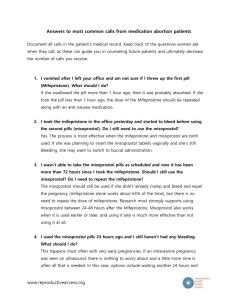
Malawi Misoprostol Protocol.
advertisement

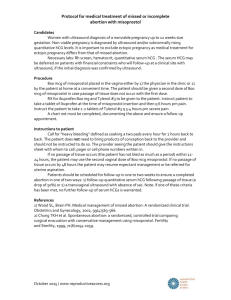
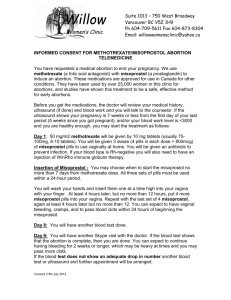
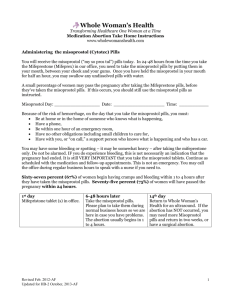
MISOPROSTOL FOR MANAGEMENT OF INCOMPLETE ABORTION A CLINICAL PROTOCOL FOR SERVICE DELIVERY ACKNOWLEDGEMENTS To be acknowledged - reviewers, sponsors, etc. Edgar Kuchingale, Shirley Lengu Alick Mazenga Joachim Osur Joseph Karanja Charles Kiggundu Monica Ogutu Emily Nakirija INTRODUCTION Data and information from various researches indicate that, compared to other countries, Malawi still has poor reproductive health indicators. One of the indicators is Maternal Mortality Ratio (MMR). According to Malawi Demographic and Health Surveys (MDHS) the MMR for Malawi rose from 620 deaths per 100,000 live births (1992) to 1,120 deaths per 100,000 live births (2000) and declined to 984 deaths per 100,000 live births (2004). The most recent estimates released by World Health Organization (WHO) and partners have ranked Malawi at 1,100 maternal deaths per 100,000 live births. Puerperal sepsis contributes 25% of all maternal deaths making it the number one cause of all maternal deaths in Malawi. Unsafe abortion contributes significantly to all cases of puerperal sepsis and obstetric haemorhage. Post abortion complications contribute to about 60% of all admissions to our hospitals. USE OF MISOPROSTOL IN POST ABORTION CARE Misoprostol, if used for treatment of incomplete abortion, promises to have an important public health impact. Women and health care systems world-wide could significantly benefit from this non-invasive treatment option. In low resource countries, where infection, hemorrhage and uterine damage are far too commonly reported as consequences of (poor) surgical care, misoprostol treatment of incomplete abortion would be tremendous step towards reducing morbidity and mortality due to abortion complications worldwide. This method promises to greatly improve access to services, by enabling women to seek appropriate, effective care at secondary and even primary healthcare facilities, with nonsurgically trained, mid- level providers. At the same time, misoprostol for incomplete abortion and miscarriage could decrease the burden on tertiary health care facilities, and reduce costs to health care systems worldwide. It could limit the burden on skilled equipment and supplies, surgical wards, sterilization and anesthesia. Misoprostol treatment also has the additional benefit of being highly acceptable to women as it is less medicalized and less invasive than standard surgical treatment. MISOPROSTOL DRUG Misoprostol is a stable, widely available and inexpensive prostaglandin analogue, initially manufactured for use in peptic ulcer disease. Misoprostol however has many uses in obstetrics and gynaecology (Goldberg et al 2001, WHO 2003). Gynaecological uses include induction of labour, induction of abortion (as a single agent or in combination with mefeprestone), postpartum haemorrhage and emptying the uterus in cases of incomplete abortion in the first trimester. In uterine evacuation in incomplete abortion Misoprostol works by interacting with prostaglandin receptors and causes the cervix to soften and the uterus to contract, resulting in the expulsion of the uterine contents. Misoprostol is a safe and effective alternative to surgical evacuation of the uterus for first trimester incomplete abortion. The misoprostol alone protocol involves two outpatient clinic visits. First Visit Clinical Assessment 1. Confirm diagnosis of otherwise uncomplicated first trimester incomplete abortion Amenorrhea in a woman of reproductive age Uterus equal to or less than 12 weeks by bimanual examination Cervix open, POCs felt or reported to have been passed, active vaginal bleeding Clinically stable, not in shock, no severe anaemia, no severe uterine infection 2. If client has any of the following contraindications, Misoprostol should not be used, and an alternative method of management should be offered: Allergy to misoprostol or other prostaglandins Confirmed or suspected ectopic pregnancy Unstable haemodynamic status or shock Signs of pelvic infection and/or sepsis 3. Use caution when There is an IUCD in place. Remove before administration of misoprostol The woman has coagulation problem or other unstable health problem. Timely uterine evacuation with (e.g. using MVA) with careful monitoring is preferred. Counselling – to include: All treatment options available Their risks and benefits What to expect with each method: bleeding, cramping, analgesia, need for follow up, pain medication provided. Medication method of evacuation may take several hours to several weeks to complete. Most complete within 2 days. Patience, patience, patience, is necessary Complications are very rare but can occur. Advise the woman to seek medical attention immediately if she experiences prolonged heavy bleeding (soaking through more than 2 pads in an hour), or fever, malaise, and foul-smelling discharge. Provide information on who to call or where to go if she is concerned. In the event of the few cases where medication does not work MVA will be necessary. Most family planning methods can be started at the time of initiating misoprostol e.g. the pill, injection, and implant. IUD needs confirmation of completion of evacuation before it can be started, and can be inserted during the follow up visit. Inform that fertility returns rapidly after the treatment. Routine Antibiotic Prophylaxis is not indicated for medication management of incomplete abortion. Standard Regimen 1. The current recommended standard regimen is 600 mcg of misoprostol orally 2. Alternative regimen: 400 mcg sublingually. There is as yet less evidence on this regimen but it may be useful where misoprostol supply is limited. For sublingual use, the pills are placed under the tongue for 30 minutes then swallowed. 3. Buccal route may also be effective. The standard regimen (#1) will be used in this protocol. Three 200mcg tablets of misoprostol will be administered under direct observation and the woman will be observed for 30 minutes before she is discharged home. Pain medication e.g. tabs paracetamol 1000mg or ibuprofen 400mg will be given to the woman to start taking before clamping starts. She may repeat 6hrly for three days. Other measures include moving around, verbal support, encouragement, distraction, hot compresses, hot showers, and/or massage. PROTOCOL FOR MISOPROSTOL FOR POSTABORTION CARE (M-PAC) Gestation Dose Route 600 mcg Oral Up to 12 weeks size 400 mcg uterus Timing Three 200 mcg tablets taken at once Sublingual First 200 mcg tablets under tongue for 30 minutes, then swallow the remaining pill. Effects and Side effects of Misoprostol 1. Bleeding lasts longer than in MVA, lasts 2 weeks of which first 3-4 days heavy followed by lighter bleeding and spotting. 2. Cramping starts or increases within few hours of misoprostol administration and is greatest during completion of the abortion. Managed by analgesics. 3. Nausea, vomiting and diarrhea: can occur within the first 4 hours of misoprostol. Reassurance usually enough but if necessary anti-emetic may be given. 4. Fever and chills: misoprostol increases temperature after administration. Paracetamol or ibuprofen will decrease the symptoms. A fever greater than 38C or 100.4F that persists more than 24 hours after administration of misoprostol may indicate possible infection. Warning Signs of Complications – inform woman to seek medical care immediately she notices: Bleeding: soaking more than 2 pads in 1 hr, for longer than 2 days; heavy bleeding that occurs after bleeding had slowed down or stopped; feeling lightheaded or dizzy after many days of bleeding. Requires stabilization, MVA, IV fluids and, if necessary, transfusion. Infection: fever or chills for more than 24 hours after taking misoprostol, severe pelvic or abdominal pain that lasts for a long time, foul smelling or purulent vaginal discharge, marked fundal tenderness. Requires broadspectrum parenteral antibiotic combination e.g. inj penicillin, gentamycin and metronidazole or a cephalosporin and metronidazole. Failure of medication management: Persistent bleeding/cramping not improved by the time of follow up visit. Requires MVA. Follow up visit This is scheduled 2 weeks following misoprostol. Confirm complete expulsion by history, and bimanual examination. Symptoms and signs of completion include: Normal uterine size Absence of uterine tenderness Closed cervical os Woman’s report of the expulsion process Minimal or absent bleeding Resolution of cramping Failure of medication management is indicated by Persistent bleeding/clamping not improved by the time of follow up visit Open cervical os Persistent incomplete abortion should be evacuated by MVA. Make sure the woman had a family planning method, if not counsel and provide a method. Women will be referred for ultrasound only for clear indications such as inability to determine completeness clinically; suspicion of ectopic pregnancy, adnexal masses, uterine masses (e.g. fibroids). SUMMARY OF MISO-PAC PROTOCOL FIRST VISIT (DAY 1) Confirm diagnosis of incomplete abortion and clinical stability Confirm woman is suitable for evacuation with misoprostol Counsel fully and appropriately; Initiate contraception if needed Administer 3 tablets of misoprostol 200mcg (= 600mcg total) orally. Give pain medication at the same time (Brufen or other NSAID).. Observe for 30 min and confirm there is no undue effect Give analgesics to take home Inform who to call or where to go in case of warning signs or complications. Give return date FOLLOW UP VISIT (DAY 7-14) Confirm complete expulsion by history and physical (bimanual) examination Manage persistent incomplete abortion by MVA Treat any complications as appropriate Resolve any doubts with ultrasonography Continue counseling and provide contraception as appropriate Link with other RH and support services REFERENCES 1. Karanja JG: Misoprostol for management of incomplete abortion Kenyan protocol. Unpublished. 2. According to 2005 estimates developed by WHO, UNICEF, UNFPA and World Bank. Available at http://www.unfpa.org/publications/detail.cfm?ID=343. Accessed on October 19, 2007. 3. Tang OS, Gemzell-Danielsson K,Ho PC. Misoprostol :pharmacokinetics profiles, effects on the uterus and side-effects. Int J Gynecol Obstet 2007; 99(Suppl2): S160–7. 4. Blum J., B. Winikoff , K. Gemzell-Danielsson , P.C. Ho ,R.Schiavon, A. Weeks. Treatment of incomplete abortion and miscarriage with misoprostol Int J Gynecol Obstet 2007; 99(Suppl2): S186–189. 5. Bique C, M.Usta, B. Debora, E.Chong, E. Weistheimeranmd B. Winkoff. 2007. Comparison of of misoprostol and manual vacuum aspiration for treatment of incomplete abortion. International Journal of Gynaecology and Obbstetrics. 98(3):222-6. 6. Rizzi R, 2007. Incomplete Abortion. Use of Misoprostol in Obstetrics and Gynaecology, FLASOG. 77-89. 7. Shwekerela B, Kalumuna R, Kipingili N, MashakaN, Westheimer, E. ClarkW, Winikoff B. Misoprostol for treatment of incomplete abortion at the regional hospital level: results fromTanzania. BJOG (Sep2007), (Online Early Articles). doi:10.1111/j.1471- 0528.2007.01469.x. 8. ChungTK, CheungLP, LeungTY, HainesCJ, ChangAM. Misoprostol in the management of spontaneous abortion. BJOG1995;102: 9. DaoB, BlumJ, ThiebaB, RaghavanS, OuedraegoM, LankoandeJ, Winikoff B. Is misoprostol a safe, effective and acceptable alternative to manual vacuum aspiration for postabortion care? Results from a randomized trial inBurkina Faso,WestAfrica.BJOG(Sep2007), (OnlineEarlyArticles). doi:10.1111/j.1471-0528.2007.01468.x 10. Weeks A, Alia G, Blum J, Ekwaru P, Durocher J, Winikoff B, et al.A randomized trial of oral misoprostol versus manual vacuum aspiration for the treatment of incomplete abortion in Kampala, Uganda.Obstet Gynecol 2005;106:540–7. 11. Gynuity Health Projects: Medical Abortion in developing Countries. N.Y.