INFORMATION SECRUITY AND CONFIDENTIALITY
advertisement
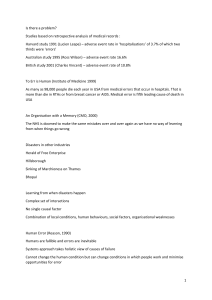
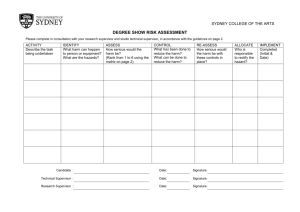
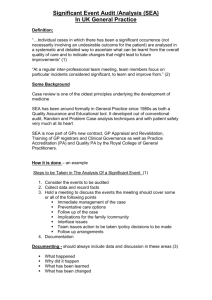
RISK MANAGEMENT The objective of managing risk is to understand, report, monitor and minimise risks to patients and staff. One of the most important aspects of risk management is learning from mistakes or near misses in order to reduce the risk of them recurring. October 2004 Risk Management A Risk Management system will enable an organisation and the people within it to identify, report and understand what goes wrong in patient care, learn from the experiences and take appropriate action to ensure that it does not happen again by sharing this knowledge. Risk is the chance of an event happening that may harm patients, their relatives, staff, and possibly the Trust’s finances and/or it’s reputation. Risk management is a systematic programme of clinical and administrative activities that are undertaken to identify, evaluate and take actions in order to reduce the risk of injury and loss. It involves: identifying, analysing, handling and monitoring of risks and learning from harmful events to avoid their recurrence. A Risk Management system will not eliminate human error or the mistakes made under pressure, but it will reduce the risk to a minimum by ensuring safe systems are in place. National Initiatives National Patient Safety Agency (NPSA) Is a special health authority formed in July 2001 after ‘Organisation with a Memory’ (DoH 2000) and ‘Building a Safer NHS for Patients’ (DoH 2001) were published. These reports exposed the need to learn more from things that go wrong and mobilised patient safety in the NHS. NPSA 7 Steps to Patient Safety: 1. Build a safety culture. 2. Lead and support your staff. 3. Integrate your risk management activity. 4. Promote reporting. 5. Involve and communicate with patients and the public. 6. Learn and share safety lessons. 7. Implement solutions to prevent harm. Risk Pooling Scheme for Trusts The National Health Service Litigation Authority (NHSLA) is established to indemnify NHS Trusts in respect of both clinical negligence and non-clinical risks. It manages both claims and litigation and has established risk management programmes against which NHS Trusts are assessed. Patient Concerns Patient Concerns re safety Don’t kill me Don’t hurt me Don’t cover up mistakes Don’t make me feel helpless Don’t tell me you can if you can’t Involve your patients, help them To reach an accurate diagnosis. Decide about appropriate treatment. Choose an experienced and safe provider. Ensure treatment appropriately administered, monitored and adhered to identify adverse events and take appropriate action. Charles Vincent & Angela Coulter (2002) And when if things do go wrong… Actively involve your patients and family. Prioritise the need to tell patients when incidents occur and provide them with clear, accurate and timely information. Make sure patients and their family receive immediate apology where it is due and are dealt with in a respectful and sympathetic way (7 Steps to Patient Safety). Creating the Culture The perfection myth - if people try hard enough they will not make any errors. The punishment myth - if we punish people when they make errors they will make fewer mistakes. The best way of reducing error rates is to target the underlying systems failures, rather than take action against the individual member of staff (NPSA 7 Steps to Patient Safety) How to Create the Culture Consistency - ensure a standard approach to Risk Management across the organisation. Policies – establish a system to ensure all policies are accepted by all clinicians; systematically disseminated and reviewed/updated. Communication - huge area of risk – Risk Pooling Scheme for Trusts (RPST) aids effective communication about risk. Education and feedback – for continuous improvement. Responsibilities It is the duty of every employee to take responsibility for the safety of themselves, their patients and colleagues. Every employee should comply with the risk management requirements of the organisation by assessing and managing risk and when necessary bring it to the attention of their line manager Individual responsibilities: Reporting incidents/accidents via the Trust’s incident form that should be sent to your line manager. See the ‘Incident Book’ yellow folder in your base. Assessing and reporting risks – being proactive by bringing to attention areas of risk that could cause harm to patients and staff. Shared learning – teams meet and discuss their experiences and that of others (e.g. national issues from NPSA). Some examples of why things go wrong Cultural Organisational Weak leadership No coherent strategies Education and research not valued Weak systems Poor communications Unsupportive environment Poor information Failures in Standards of Care External Individual Defensive to criticism Lack of skills Fortress mentality Little collaboration or networking Bad team working Poor motivation and attitude Ostrich mentality Risk Areas Clinical practice (delay in diagnosis). Prescribing. Medico-legal issues. Organisation/staffing. Health and safety - including premises, first aid, fire, VDUs, infection control, sharps & waste, hazardous substances and equipment (autoclaves, fridges, nebulisers, sphygmomanometers, lasers, scales). Patient records/confidentiality. Record keeping. Patient experience and complaints. What is a Risk Assessment? A risk assessment is a careful examination of what, in your work, could be a hazard. This enables you to decide whether you have taken enough precautions, or should do more to prevent harm. The aim is to make sure that no one gets hurt or becomes ill. The Five Stages of Risk Assessment Step 1 Hazard means anything that can cause harm (e.g. chemicals, electricity, machinery). Risk is the chance, high or low, that somebody will be harmed by the hazard. Walk around your workplace and look afresh at what could reasonably be expected to cause harm. Concentrate on significant hazards that could result in serious harm or affect several people. Ask your colleagues what they think – they may have noticed things that are not immediately obvious. Step 2 Don’t forget to consider: Trainees, new/expectant mothers, etc who may be at particular risk. Cleaners, visitors, contractors, maintenance workers, etc who may not be in the workplace at all times. Members of the public. Step 3 Consider: Can I get rid of the hazard altogether? If not, how can I control the risks so that harm is unlikely? Try a less risky option. Prevent access to the hazard (e.g. by guarding). Organise work to reduce exposure to the hazard. Issue personal protective equipment. Provide welfare facilities (e.g. hand washing). Step 4 You must record the significant findings of your assessment, e.g. “Electrical installations: insulation and earthing checked and found sound”. Keep the record for future reference. You must also tell your employees about your findings. You must be able to show that: A proper check was made. You asked who might be affected. You dealt with all the obvious significant hazards, taking into account the number of people who could be involved. The precautions are reasonable, and the remaining risk is low. Step 5 If there is any significant change in your workplace, or new equipment, review your assessment. It is good practice to review your assessment from time to time to make sure that your precautions are still working effectively. Definition of Incidents Adverse incident: Any unfavourable event or circumstance that results in a harmful outcome of clinical care or therapeutic intervention. Including property loss or damage. Accident: Any unexpected event which results in harm, personal injury or ill health e.g. needlestick, fall. Near miss: Any event or circumstance that was prevented, so narrowly avoided injury or harm, but if it had occurred could have had a detrimental result. Potential Risk: Anything that poses a threat to people or service provision. Significant Event: A noteworthy event (good or bad) that is reported for the purposes of sharing learning within the clinical team. Further Investigation Incidents with a high frequency or recurring theme and those with high-risk ratings will need more detailed consideration. Root Cause Analysis (RCA) The purpose of any investigation should be: Find out the full facts, with respect to the sequence of events that led to the incident occurring. Determine what was managed well. Determine what, if anything, went wrong and identify issues of concern. Identify the actions required to prevent recurrence, and who can implement them. Incident Reporting and Significant Event Analysis (SEA) All staff must report clinical and non-clinical incidents via the Trust’s reporting system. This information can then be used to reduce risk. Significant Event Analysis includes recording events (good and bad), followed by a systematic peer review of the event, discussion to identify what happened and share the learning outcome within and outside the team. NHS organisations use SEAs as one of the ways to develop an open, transparent and blame-free culture. When errors occur it is usually the systems, rather than the individuals, which are reviewed. Independent Contractors should submit quarterly reports on Significant Events to the Clinical Governance Office. Contributing Factors to Risk Management Clinical Negligence Scheme National Patient Safety Agency Creating the Culture Risk Management Risk Register Risk Assessments Root Cause Analysis All staff responsible for Risk Risk/Patient Safety on Agenda at Team Meetings Incident Reporting Risk Management Training Caldicott/ Confidentiality/ Information Security Risk Management References The National Patient Safety Agency website: www.npsa.nhs.uk The Healthcare Commission (CHAI) website: www.healthcarecommission.org.uk The Health and Safety Executive website: www.hse.gov.uk The National Health Service Litigation Authority website: www.nhsla.nhs.uk Your local Risk Management contact details:- Corporate Services Office Bedford PCT Gilbert Hitchcock House 21 Kimbolton Road Bedford MK40 2AW Tel 01234 795714 (switchboard) Clinical Governance Team Bedford PCT Gilbert Hitchcock House 21 Kimbolton Road Bedford MK40 2AW Tel 01234 795714 (switchboard) Direct Line 01234 795760