Debridement of the root canal by instrumentation and irrigation is
advertisement

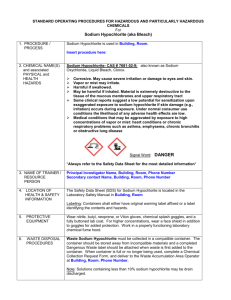
Various Irrigation Solution in Endodontic Complete debridement and disinfection of the pulpal space are considered to be essential for predictable long-term success in endodontic treatment. Residual pulpal tissue, bacteria, and dentine debris may persist in the irregularities of root canal systems, even after meticulous mechanical preparation (Abou-Rass & Piccinino 1982). Therefore, several irrigant solutions have been recommended for use in combination with canal preparation. To date Sodium hypochlorite (NaOCl) is the most commonly used irrigant in endodontic treatment, and has proven to be excellent irrigating solution, due to its tissue dissolving capability and microbial activity. An irrigant serves to flush out debris from within the instrumented root canals, dissolve organic tissue remnants, disinfect the root canal space and provide lubrication during instrumentation, without causing irritation to biological tissues (Cheung & Stock 1993, Ingle et al. 1994). Variables considered during irrigation 1. Canal diameter "Ram pointed out that the irrigational removal of root canal 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. debris seems to be more closely related to canal diameter than to the type of solution used." The viscosity or surface tension of the solution. The diameter and depth of penetration of the irrigating needle. The volume of the solution used. The anatomy of the canal. The method of delivering the irrigant. Contact time with the tissue. Temperature of the irrigant. Ultrasonic activation. The effect of combining different types of solutions. Concentration of irrigant. NaOCl Sodium hypochlorite is one of the most widely used irrigating solutions. Household bleach such as Chlorox contains 5.25% sodium hypochlorite. Some suggest that it be used at that concentration, whereas others suggest diluting it with water, and still others alternate it with other agents, such as ethylenediaminetetraacetic acid with centrimide (EDTAC) or chlorhexidine. Sodium hypochlorite is an effective antimicrobial agent, serves as a lubricant during instrumentation, and dissolves vital and non-vital tissue. Questions concerning the use of sodium hypochlorite are often focused on the appropriate concentration, method of delivery, and concern with cellular damage caused by extrusion into the periradicular tissues. The bactericidal ability of NaOCl results from the formation of hypochlorous acid (HOCl), when in contact with organic debris. HOCl exerts its effects by oxidizing sulphydryl groups within bacterial enzyme systems, thereby disrupting the metabolism of the microorganism (Siqueira et al. 1997), resulting in the killing of the bacterial cells (Baumgartner & Cuenin 1992) NaOCl is used in concentrations varying from 0.5% to 5.25%; it is a potent antimicrobial agent, and effectively dissolves pulpal remnants and organic components of dentine. It is used both as an unbuffered solution at pH 11 in concentration 0.5–5.25%, and buffered with bicarbonate buffer (pH 9.0) usually as a 0.5% solution (Dakin's solution) (Barrette et al. 1989). Contradicting earlier statements, Zehnder et al. ((2002) reported that buffering had little effect on tissue dissolution, and Dakin's solution was equally effective on decayed (necrotic) and fresh tissues. In addition, no differences were recorded for the antibacterial properties of Dakin's solution and an equivalent unbuffered hypochlorite solution. Antibacterial Studies NaOCl is best known for its strong antibacterial activity; it kills bacteria very rapidly even at low concentrations. Waltimo et al. (1999) showed that the resistant microorganism, Candida albicans was killed in vitro in 30 s by both 5% and 0.5% NaOCl. The high susceptibility of C. albicans to NaOCl was recently also verified by Radcliffe et al. (2004). However, Vianna et al. (2004) contrasted these results partly, as 0.5% NaOCl required 30 min to kill C. albicans, whereas 5.25% solution killed all yeast cells in 15 s. Gomes et al. (2001) tested in vitro the effect of various concentrations against E. faecalis. The microbe was killed in less than 30 s by the 5.25% solution, while it took 10 and 30 min for complete killing of the bacteria by 2.5% and 0.5% solutions, respectively. The clearly higher resistance to hypochlorite by E. faecalis as compared with the yeast C. albicans was confirmed by Radcliffe et al. (2004). Recent laboratory experiments using three Gram-negative anaerobic rods typically isolated from primary apical periodontitis, Porphyromonas gingivalis, P. endodontalis, and Prevotella intermedia demonstrated high susceptibility to NaOCl, and all three species were killed within 15 s with all concentrations tested (0.5–5%) (2004). The efficacy of 0.5%, 2.5% and 5.25% sodium hypochlorite (NaOCl) as intracanal irrigants associated with hand and rotary instrumentation techniques against Enterococcus faecalis within root canals and dentinal tubules was investigated (Berber et al. 2006). The results of the present study suggest that 5.25% NaOCl has a greater antibacterial activity inside the dentinal tubules infected with E. faecalis than the other concentrations tested. Under the conditions of this study, irrigants such as NaOCl seem to be able to penetrate well into dentinal tubules. The three main differences between the conditions of in vitro and in vivo studies are the high volume of the medicament available for killing, direct access to all microbes, and absence of other materials in the in vitro experiments that potentially protect bacteria in vivo. In vivo studies have failed to show a better antibacterial effect in the root canal by highly concentrated hypochlorite solutions as compared with low concentrations. Byström & Sundqvist (1983-1985) showed that although 0.5% NaOCl, with or without ethylene-diammine-tetra-acetic acid (EDTA), improved the antibacterial efficiency of preparation compared with saline irrigation, all canals could not be rendered bacteria free even after several appointments. The same authors could not show any significant difference in antibacterial efficiency in vivo between 0.5% and 5% NaOCl solutions. Siqueira et al. (2002) also demonstrated the superior antibacterial affect against root canal bacteria of hypochlorite in comparison with physiological saline. The literature about the antibacterial effect of NaOCl against root canal bacteria describes mostly in vitro studies performed in a test tube, in the root canals of extracted teeth, or in prepared dentine blocks infected with a pure culture of one organism at a time. The in vivo studies, on the other hand, have focused on the elimination of microorganisms from the root canal system in teeth with primary apical periodontitis. However, Peciuliene et al. (2001) studied the effect of instrumentation and NaOCl irrigation in previously root-filled teeth with apical periodontitis. Existing root fillings were removed with endodontic hand instruments and chloroform was not used to avoid a negative effect on microbial viability. After the first microbiological sample, the canal was cleaned and shaped with reamers and Hedström files, using 2.5% NaOCl (10 mL per canal) and 17% buffered EDTA (pH 7, 5 mL) as irrigating solutions. All canals were prepared to size #40 or larger. Chemomechanical instrumentation was completed at the same appointment in all cases. The canals were dried with paper points and a second microbiological sample was taken from all teeth. Bacteria were isolated in 33 of the 40 teeth examined before the instrumentation: E. faecalis was found in 21 teeth (in 11 teeth as a pure culture), yeast C. albicans in six teeth, Gram-negative enteric rods in three teeth, and other microbes in 17 teeth .While no enteric Gram-negative rods or yeasts were found in the second sample after the preparation and irrigation, E. faecalis still persisted in six root canals. Other microbes were found in five canals after preparation. Although not known with certainty, the disappearance of yeasts and the persistence of E. faecalis in the root canals in this study may reflect the results of the above-mentioned in vitro studies (Waltimo et al. (1999), Radcliffe et al. (2004), and Gomes et al. (2001)) which indicated that E. faecalis is much more resistant to killing by NaOCl than C. albicans and Gram-negative rods. NaOCl has been criticized for its unpleasant taste, relative toxicity, and its inability to remove smear layer (Spångberg et al.1973- McComb D 1976). It is also clear that the in vivo effectiveness of NaOCl in the root canal against the infecting microflora is somewhat disappointing in light of the more promising in vitro results, which show killing of practically all microorganisms in a few seconds, when concentrated solutions are used. One natural explanation to poorer in vivo performance is root canal anatomy, in particular, the difficulty in it reaching the most apical region of the canal with large volumes of fresh irrigant. However, it should not be forgotten that the chemical milieu in the canal is quite different from a simplified test tube environment. Marcinkiewicz et al. (2000) showed that nitrite prevented HOCl-mediated bacterial killing. Haapasalo et al. (2000), using dentine powder, showed that the presence of dentine caused marked delays in the killing of the test organism, E. faecalis, by 1% NaOCl. Concentration Pashley et al. (1985) compared the biological effects of mild and strong NaOCl solutions and demonstrated greater cytotoxicity and caustic effects on healthy tissue with 5.25% NaOCl than with 0.5% and 1% solutions. Chang et al. (65) also showed the relationship between the concentration and cytotoxicity of NaOCl. Therefore, it might be recommended to use 0.5–1% NaOCl for canal irrigation instead of the 5.25% solution. However, evidently, more in vivo research on persistent endodontic infections and retreatment is required to obtain a better understanding of the relationship between NaOCl concentration and its antimicrobial activity against specific microorganisms, before final conclusions can be drawn. Baumgartner and Cuenin, in an in vitro study, found that 5.25%, 2.5%, and 1.0% solutions of sodium hypochlorite completely removed pulpal remnants and predentin from un-instrumented surfaces of single-canal premolars.219 Although 0.5% sodium hypochlorite removed most of the pulpal remnants and predentin from uninstrumented surfaces, it left some fibrils on the surface. They commented that “It seemed probable that there would be a greater amount of organic residue present following irrigation of longer, narrower, more convoluted root canals that impede the delivery of the irrigant.” This concern seems reasonable as the ability of an irrigant to be distributed to the apical portion of a canal is dependent on canal anatomy, size of instrumentation, and delivery system. Trepagnier et al. reported that either 5.25% or 2.5% sodium hypochlorite has the same effect when used in the root canal space for a period of 5 minutes.220 Spångberg et al. noted that 5% sodium hypochlorite may be too toxic for routine use.221 They found that 0.5% sodium hypochlorite solution dissolves necrotic but not vital tissue and has considerably less toxicity for HeLa cells than a 5% solution. They suggested that 0.5% sodium hypochlorite be used in endodontic therapy. Bystrom and Sundquist examined the bacteriologic effect of 0.5% sodium hypochlorite solution in endodontic therapy.222 In that in vivo study, using 0.5% sodium hypochlorite, no bacteria could be recovered from 12 of 15 root canals at the fifth appointment. This was compared with 8 of 15 root canals when saline solution was used as the irrigant. Baumgartner and Cuenin also commented that “The effectiveness of low concentrations of NaOCl may be improved by using larger volumes of irrigant or by the presence of replenished irrigant in the canals for longer periods of time.”219 On the other hand, a higher concentration of sodium hypochlorite might be equally effective in shorter periods of time. Siqueira et al., in an in vitro study, evaluated the effect of endodontic irrigants against four blackpigmented gram-negative anaerobes and four facultative anaerobic bacteria by means of an agar diffusion test. A 4% sodium hypochlorite solution provided the largest average zone of bacterial inhibition and was significantly superior when compared with the other solutions, except 2.5% sodium hypochlorite (p < .05). Based on the averages of the diameters of the zones of bacterial growth inhibition, the antibacterial effects of the solution were ranked from strongest to weakest as follows: 4% sodium hypochlorite; 2.5% sodium hypochlorite; 2% chlorhexidine, 0.2% chlorhexidine EDTA, and citric acid; and 0.5% sodium hypochlorite.223 The question of whether sodium hypochlorite is equally effective in dissolving vital, nonvital, or fixed tissue is important since all three types of tissue may be encountered in the root canal system. Rosenfeld et al. demonstrated that 5.25% sodium hypochlorite dissolves vital tissue.224 In addition, as a necrotic tissue solvent, 5.25% sodium hypochlorite was found to be significantly better than 2.6%, 1%, or 0.5%.225 In another study, 3% sodium hypochlorite was found to be optimal for dissolving tissue fixed with parachlorophenol or formaldehyde.226 Clearly, the final word has not been written on this subject. Sodium Hypochlorite Used in Combination with Other Medicaments. Whether sodium hypochlorite should be used alone or in combination with other agents is also a source of controversy. There is increasing evidence that the efficacy of sodium hypochlorite, as an antibacterial agent, is increased when it is used in combination with other solutions, such as calcium hydroxide, EDTAC, or chlorhexidine. Hasselgren et al .found that pretreatment of tissue with calcium hydroxide can enhance the tissue-dissolving effect of sodium hypochlorite.227 Wadachi et al., using 38 bovine freshly extracted teeth, studied the effect of calcium hydroxide on the dissolution of soft tissue on the root canal wall.228 They found that the combination of calcium hydroxide and sodium hypochlorite was more effective than using either medicament alone .However, Yang et al., using 81 freshly extracted human molars, examined the cleanliness of main canals and inaccessible areas (isthmi and fins) at the apical, middle, and coronal thirds.229 Complete chemomechanical instrumentation combined with 2.5% sodium hypochlorite irrigation alone accounted for the removal of most tissue remnants in the main canal. Prolonged contact with calcium hydroxide to aid in dissolving main canal tissue remnants after complete instrumentation was ineffective. They also found that tissues in inaccessible areas (isthmi and fins) of root canals were not contacted by calcium hydroxide or sodium hypochlorite and were poorly débrided. As they noted, however, it could be that their study did not permit sufficient time (1 day or 7 days) for the tissue to be degraded. Hasselgren et al. reported that porcine muscle was completely dissolved after 12 days of exposure to calcium hydroxide.227 Byström and Sundqvist found 5.0% and 0.5% sodium hypochlorite equally effective. By combining 5.0% sodium hypochlorite with EDTA, however, the bactericidal effect was considerably enhanced. This could be related to the removal of the contaminated smear layer by EDTA.235 Fischer and Huerta believe that it is the alkaline property (pH 11.0 to 11.5) of sodium hypochlorite that makes it effective against anaerobic microbes,236 and a US Army group found full-strength sodium hypochlorite to be effective in 5 minutes against obligate anaerobes.237 Possibly, the bactericidal effect gained by combining sodium hypochlorite with other chemicals comes from the release of chlorine gas. This was especially true of citric acid and to some extent with EDTA, but not with peroxide.238 Temerature .Other variables to be considered include temperature as well as shelf life of the solution.230–232 Raphael et al. tested 5.25% sodium hypochlorite on Streptococcus faecalis,Staphylococcus aureus, and Pseudomonas aeruginosa at 21°C and 37°C and found that increasing the temperature made no difference on antimicrobial efficacy and may even have decreased it.233 Pseudomonas aeruginosa was particularly difficult to eliminate. Buttler and Crawford, using Escherichia coli and Salmonella typhosa, studied 0.58%, 2.7%, and 5.20% sodium hypochlorite for its ability to detoxify endotoxin.234 All three concentrations were equally effective; however, large amounts of E. coli endotoxin could not be detoxi-fied by 1 mL of 0.58% or 2.7% sodium hypochlorite.How this relates to the clinical situation is uncertain.Against most anaerobic bacteria, Chlorhexidine (CHX) While NaOCl kills bacteria quite effectively, it is caustic if accidentally expressed into the periapical area or adjacent structures such as the maxillary sinus (66). In addition, the active chlorine in the solution may damage patients' clothing through its strong bleaching effect. Therefore, there has been an ongoing search for alternative irrigating solutions that could replace NaOCl. CHX is probably the most widely used biocide in antiseptic products in general. It is able to permeate the cell wall or outer membrane and attacks the bacterial cytoplasmic or inner membrane or the yeast plasma membrane. High concentrations of CHX cause coagulation of intracellular constituents (49). CHX gluconate has been in use for a long time in dentistry because of its antimicrobial properties, its substantivity, and its relatively low toxicity. Despite the advantages of CHX, its activity is pH dependent and is greatly reduced in the presence of organic matter (67). It has a wide antimicrobial spectrum and is effective against both Gram-positive and Gram-negative bacteria as well as yeasts, while mycobacteria and bacterial spores are resistant to CHX (68, 69). CHX is not considered to be an effective antiviral agent, and its activity is limited to lipid-enveloped viruses (70). In direct contact with human cells, CHX is cytotoxic; a comparative study using fluorescence assay on human PDL cells showed corresponding cytotoxicity with 0.4% NaOCl and 0.1% CHX (65). Its potential and use in endodontics have been under active research over the last few years. Although studies comparing the antibacterial effect of NaOCl and CHX have produced somewhat conflicting results, it seems that when used in identical concentrations, their antibacterial effect in the root canal and in infected dentine is similar (71–73). However, an in vitro study by Gomes et al. (56) demonstrated marked differences in the killing of enterococci by CHX and NaOCl. Only the highest concentration of 5.25% of NaOCl killed E. faecalis rapidly in 30 s, while with a lower concentration, (4–0.5%) 5–30 min were required for complete killing to occur. CHX digluconate, on the other hand, killed E. faecalis cells in 30 s or less in concentrations of 0.2–2%. The result was later supported by Oncag et al. (74) and Vianna et al. (55), who also showed in vitro CHX to be superior to NaOCl in killing of E. faecalis and Staphylococcus aureus. The same study revealed that CHX in a gel form required a much longer time to kill E. faecalis than the corresponding concentration in a liquid. Waltimo et al. (53) studied the antifungal effect of combinations of endodontic irrigants including CHX. CHX effectively killed C. albicans, which is in accordance with previous studies that have shown that CHX is an effective antifungal agent in vitro (75–77). Waltimo et al. (53) also found that the combinations of disinfectants were equally or less effective than the more effective component when used alone. Heling & Chandler (71) studied the antimicrobial effect of irrigant combinations within dentinal tubules in vitro against E. faecalis and found that a specific combination of 3% hydrogen peroxide (H2O2) and CHX was superior in its antibacterial activity in dentine compared with other regimens such as CHX alone and NaOCl. These studies were continued in a series of in vitro experiments by Steinberg et al. (78), who challenged E. faecalis suspensions in trypticase soy broth (a culture medium rich in peptides) with various combinations of CHX and H2O2. The experiments demonstrated that the combination of the two substances totally killed E. faecalis in concentrations much lower than each component alone. According to that study, the bactericidal effect of CHX derives from its ability to denaturate the bacterial cell wall while forming pores in the membrane, while H2O2 is effective against intracellular organelles such as DNA. Although the exact synergistic mechanism of CHX and H2O2 is not known, it can be postulated that the exposure of bacteria to CHX leads to a more permeable cell wall that H2O2 can penetrate easily and hence damage the intracellular organelles (78). Corresponding synergistic effects were not detected between H2O2 and NaOCl in the dentine block model (71). Dona et al. (79) showed that the combination of CHX and H2O2 was a more effective antiplaque mouth rinse than either component alone. There are no reports of clinical studies where the combinations of CHX and H2O2 have been used to disinfect the root canal system in cases of primary apical periodontitis or persistent endodontic infections. However, cytotoxicity of the medicament combinations should first be investigated. Interestingly, combinations of CHX and carbamide peroxide have been shown to be additive in their cytotoxicity (80). A potential weakness of CHX in the root canal may be its susceptibility to the presence of organic matter (67). In an in vitro study, Haapasalo et al. (63) showed that the effect of CHX is reduced, although not prevented, by the presence of dentine. Portenier et al. (81) demonstrated total loss of activity of CHX by bovine serum albumin. This might indicate the possibility that inflammatory exudate, rich in proteins such as albumin, entering the root canal through the apical foramen, may weaken the antibacterial effect of CHX. In a separate study, Portenier et al. (82) showed further that CHX was strongly inhibited by dentine matrix (the organic component of dentine) as well as heat-killed cells of E. faecalis and C. albicans. It is quite possible that inhibitions like the ones described in these studies can partly explain the poorer in vivo performance of CHX in the root canal as compared with killing experiments in vitro in a test tube environment. CHX lacks the tissue-dissolving ability, which is one of the obvious benefits of NaOCl. While the in vitro studies have demonstrated the antibacterial effect of CHX against E. faecalis to be superior to that of NaOCl, there are no in vivo studies yet available that would confirm the better activity of CHX against this resistant species also in the infected root canal. Nevertheless, there is no doubt that CHX gluconate, in concentrations between 0.2% and 2%, offers a good alternative for root canal irrigation with potent antimicrobial activity. Future studies of CHX combinations are needed to establish whether these could give additional advantage in the fight against resistant root canal microbes. Kuruvilla and Kamath combined the solutions within the root canal, the antibacterial action was suggestive of being augmented.245 The results of their study indicate that the alternate use of sodium hypochlorite and chlorhexidine gluconate irrigants resulted in a greater reduction of microbial flora (84.6%) when compared with the individual use of sodium hypochlorite (59.4%) orchlorhexidine gluconate (70%) alone.245 White et al. found that chlorhexidine instills effective antimicrobial activity for many hours after instrumentation. 246 Although sodium hypochlorite is equally effective on initial exposure, it is not a substantive antimicrobial agent EDTA and citric acid EDTA (17%, disodium salt, pH 7) has little if any antibacterial activity. On direct exposure for extended time, EDTA extracts bacterial surface proteins by combining with metal ions from the cell envelope, which can eventually lead to bacterial death. EDTA is an effective chelating agent, which is widely used in endodontic preparation (88). It effectively removes smear layer by chelating the inorganic component of the dentine. Therefore, by facilitating cleaning and removal of infected tissue, EDTA contributes to the elimination of bacteria in the root canal. It has also been shown that removal of the smear layer by EDTA (or citric acid) improves the antibacterial effect of locally used disinfecting agents in deeper layers of dentine (30, 89). Niu et al. (90) studied the ultrastructure on canal walls after EDTA and combined EDTA plus NaOCl irrigation by scanning electron microscopy: more debris was removed by irrigation with EDTA followed by NaOCl than with EDTA alone. In addition to EDTA, citric acid can also be used for irrigation of the root canal to remove the smear layer (88, 91, 92). Concentrations ranging from 1% to 50% have been used (91). Gutmann et al. (93) showed that 10% citric acid was more effective in removing the smear layer from apical root-end cavities than ultrasound. Yamaguchi et al. (94) compared the chelating and antibacterial properties of citric acid and EDTA. Powdered dentine–resin mixture was found to be more soluble in a 0.5, 1, and 2 M citric acid solutions than in a 0.5 M EDTA solution. Citric acid solution showed antibacterial effects on all 12 root canal bacteria tested. However, Liolios et al. (95) reported better removal of smear layer by commercial EDTA preparations than with 50% citric acid. Di Lenarda et al. (96) and Scelza et al. (97) reported a minor or no difference in smear layer removal with citric acid and 15% EDTA. In a recent study, Machado-Silveiro et al (98) measured the demineralization capability of 1% and 10% citric acid, 10% sodium citrate, and 17% EDTA during immersions of 5, 10, and 15 min on root canal dentine. Ten percent citric acid was more effective than 1% citric acid, which was more effective than EDTA. Takeda et al. (99) studied the effects of three endodontic irrigants and two types of laser on a smear layer created by hand instrumentation ex vivo in the middle and apical thirds of root canals. Irrigation with 17% EDTA, 6% phosphoric acid and 6% citric acid did not remove the entire smear layer from the root canal system. In addition, these acidic solutions demineralized the intertubular dentine around tubular openings, which became enlarged. The CO2 laser was useful in removing and melting the smear layer on the instrumented root canal walls, and the Er : YAG laser was the most effective in removing the smear layer from the root canal wall. Removal of the smear layer is an important step to facilitate disinfection of the root canal. Both EDTA and citric acid can effectively remove the smear layer created during canal instrumentation. Although citric acid may also have an antibacterial effect, this has not been compared with other root canal disinfecting agents in in vitro or in vivo studies. H2O2 H2O2 is a widely used biocide for disinfection and sterilization (49). It is a clear, colorless liquid that is used in a variety of concentrations in dentistry, ranging from 1% to 30%. H2O2 is environmentally non-problematic, as it degrades into water and oxygen. H2O2 solutions are quite stable, but they may contain stabilizers to prevent decomposition. H2O2 is active against viruses, bacteria, yeasts, and even bacterial spores (100). It has greater activity against Gram-positive than Gram-negative bacteria. Production of catalase or superoxide dismutase by several bacteria can afford those species some protection against H2O2. H2O2 produces hydroxyl free radicals (•OH), which attack several cell components such as proteins and DNA (49). In endodontics, H2O2 has long been used because of its antimicrobial and cleansing properties. Möller (85) recommended 30% H2O2 as the first step (after mechanical cleaning) in tooth surface disinfection. Potent H2O2 solution will affect the organic matter on the tooth in such a way that the disinfectants, such as iodine, will more effectively kill the microbes. It has been particularly popular in cleaning the pulp chamber from blood and tissue remnants, but it has also been used in canal irrigation. However, there are much less research reports about the effectiveness of H2O2 in the root canal than of other disinfectants. Siqueira et al. (101) showed that a combination of NaOCl and H2O2 was no more effective against E. faecalis in contaminated root canals ex vivo than NaOCl alone. Heling & Chandler (71) compared the antibacterial effect of CHX and H2O2 in various concentrations against E. faecalis-infected dentine. CHX proved to be superior in its antibacterial effect; however, a combination of the two medicaments at low concentration was far more antibacterial than any other tested medicament alone. A similar synergistic effect was not measured with a combination of H2O2 and NaOCl (71). The synergism between H2O2 and CHX was subsequently verified by Steinberg et al. (78). In a recent study by Möller et al. (102) in monkey teeth, 10% H2O2 was used as part of the irrigating protocol. A total of 186 root canals in 176 teeth were inoculated with preselected combinations of bacteria for several months: group 1, anaerobes and streptococci; group 2, E. faecalis+group 1. The first bacteriological sample was taken before preparation taking great care to avoid contamination. The root canals were treated according to a standardized protocol: mechanical instrumentation by hand files to size #40–#60, with irrigation with buffered 1% NaOCl solution, followed by 10% H2O2. The procedure was completed by rinsing with NaOCl solution. This solution was subsequently inactivated with 5% sodium thiosulpfate solution in the root canal. A second bacteriological sample was then taken. In group 1 (160 canals), bacteria were found in 98% and 68% of the canals in samples 1 and 2, respectively. In group two (24 canals), the corresponding frequencies were 100% and 88%. Although the bacterial counts were greatly reduced, it is correct to conclude that the protocol used could not predictably produce sterile root canals in monkey teeth (102). Although H2O2 has long been used in disinfection and canal irrigation in endodontics, the available literature does not support its use over that of other irrigating solutions. However, it has a role in tooth surface disinfection, and the potential usefulness of the synergistic effect with CHX has not yet been fully evaluated. MTAD MTAD (a mixture of tetracycline isomer, acid, and detergent, Biopure, Tulsa Dentsply, Tulsa OK, USA) is a new product in the quest for a better root canal irrigant, with a pH as low as 2.15 (103, 104). Although many of the existing root canal-irrigating solutions have a number of positive effects in the canal, all of them also have weaknesses. Therefore, in order to maximize the benefits of irrigation, several different solutions must be used during the preparation, in varying volumes and time. In addition, although poorly studied, there is a general uncertainty about the efficiency of irrigation in the narrow, most apical part of the canal. MTAD consists of doxycycline, citric acid, and the detergent Tween-80 (103). In that study with this new irrigant, focusing on the removal of smear layer, 48 extracted single-rooted teeth were prepared by using passive stepback and rotary 0.04 taper NiTi files. Distilled water or 5.25% NaOCl was used for irrigation followed by a 5 mL irrigation with one of the following: sterile distilled water, 5.25% NaOCl, 17% EDTA, or MTAD. The effect on the smear layer and the amount of erosion on the root canal walls at the coronal, middle, and apical portion were examined using a scanning electron microscope. The results indicated that MTAD is an effective solution for the removal of the smear layer and does not significantly change the structure of the dentinal tubules, when canals are first irrigated with NaOCl, followed by a final rinse of MTAD (103). EDTA caused more erosion of dentine in the coronal and middle parts of the canal than MTAD. In the apical third, canals irrigated with MTAD (final irrigation) were cleaner, as judged from scanning electron micrographs, compared with final irrigation with EDTA (103). In another study, the same group investigated the effect of various concentrations of sodium NaOCl as an intracanal irrigant before irrigation with MTAD as a final rinse on the smear layer. The results showed that MTAD removed most of the smear layer when used alone; however, remnants of the organic component of the smear layer could be detected on the root canal walls. There were no significant differences between the ability of 1.3%, 2.6%, and 5.25% NaOCl as root canal irrigants and MTAD as a final rinse to remove the smear layer. All combinations removed both the smear layer as well as the organic remnants. Therefore, it seems to be reasonable to use 1.3% NaOCl during instrumentation, followed by MTAD to remove the smear layer (104). Beltz et al. (105) compared the tissue-solubilizing action of MTAD, NaOCl, and EDTA. MTAD solubilized dentine well, whereas organic pulp tissue was clearly more unaffected by it. Zhang et al. (106) evaluated the cytotoxicity of MTAD on fibroblasts by comparing the 50% inhibitory dose with other irrigating regimens. The results showed that MTAD is less cytotoxic than eugenol, 3% H2O2, Ca(OH)2 paste, 5.25% NaOCl, Peridex (a CHX mouth rinse with additives), and EDTA, but more cytotoxic than 2.63%, 1.31%, and 0.66% NaOCl (106). One of the key points of interest with MTAD is its antibacterial activity, as it contains tetracycline, detergent, and has a low pH (103, 104). In an in vitro study, the antibacterial effects of MTAD, NaOCl, and EDTA were compared using a diskdiffusion test on agar plates. The results showed that even highly diluted MTAD produced clear zones of inhibition of the test bacterium, E. faecalis (107). However, it is important to bear in mind that the agar diffusion test only shows inhibition of growth, which may not be the same as bacterial killing. With regard to the high concentration of tetracycline in MTAD, the result is as expected with the agar diffusion test. Shabahang et al. (108) and Shabahang & Torabinejad (109) investigated the effect of MTAD on root canals contaminated with either whole saliva or E. faecalis of extracted human teeth and reported good antibacterial activity. BDA Kaufman reported the success of several cases using bis-dequalinium acetate (BDA) as a disinfectant and chemotherapeutic agent247 He cited its low toxicity, lubrication action, disinfecting ability, and low surface tension, as well as its chelating properties and low incidence of post-treatment pain. Others have pointed out the efficacy of BDA. In one report, it was rated superior to sodium hypochlorite in débriding the apical third.248 When marketed as Solvidont (Dentsply/DeTrey, Switzerland), the University of Malaysia reported a remarkable decrease in postoperative pain and swelling when BDA was used. They attributed these results to the chelation properties of BDA in removing the smear layer coated with bacteria and contaminants as well as the surfactant properties that allow BDA “to penetrate into areas inaccessible to instruments.”249 Bisdequalinium acetate is recommended as an excellent substitute for sodium hypochlorite in those patients who are allergic to the latter.Outside North America, it enjoys widespread use. A Loyola University in vitro study reported that fullstrength Clorox (sodium hypochlorite) and Gly-Oxide (urea peroxide), used alternately, were 100% effective against Bacteroides melaninogenicus, which has been implicated as an endodontic pathogen. Alternating solutions of sodium hypochlorite and hydrogen peroxide bcause a foaming action in the canal through the release of nascent oxygen. Hydrogen peroxide (3%) alone also effectively “bubbles” out debris and mildly disinfects the canal. In contrast, Harrison et al. have shown that using equal amounts of 3% hydrogen peroxide and 5.25% sodium hypochlorite inhibited the antibacterial action of the irrigants.250 Because of the potential for gaseous pressure from residual hydrogen peroxide, it must always be neutralized by the sodium hypochlorite and not sealed in the canal. It must be understood that each of the studies cited above has examined limited test results concerning the use of various irrigants or combinations of irrigants. However, there are other factors aside from the solution used. For example, Ram pointed out that the irrigational removal of root canal debris seems to be more closely related to canal diameter than to the type of solution used.251 This, in turn, must be related to the viscosity or surface tension of the solution, the diameter and depth of penetration of the irrigating needle,the volume of the solution used, and the anatomy of the canal. Ultrasonic Irrigation. An irrigant serves to flush out debris from within the instrumented root canals, dissolve organic tissue remnants, disinfect the root canal space and provide lubrication during instrumentation, without causing irritation to biological tissues (Cheung & Stock 1993, Ingle et al. 1994). The flushing action of the irrigant solution may be more important during the cleaning process than the ability of the irrigant solution to dissolve tissue (Baker et al. 1975). Most of the dentine debris is inorganic matter that cannot be dissolved by NaOCl. Therefore, removal of dentine debris relies mostly on the flushing action of irrigant. The enhancement of the flushing action of an irrigant solution by using ultrasound is well documented (Cunningham & Martin 1982, Cunningham et al. 1982a,b, Stock 1991, Lumley et al. 1993, Lee et al. 2004a,b). The ultrasound device is designed to allow endodontic irrigant to pass along the ultrasonic files. The irrigant is activated by the ultrasonic energy imparted from the energized instruments producing acoustic streaming and eddies (Ahmad et al. 1987, Krell & Johnson 1988, Stock 1991). Cunningham & Martin (1982) and Cunningham et al. (1982a,b) reported that more bacterial spores and dentine debris were removed during ultrasonic irrigation than hand irrigation. Previous studies showed that both mechanical and chemical action of the irrigant were dependent upon the efficiency of the delivery system (Abou-Rass M, Oglesby SW 1981), the tissue surface area in contact with the irrigant solution ( Baker et al. 1975, Moored WR, Wesselink PR 1982,Gomes et al. 2001, Radcliffe et al. 2004, Vianna et al. 2004,), the frequency of changing the solution (Moorer WR, Wesselink PR 1982) and the total volume of the irrigant (Cunningham et al.1982,siqueira at al.2000, Sedgley et al.2005). However, few studies have evaluated these aspects in the presence of ultrasonic activiation and rotary instrumentation. As stated previously, the use of ultrasonic or sonic irrigation to better cleanse root canals of their filings, debris, and bacteria, all the way to the apex, has been well documented by Cunningham et al.168,169 as well as others. More recently, they have been joined by a number of clinicians reporting favorable results with ultrasonic/sonic irrigation, from thoroughly cleansing the walls in necrotic open apex cases, 252 to removing the smear layer.253 Griffiths and Stock preferred half-strength sodium hypochlorite to Solvidont in débriding canals with ultrasound.254 Sjögren and Sundqvist found that ultrasonography was best in eliminating canal bacteria but still recommended the “use of an antibacterial dressing between appointments.255 Others were not as impressed.256,257 In fact, one group found sodium hypochlorite somewhat better than tap water when used with ultrasonography but also noted that both irrigants were ineffective “in removing soft tissue from the main canal, the isthmus between canals, the canal fins, and the multiple branches or deltas.”252 However, they used ultrasonics for only 3 minutes with a No. 15 file and 1 minute with a No. 25 diamond file.252 As Druttman and Stock pointed out, “with the ultrasonic method, results depended on irrigation time.”258 As previously noted, the cleanest canals are achieved by irrigating with ultrasonics and sodium hypochlorite for 3 minutes after the canal has been totally prepared (Figure 10- 38). Moreover, ultrasonics proved superior to syringe irrigation alone when the canal narrowed to 0.3 mm (size 30 instrument) or less.259 Buchanan noted that it is the irrigants alone that clean out the accessory canal. Instruments cannot reach back into these passages. Only the copious use of a tissue-dissolving irrigant left in place for 5 to 10 minutes repeatedly will ensure auxiliary canal cleaning.260 Figure 10-38 Irrigating solution climbs the shaft of a CaviEndo vibrating No. 15 file to agitate and débride unreachable spaces in the canal. (Courtesy of Dentsply/Cavitron.) Method of Use Although the technique for irrigation is simple, the potential for serious complications exists. Regardless of the delivery system, the solution must be introduced slowly and the needle never wedged in the canal. The greatest danger exists from forcing the irrigant and canal debris into the periradicular tissue owing to a piston-like effect. Several types of plastic disposable syringes are available. Usually, the irrigating solution is kept in a dappen dish that is kept filled. The syringe is filled by immersing the hub into the solution while withdrawing the plunger. The needle, or probe in the case of the ProRinse (Dentsply/Tulsa Dental; Tulsa, Okla.), is then attached. Care must be taken with irrigants like sodium hypochlorite to prevent accidents. Sodium hypochlorite can be irritating to the eyes, skin, and mucous membranes. Some practioners provide protective glasses to their patients to protect their eyes. Also, it can ruin clothing. The irrigating needle may be one of several types. It should be bent to allow easier delivery of the solution and to prevent deep penetration of the needle or probe (see Figure 10-38). A commonly used needle is the 27- gauge needle with a notched tip, allowing for solution flowback (see Figure 10-39, insert), or the blunt-end ProRinse. It is strongly recommended that the needle lie passively in the canal and not engage the walls. Severe complications have been reported from forcing irrigating solutions beyond the apex by wedging the needle in the canal and not allowing an adequate backflow.261 This is an important point in view of results suggesting that the proximity of the irrigation needle to the apex plays an important role in removing root canal debris.262 Moser and Heuer reported Monoject endodontic needles (Tyco/Kendall;Mansfield,Mass.) to be the most efficient delivery system in which longer needles of a blunted, open-end system were inserted to the full length of the canal.263 The point is that a larger volume of solution can be delivered by this method. However, the closer the needle tip is placed to the apex, the greater the potential for damage to the periradicular tissues. Druttman and Stock found much the same results, that with “conventional methods, irrigation performance varied with the size of the needle and volume of irrigant.”258 Walton and Torabinejad stated that “Perhaps the most important factor is the delivery system and not the irrigating solution per se.” ..266,267 Furthermore, it was found that the volume of the irrigant is more important than the concentration or type of irrigant.264 Chow found that there was little flushing beyond the depth of the needle, unless the needle was “bound” in the canal and the irrigant forcibly expressed.265Wedging a needle in a canal is dangerous and can cause serious sequelae. It is reported that “In order to be effective, the needle delivering the solution must come in close proximity to the material to be removed.”262 Small diameter needles were found to be more effective in reaching adequate depth but were more prone to problems of possible breakage and difficulty in expressing the irrigant from the narrow needles.262 Of course, the closer the needle is to the apical foramen, the more likely it is that solution will be extended into the periradicular tissues. Kahn, Rosenberg et al. at New York University, in an in vitro study, tested various methods of irrigating the canal. Evaluated were Becton-Dickinson (BD), (Franklin Lake, N.J.) 22-gauge needles;Monoject endodontic needles, 23 and 27 gauge (Tyco/Kendall, Mansfield, Mass.) (Figure 10-39); ProRinse 25-, 28-, and 30-gauge probes (Dentsply/Tulsa Dental; Tulsa, Okla); CaviEndo ultra- sonic handpiece (Dentsply/Caulk, York, Pa.); and the MicroMega 1500; Woodside, N.Y.) Figure 10-39 Simplest endodontic irrigating system—plastic disposable syringe and needle. Note that the needle is loose in the canal to allow backflow. Notched needle tip (inset) eliminates pressure (Monoject). Canals in plastic blocks were filled with food dye and instrumented to progressively larger sizes. ProRinse probes were highly effective in all gauges and in all sizes of canals tested. In canals instrumented to size 30 K file and size 35 K file, the smaller-lumen 27gauge notch-tip needle was found to be highly effective. The larger 23-gauge notchtip needle was found to be relatively ineffective, as was the standard 22-gauge beveled needle. The Micromega 1500 and CaviEndo systems were highly effective at the size 20, 25, and 30 K-file levels. Recapitulation, with smaller-sized vibrating files, completely cleared dye from the few apical millimeters. The zones of clearance beyond the tip of the ProRinse probes were significant in that they indicated that highly effective canal clearance occurred without having to place the tip of the probes at the apical foramina. The effectiveness of the ProRinse seemed related to its design. It has a blunt tip, with the lumen 2 mm from the tip. Expression of fluid through the lumen creates turbulence around and beyond the end of the probe (Figure 10-40).This model system was created to enable the investigators, using a Sony camcorder, to observe the differences of different irrigating systems. However, there are inherent differences in the in vitro test model from the in vivo situation. In vivo variables that affect delivery of the irrigant are canal length and quality of instrumentation. In vitro results, although potentially valuable, cannot be directly extrapolated to the in vivosituation. Removal of the Smear Layer Organic Acid Irrigants. The use of organic acids to irrigate and débride root canals is as old as root canal therapy itself. More recently, though, it has been investigated by Tidmarsh, who felt that 50% citric acid gave the cleanest dentin walls without a smear layer268 (Figure 10-41). Wayman et al. also reported excellent filling results after preparation with citric acid (20%), followed by 2.6% sodium hypochlorite and a final flushing with 10% citric acid.269 In two separate studies, the US Army reported essentially the same results. Both studies, however, emphasized the importance of recapitulation—re-instrumentation with a smaller instrument following each irrigation. 270,271 Not to be outdone, the US Air Force tested both citric acid and sodium hypochlorite against anaerobic bacteria. They reported them equally effective as a bactericide in 5 to 15 minutes.272 Figure 10-40 ProRinse needles irrigate through a side vent. A, Douching spray reaches all regions of the canal by rotating the needle.B, Closed-end needle eliminates possibilities of puncture of the apical foramen or a “water cannon” effect from openend needles (Courtesy of Dentsply/Tulsa Dental.) Figure 10-41 A, Canal wall untreated by acid. Note granular material and obstructed tubuli. B,Midroot canal wall treated with citric acid.The surface is generally free of debris. C, Midroot canal wall cleaned with phosphoric acid, showing an exceptionally clean regular surface.D, Apical area of root canal etched by phosphoric acid, revealing lateral canals. Reproduced with permission from Tidmarsh BG.268 Other organic acids have been used to remove the smear layer: polyacrylic acid as Durelon and Fuju II liquids, both 40% polyacrylic acid.273 Chelating Agents. The most common chelating solutions used for irrigation include Tublicid, EDTA, EDTAC, File-Eze, and RC Prep, in all of which EDTA is the active ingredient.Nygaard-Østby first suggested the use of EDTA for cleaning and widening canals.274 Later, Fehr and Nygaard-Østby introduced EDTAC (N-O 504 endodontics Therapeutics Hd, Sweden), quaternary ammonium bromide, used to reduce surface tension and increase penetration.275 The optimal pH for the demineralizing efficacy of EDTA on dentin was shown by Valdrighi to be between 5.0 and 6.0.276 Goldberg and Abramovich have shown that EDTAC increases permeability into dentinal tubules, accessory canals, and apical foramina277 (Figure 10-42). McComb and Smith found that EDTA (in its commer- cial form, REDTA), when sealed in the canal for 24 hours, produced the cleanest dentinal walls.278 Goldman and colleagues have shown that the smear layer is not removed by sodium hypochlorite irrigation alone but is removed with the combined use of REDTA.279. This study helps answer the question of the composition of the smear layer since chelating agents remove only calcified tissue, whereas sodium hypochlorite removes organic material. Goldberg and Spielberg have shown that the optimal working time of EDTA is 15 minutes, after which time no more chelating action can be expected.280 This study indicates that EDTA solutions should perhaps be renewed in the canal each 15 minutes. Since Goldman et al.’s landmark research in 1981, reporting the efficacy of EDTA and sodium hypochlorite to remove the smear layer, a host of confirming reports have been published.281–289. The US Army Institute of Dental Research, after first reporting the constituents, the thickness, and the layering of the smear layer,281 followed up with two reports detailing the importance of alternate use of 15% EDTA and 5.25% sodium hypochlorite.282–287 They introduced a total of 33 mL of irrigants into each canal, using 27 g blunt Monoject endodontic needles. The original Nygaard-Østby formula for 15% EDTA was used: disodium salt of EDTA, 17 g; distilled water, 100 mL; and 5 N sodium hydroxide, 9.25 mL.287 Developed by Stewart and others in 1969,290 RC-Prep is composed of EDTA and urea peroxide in a base of Carbowax. It is not water soluble. Its popularity in combination with sodium hypochlorite, is enhanced by the interaction of the urea peroxide in RC-Prep with sodium hypochlorite, producing a bubbling action thought to loosen and help float out dentinal debris.291 Zubriggen et al., however, reported that a residue of RC-Prep remains in the canals in spite of further irrigation and cleansing.292. This led to the question of the effect of RC-Prep residue on apical seal. Cooke et al. showed that RC-Prep allowed maximum leakage into filled canals—over 2.6 times the leakage of the controls.293 Figure 10-42 A, Coronal portion of canal of in vivo endodontically treated tooth with EDTAC. The tubules are open, and the canal is clean and free of smear. B, Filed canal treated with EDTAC.Longitudinal section of dentinal tubules shows thin intertubular matrix. A reproduced with permission from Kaufman AY et al.239 B reproduced with ermission from Goldberg F and Abramovich A.277 Although the presence of an irrigant in the canal throughout instrumentation facilitates the procedure, there are specific lubricating agents designed for that purpose: examples are RC Prep (Premier Dental; King of Prussia, Pa.), GlyOxide (Smith Kline Beecham, Pittsburgh, Pa.), REDTAC (Roth International, Chicago, Ill.), and Glyde File Prep (Dentsply/Maillefer; Tulsa, Okla.). It is highly recommended that canals always be instrumented while containing an irrigant and/or a lubricating agent. Instrumentation in this manner may prevent the complication of losing contact with the measurement control owing to an accumulation of debris in the apical segment of the canal.