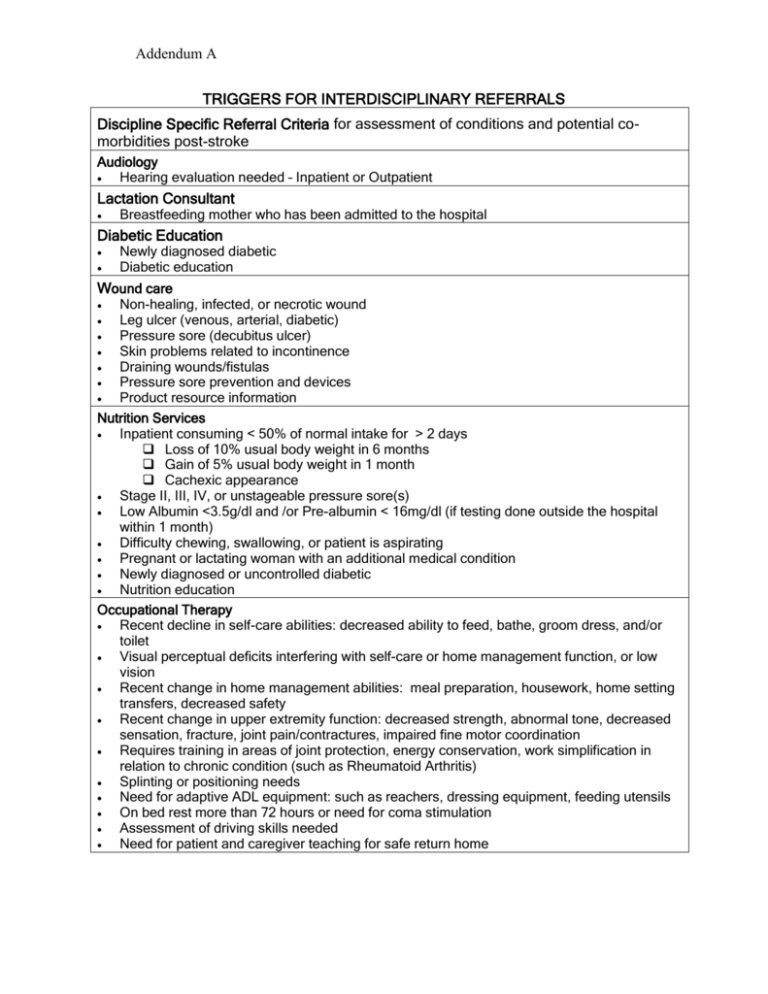
Addendum A TRIGGERS FOR INTERDISCIPLINARY REFERRALS Discipline Specific Referral Criteria for assessment of conditions and potential comorbidities post-stroke Audiology Hearing evaluation needed – Inpatient or Outpatient Lactation Consultant Breastfeeding mother who has been admitted to the hospital Diabetic Education Newly diagnosed diabetic Diabetic education Wound care Non-healing, infected, or necrotic wound Leg ulcer (venous, arterial, diabetic) Pressure sore (decubitus ulcer) Skin problems related to incontinence Draining wounds/fistulas Pressure sore prevention and devices Product resource information Nutrition Services Inpatient consuming < 50% of normal intake for > 2 days Loss of 10% usual body weight in 6 months Gain of 5% usual body weight in 1 month Cachexic appearance Stage II, III, IV, or unstageable pressure sore(s) Low Albumin <3.5g/dl and /or Pre-albumin < 16mg/dl (if testing done outside the hospital within 1 month) Difficulty chewing, swallowing, or patient is aspirating Pregnant or lactating woman with an additional medical condition Newly diagnosed or uncontrolled diabetic Nutrition education Occupational Therapy Recent decline in self-care abilities: decreased ability to feed, bathe, groom dress, and/or toilet Visual perceptual deficits interfering with self-care or home management function, or low vision Recent change in home management abilities: meal preparation, housework, home setting transfers, decreased safety Recent change in upper extremity function: decreased strength, abnormal tone, decreased sensation, fracture, joint pain/contractures, impaired fine motor coordination Requires training in areas of joint protection, energy conservation, work simplification in relation to chronic condition (such as Rheumatoid Arthritis) Splinting or positioning needs Need for adaptive ADL equipment: such as reachers, dressing equipment, feeding utensils On bed rest more than 72 hours or need for coma stimulation Assessment of driving skills needed Need for patient and caregiver teaching for safe return home Addendum A Pastoral Care Patient/Family Support: Serious injury, illness, major surgery, long term hospitalization or treatment, cardiopulmonary arrest, or death Patient requests a Sacrament, prayer, or other spiritual support Ethical decisions Advance directives (at some facilities) Pharmacy Services Patient or family requests more information about medications Evaluation for possible adverse drug reactions, food-drug interactions, or drug-drug interactions Physical Therapy Recent change in mobility: Difficulty moving from/to bed, chair, tub, toilet; balance problems; safety concerns Recent change in ambulation: Difficulty walking (or with stairs) with or without a device; recent history of falls Positioning needs due to wounds, pressure ulcers, musculoskeletal issues Uncontrolled back, neck, or extremity musculoskeletal pain Amputated limb: new amputation or improperly fitting prosthesis Recent change in function related to decreased strength, fracture, altered muscle tone range of motion, joint movement or sensation. Edema in trunk or extremities On bed rest more than 72 hours: excessive decrease in endurance Requires assistance to procure and training for the use of a wheelchair Requires patient and caregiver training for safe return home Rehabilitation Psychology Anxiety management Assessment of competency Assessment of dementia Change in mental status/cognitive functioning Assessment of suicidal ideation, mood disturbances Emotional lability Depression Lack of motivation/participation Agitation/combativeness with need for behavior modification Respiratory Care Respiratory compromise Patient requires artificial airway Patient unable to perform Incentive Spirometry or deep breathing and coughing exercises independently or with RN’s assistance Patient on respiratory treatments at home CPAP/BIPAP Home ventilators Home nebulizer therapy Social Services/Case Management Abuse, neglect, or domestic violence Advance directives: assistance and problem solving Community resource needs (meals on wheels, transportation, adult day care, etc.) Potential need for: rehab, subacute, long term acute care, home care, nursing home, group home, hospice, etc. Resume prior services: nursing home, group home, home care meals, etc. Diminishing capacity for self care, frail, or living alone with marginal or no support system Homelessness/shelter needs Altered mental status with potential for continuing care needs Patient is caregiver to another person Addendum A Patient’s caregiver having difficulty coping Psychosocial needs: adjustment to illness, grieving, patient/family conflict interfering with care ETOH abuse identified on the database (referral may also be made to Psych) Speech Therapy Recent change in swallowing ability: difficulty chewing, choking when eating/drinking, residual food in mouth and/or aspiration suspected Admitting diagnosis of aspiration pneumonia Recent change in communication or cognitive skills: Difficulty with verbal or written expression Reduced understanding of spoken word or written word Slurred speech Decreased fluency with speech Inappropriate responses to questions Decreased attention, memory, problem solving or judgment Decreased safety awareness Tracheotomy or is otherwise non-verbal and requires communication intervention Change in voice quality (hoarseness, reduced intensity, etc.) Therapeutic Recreation Major lifestyle changes as a result of illness or injury affecting leisure and community interests, employment, and/or life roles Plan to return to community living with any above deficit