ketamineMMCJuly12
advertisement

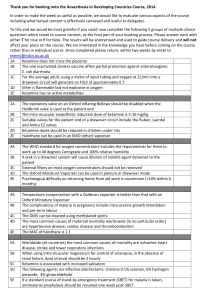
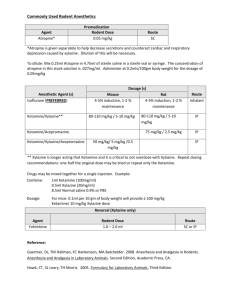
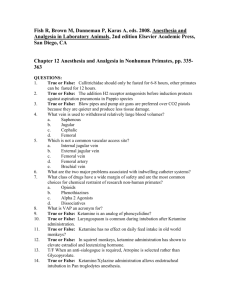
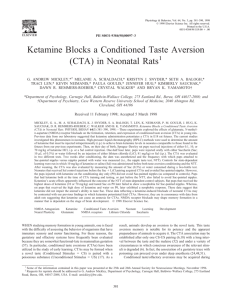
Ketamine as an Adjunct to Pain Management: A Clinical Practice Guideline Location: Adult patients located in PACU, R1 IMC, R1, R3COR, R3, R5, R608, R6, B2, AVU and Gibson Pavilion at Maine Medical Center, Bramhall Campus Prescribers: Patients will be managed by the Anesthesia Pain Management Service. Exception: patients managed by the Palliative Care Service and patients in SCU may be managed per established protocols. Indications: Ketamine has been used at subanesthetic doses (LOW DOSE) as an N-methyl D-aspartate (NMDA) receptor antagonist to block the processing of nociceptive input in chronic pain syndromes. It is effective for the treatment of moderate to severe pain that remains refractory to traditional pain management, including chronic opioid tolerance and opioid-induced hyperalgesia. Ketamine is indicated for chronic pain management and postoperative acute pain management. Infusions may be used in conjunction with opioids and regional analgesia. Pharmacology: Ketamine is a phencyclidine derivative. It is unique among anesthetic agents in that it does not depress respiratory and cardiovascular systems. It is metabolized and conjugated in the liver before being excreted in the urine, with minimally active metabolites. Ketamine is a small lipophilic molecule that distributes very rapidly after vascular uptake, crosses the blood-brain barrier quickly, and is subsequently cleared very quickly, accounting for its rapid onset (30-60 seconds) and relatively short duration of action (about 15 minutes), requiring continuous infusion for maintenance of clinical effects. In subanesthetic doses, the typical anesthetic-dose effects of ketamine, including nystagmus, lacrimation, salivation, tachycardia and spontaneous movements are usually absent, and patients can respond and interact coherently and purposefully. Also, the vivid and often disturbing dreams and hallucinations that follow anesthetic doses of ketamine are avoided. Adverse Reactions: * Hypertension, tachyarrhythmias, tonic/clonic movements, tremor, increased intracranial pressures, hepatotoxicity, emergence reaction/dissociative effects (vivid dreams, hallucinations, delirium, confusion, excitement, or irrational behavior), visual disturbances—diplopia and nystagmus. * Reported adverse effects are based on anesthetic doses of ketamine and occur in less than 10% of patients. Contraindication: History of uncontrolled seizures Uncontrolled intracranial pressure due to brain metastasis or hydrocephalus Severe labile hypertension or poorly controlled cardiac arrhythmia Recent MI, active angina or CHF Known hypersensitivity to ketamine Relative Contraindications Severe hypertension, CHF, COPD associated with hypercarbia Recent CVA History of psychiatric illness Precautions: Current opioid dosing should be reduced by 25%-35% on initiation of ketamine. Potential respiratory depression when other CNS depressants or opioids are administered. Drug Interactions: Thyroid hormones: may increase blood pressure and heart rate. Theophylline: unpredictable extensor-type seizures have been reported. Intravenous Dosing The patient should be provided with ready access, self-administered opiate doses (i.e. PCA bolus) as needed. Patients may also have regional analgesia (i.e. epidural infusions). Dosing of Ketamine o Intravenous subanesthetic (LOW DOSE)* ketamine added as an adjunct to general anesthesia o Initial bolus 0.2-0.5mg/kg intraop at induction o Infusion 0.1mg/kg/hr initiated intraop o Dosing range 0.05-0.2mg/kg/hr Titration and dose modifications must be made by the Anesthesia Pain Management Service, based on analgesic efficacy and patient tolerability. o Increasing by increments of 0.1mg/kg/hr every 6 hours is recommended Ketamine infusions must be administered on an infusion rate controlled pump. * LOW DOSE is defined as less than 0.5mg/kg/hr Supportive Medications Scheduled low-dose benzodiazepines and or haloperidol should be available if needed during the first 24-48 hours on ketamine to prevent or mitigate potential psychomimetic side effects (i.e. lorazepam 0.25-0.5mg PO or IV Q6 hours, may titrate as needed). Anti-cholinergic medications (i.e. glycopyrrolate or scopolamine) should be prescribed as needed to treat or prevent excessive oral secretions. Anesthesia Physician Responsibility The anesthesia physician will remain with the patient for 15 minutes to assess for side effects, vital signs, and analgesic efficacy. Order entry of ketamine in the electronic medical record. RN Responsibility Vital signs, sedation, pain scores, and psychomimetic side effect evaluation every four hours until the ketamine infusion is ceased. Oxygen saturations should be performed at the initiation of ketamine and for changes in dose. Notify APMS for the presence of any of the following signs or symptoms: 1) Systolic blood pressure < 85 2) Heart rate < 60 3) Respiratory rate <10 4) Oxygen saturation <93% (if ordered) 5) Signs of hypertension or blood pressure > 140/90 6) Signs of increased intracranial pressure 7) Presence of tremors, tonic-clonic movements, and/or tics 8) Signs of decreased cough or gag reflex 9) Onset of nausea and/or vomiting 10) Hypersalivation 11) Patient reported diplopia, blurred vision, and/or nystagmus 12) Onset of agitation, fear, hallucinations, nightmares, or vivid dreams 13) Dizziness, lightheadedness, and/or headache 14) Loss of concentration, memory, and/or sense of depression 15) Difficulty sleeping 16) Profound sleepiness or change in level of consciousness 17) Loss of hearing 18) Uncontrolled pain or onset of a significant change in the character of the patient’s reported pain Pharmacy: Ketamine should be mixed in 250ml of sodium chloride 0.9% or dextrose 5% in water to a concentration of 2mg/ml. REFERENCES: Urban MK, Ya Deau JT, Wukovits B, Lipnitsky J. Ketamine as an Adjunct to Postoperative Pain Management in Opioid Tolerant Patients After Spinal Fusions: A Prospective Randomized Trial. Published online: 12/19/2007. Department of Anesthesiology, Hospital for Special Surgery, New York, NY Grande LA, O’Donnell BR, Fitsgibbon DR, Terman GW. Ultra-Low Dose Ketamine and Memantine Treatment for Pain in an Opioid-Tolerant Oncology Patient. Anesthesia & Analgesia 2008; 107:1380-1383 Himmelseher S, Durieux ME. Ketamine for Perioperative Pain Management. Anesthesiology 2005; 102:211-20 Ballantyne JC, Mao J. Opioid Therapy for Chronic Pain. The New England Journal of Medicine 2003:349:1943-53 Hocking G, Cousins MJ. Ketamine in Chronic Pain Management: An Evidence-Based Review. Anesth Analg 2003:97:1730-1739 Ketamine infusion for refractory pain and other symptoms in the inpatient setting. From: City of Hope Policy and Procedure Manual. Original date: 1/2003, Revised 10/2007. Provided by Dr. Neil Slatkin from City of Hope, Duarte, CA. Perry G. Fine. Ketamine: From Anesthesia to Palliative care. Quarterly Newsletter of the American Academy of Hospice and Palliative Medicine. Spring 2003:3. Original Date: 6/2011 Revision Date: 7/2012 Approved by James Pisini, D.O. Approved by Nursing Practice Council: 6/11, 7/12