CASE - هيئة التدريس جامعة الملك سعود

RAPID REVIEW
OF
PSYCHIATRIC DISORDERS
- ORAL
- MCQs
- CASES
Dr. MOHAMMED A AL-SUGHAYIR
COLLEGE OF MEDICINE
KING SAUD UNIVERSITY - RIYADH
1417 H - 1996 G
ةمدقم
،دعبو .مملأا ريخ يبن ىلع ملاسلاو ةلاصلاو ،ملعي مل ام ناسنلإا ملع ملقلاب ملع يذلا لله دمحلا
بطلا يف عجارملا مهأ نم اهتعمج تاباجإو ةلئسأ لكش ىلع اهتعضو ةركذم بّيتكلا اذه لصأ
لبق ةعجارملا ىلع )دوعس كلملا ةعماجب( بطلا ةيلك يف جرختلا لبق ام ةبلطل ًانوع نوكتل يسفنلا
ترصتقا دقو .ةيلمعلا يحاونلاب ةلصتملاو ةبولطملا بناوجلا مهأ ىلع زيكرتلاب كلذو ناحتملاا
ىرخلأا ليصافتلا يف ضوخلا نود جلاعلاو صيخشتلا يف ةمهملا تايساسلأا ىلع اهيف
.)كلذ وحنو ضارملأا راشتناو بابسلأاك(
- 1
ةيباتكلا ةلئسلأا نم ددع عم ،يهفشلا ناحتملاا ةرطنق روبعل بلاطلا يفكي هارأ ام تعمج دقو
ةلحرملا هذهلو )يسفنلا بطلا( لاجملا اذه يف ةلئسلأا ةعيبط حيضوتل جذومنأك )أطخو حص(
.)جرختلا لبق ام ةلحرم(
ةعيبط نم مهاوكش ةرثكو ةبلطلا ةوخلإا ةجاح هجضن مامت لبق دهجلا اذه جارخلإ ينعفد دقو
صيخشتلا قرط يف عجارملاو بتكلا ءارآ نيابتو اهتاحلطصم ضومغ عم ةصاخ اهديقعتو ةداملا
.نورخأتيو اهيف نورثعتي ةبلطلا ضعب لعج يذلا رملأا ،جلاعلاو
ةيسفنلا ضارملأا نع ةيبرعلاب باتك ـ ىلاعت الله ةئيشمب ـ ًابيرق دوهجملا اذه عبتي فوسو
ةيبرعلا ةئيبلاب ةلصتملا ثحابملا نم كلذب قلعتي ام عم اهتاجلاعو اهبابسأو اهصيخشت قرطو
ضارم لأا ترثـك دقو اميس لاو ةيدوعسلا ةيبرعلا ةكلمملا يف يسفنلا بطلا عضوو ،ةيملاسلإا
ريثكو ،يملع يبط ساسأ ىلع موقي لا اهمظعم ةريثك ةيجلاع قرط ترشتناو ًارخؤم ةيسفنلا
بتكلا نأو ةصاخ ،هريغو ضيرملاب قحلت ةيلامو ةينيدو ةيحص رارضأ هببسب لصحي اهنم
ن ع ةيفرح ةمجرت وه امنإ دوجوملا مظعمو ًادج ةليلق ةيبرعلا ةغللاب ةفلؤملا ةيسفنلا ةيبطلا
بناوجلا نع )اهلقن يغبني يتلاو( ةيبطلا ةمولعملا هيف زيمتت لا د قو ةيبرغلا ةيبنجلأا عجارملا
ةئيبلا عم مءلاتت لا دقو صيحمتو رظن عضوم يه يتلاو( ةيبرغلا ةيقلاخلأاو ةيكولسلا
ضايرلا 21525 ب .ص
.)ةيملاسلإا
..ليبسلا ءاوس ىلإ يداهلا وهو نلاكتلا هيلعو ناعتسملا اللهو
بطلا ةيلك ـ يسفنلا بطلا مسق
ر يغصلا الله دبع نب دمحم .د
ضايرلاب دوعس كلملا ةعماج
.ـه 1417 11485
- 2
CONTENT
SECTION - A : ORAL.................................................. 7
* Guidelines ............................................................. 9
1 - Classification ............................................... 10
2 - Psychopathology .......................................... 12
3 - Organic Psychiatry ...................................... 14
4 - Substance abuse ............................................ 16
5 - Anxiety disorders ......................................... 19
6 - Somatoform disorders ................................. 24
7 - Affective (Mood) disorders ........................... 28
8 - Schizophrenia .............................................. 31
9 - Emergency Psychiatry ................................. 34
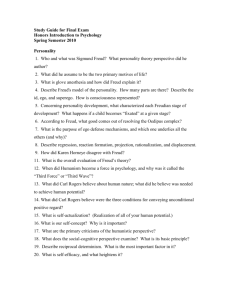
10 - Personality disorders ................................. 37
11 - Drugs and ECT .......................................... 42
12 - Child Psychiatry ......................................... 49
13 - Psychotherapy ............................................. 53
* Test Questions ..................................................... 55
SECTION - B : MCQs ................................................ 57
* Guidelines ........................................................... 61
* Questions .............................................................. 62
* Answers ............................................................... 77
SECTION - C : CASES .............................................. 79
REFERENCES .......................................................... 91
- 3
- 4
SECTION - A
ORAL
Two examiners to one student?! - Oral exam is a real stress
- 5
- 6
ORAL EXAM : GUIDE LINES
1 - Certain topics to be well covered, include:
* Classification * Psychopharmacology
* Depression * Phobias
* Emergency * Obsessive Compulsive disorder
* Delirium * Dementia
* Schizophrenia * Mania.
2 - Prepare concise informative answers in a systematic approach.
3 - Be calm, confident (not overconfident) and non hesitant.
Feel as if you were talking to a lay man (non-psychiatrist).
[If too anxious: Propranalol 20mg p.o. one hour before.]
4 - Listen carefully to every word in the question paying a special attention to hints.
5 - Avoid giving excuses (e.g. I had another exam yesterday).
6 - Use non-verbal (body) language keeping good eye contact with the examiner.
7 - Remember that the facial expression of the examiner does not necessarily reflect his evaluation of your answers, so do not be disappointed or lose your self-esteem.
8 - Make your answers direct and clear to the specific question, WHAT? means: what? not “how”? or “when”?.
9 - If you do not know the answer do not hesitate to admit that and do not waste your time in evasive or circumstantial answers
.
CLASSIFICATION
[1] HOW WOULD YOU CLASSIFY PSYCHIATRIC DISORDERS?
- I would classify them into two main groups: (see A & B)
A – ORGANIC; Includes:
1 - Acute organic brain syndrome (delirium).
2 - Chronic organic brain syndrome (dementia).
3 - Amnesic syndrome (including Wernicke-Korsakov’s syndrome).
4 - Complex partial seizure (Temporal lobe epilepsy).
5 - Psychoactive substance induced disorders.
6 - Drug induced disorders (e.g. due to steroids).
7 - Those due to Focal brain lesions (e.g. frontal lobe infarction).
B – FUNCTIONAL; (Includes I, II & III):
- 7
I Psychoses (plural of psychosis) a - Schizophrenic (acute and chronic).
b - Mood (affective) disorders (mania-major depression with psychosis).
c - Schizoaffective disorder (both schizophrenic and affective features).
d - Schizophreniform dis. (Schizophrenic features with duration 2 6 mos).
e - Delusional disorders (e.g. grandiose, persecutory, mixed ...etc).
f - Brief psychosis (reactive and non-reactive types).
II Neuroses (plural of neurosis) a - Dysthymia (chronic mild depression).
b - Anxiety Disorders:
1- Generalized Anxiety Disorder; 2- Panic Disorder; 3 - Agoraphobia 4-
Social Phobia; 5- Specific Phobia; 6- Obsessive Compulsive Disorder; 7-
Post-Traumatic Stress Disorder; 8- Acute Stress Disorder.
c - Somatoform Disorders:
1- Somatization Disorder; 2- Conversion Disorder (hysteria); 3-
Hypochondriasis; 4-Psychogenic Pain; 5- Dysmorpho phobia.
d - Adjustment Disorders:
* with depressed mood * with anxiety ...etc.
III Other Disorders including:
* Personality Disorders, * Factitious Disorders, * Impulse Control Disorders, *
Eating Disorders, * Sleep Disorders, * Sexual Disorders, * Dissociative
Disorders, ...etc.
[2] WHAT DO YOU KNOW ABOUT MULTIAXIAL SYSTEM OF CLASSIFICATION OF
MENTAL DISORDERS?
A - It is an American system for classifying mental disorders in which 5 axes are used in
each case as follows:
Axis I : For mental disorder (e.g. major depression).
Axis II: For personality disorder (e.g. dependent personality disorder); For * specific developmental disorders & Mental retardation.
Axis III: Physical diseases (e.g. hypothyroidism).
Axis IV: Severity of psychosocial stressors (e.g. mild, moderate, severe, extreme, minimal, ...etc...).
Axis V: Level of functioning compared to the past year.
- 8
PSYCHOPATHOLOGY
[3] Q. WHAT IS THE DEFINITION OF DELUSION?
A - It is a fixed unshakable false belief that is against one’s sociocultural and educational background, and the patient lacks insight into it. (e.g. fixed belief of being persecuted and followed by CIA).
* It usually indicates a psychotic disorder.
[4] Q. WHAT IS THE DEFINITION OF OVERVALUED IDEA?
A - It is a strongly held belief that dominates a persons life and may affect his actions, but shakable. (e.g. being convinced that cancer is contagious).
[5] Q. WHAT IS THE DEFINITION OF OBSESSIONS?
A - Obsessions are recurrent and persistent thoughts, impulses, or images that enter the mind despite efforts to exclude them, and that leads to distress.
[6] Q. WHAT IS THE DEFINITION OF COMPULSIONS?
A - Compulsions are repeated, stereotyped actions carried out by a patient to reduce the distress associated with the obsessions. They are called rituals. They include:
checking, cleaning, counting, dressing, .....etc.).
[7] Q. COMPARE AND CONTRAST DELUSIONS, OBSESSIONS AND
OVERVALUED IDEAS.
A - * All are thought problems but delusions indicate a psychotic disorder, obsessions indicate a neurotic disorder whereas overvalued ideas could occur in normal people.
* In delusion usually the patient accepts the idea as true (fixed belief and unshakable), in overvalued idea also the patient accepts the idea as true (but shakable) whereas in obsessions the patient is aware that the idea is untrue and sometimes silly and absurd.
[8] Q. WHAT IS THE DEFINITION OF HALLUCINATIONS?
A - They are perceptions without an external stimulus, to the corresponding sense organ. Perceived as coming from outside the head.
[9] Q. WHAT ARE THE DIFFERENT TYPES OF HALLUCINATIONS?
A - According to sensory modality:
* Auditory “usually associated with schizophrenia”
* Visual “usually associated with organic brain diseases”
* Olfactory * Tactile.
Special kinds of auditory hallucinations:
- 9
* second person, * third person, * thought echo.
[10] Q. WHAT IS THE DEFINITION OF ILLUSION?
A - An illusion is a misperception of an external stimulus.
B - Usually occurs when the level of sensory stimulation is reduced. (e.g. in delirium).
[11] Q. WHAT ARE PSEUDOHALLUCINATIONS?
A - They are type of imaginary perception coming from inside the head, which occur in clear consciousness and usually the patient has insight into them.
ORGANIC PSYCHIATRY
[12] Q. WHAT IS THE DEFINITION OF DELIRIUM?
A - Acute global organic disturbance of higher mental functions with fluctuation of consciousness.
[13] Q. WHAT ARE THE MAIN FEATURES OF DELIRIUM?
A - * Fluctuation of consciousness * disorientation * illusions * hallucinations * behavioral disturbances * emotional disturbances: worries, fearfulness, anxiety * fleeting delusions.
[14] Q. WHAT IS THE DEFINITION OF DEMENTIA?
A - Chronic global organic disturbance of higher mental functions without disturbance of consciousness (mainly memory and intellectual dysfunctions).
[15] Q. WHAT ARE THE VARIOUS CAUSES OF DEMENTIA?
A -
I - Treatable
* Multi-infarct dementia
* Normal pressure hydrocephalus
* Metabolic disorders e.g. hypothyroidism
* Malnutrition
* Heart failure, liver failure, etc...
II - Non-Treatable
* Alzheimer disease
* Parkinson’s disease
* Huntington’s Chorea
* Pick’s disease
- 10
* AIDS
[16] Q. HOW WOULD YOU MANAGE A DELIRIOUS PATIENT?
A - Search for the cause (e.g. hypoxemia) and treat it.
B - Small doses of Haloperidol (e.g. 1.5mg TDS) to control the disturbed behavior and calm the patient.
C - The patient should be comfortable, adequately hydrated and placed in a well-lit
room, few nursing staff with repeated explanations and orientation.
[17] Q. WHAT ARE THE FACTORS THAT SUGGEST ORGANIC CAUSES OF THE
MENTAL ILLNESS?
1 - Disturbance of cognitive functions: *orientation * attention and concentration
* memory
2 - Disturbances of consciousness.
3 - Neurological features e.g. hemiparesis, dysarthria.
4 - Visual hallucinations.
5 - When the clinical picture is not typical of functional disorder.
6 - Presence of medical (especially neurological) disease.
- 11
SUBSTANCE ABUSE
[18] Q. MENTION THE MAIN ALCOHOL - RELATED DISABILITIES:
A -
* Physical:
- GI: gastritis - liver disease...
- Cardiac: cardiomyopathy...
- Neurological: Cerebellar degeneration, seizure...
- Nutritional: vitamin deficiency, anemia...
- Accidents.
* Psychological:
- Depression and anxiety
- Personality changes
- Morbid jealousy and sexual dysfunction
- Suicide
- Amnesia, delirium, dementia
- Psychosis.
* Social:
- Marital and family problems
- Financial problems
- Problems at work, school, etc...
[19] Q. WHAT ARE THE FEATURES OF ALCOHOL WITHDRAWAL?
A - 1- Nausea, 2- Sweating, 3- Agitation, 4- Acute tremulousness, 5- Misperception and hallucinations.
[20] Q. WHAT IS DELIRIUM TREMENS?
A - It is a severe form of withdrawal picture that appear around 48 hours after the last alcohol ingestion. Usually occurs in those who have been excessively using alcohol for several years.
- It is characterized by disturbance of consciousness autonomic disturbances (including gross tremor), dehydration, electrolyte and cardiovascular disturbances.
- It lasts for 3-4 days followed by prolonged sleep then recovery. Death rate is around
10%.
- It is considered as medical emergency that should be treated carefully, It’s treatment includes rehydration, multivitamin, benzodiazepine (for the risk of seizure).
- 12
[21] Q. MENTION THE MAIN FEATURES OF OPIATES WITHDRAWAL:
A - Lacrimation - Rhinorrhea - Yawning - Sweating - Shivering - Mydriasis - Abdominal cramps - Diarrhea - Tachycardia.
- These features start few hours after last dose.
- Peak: 24-48 hours then subside in 7-10 days.
[22] Q. MENTION THE MAIN FEATURES OF STIMULANTS ABUSE:
A - Stimulants (such as amphetamine and cocaine) have sympathomimetic effect:
- Mydriasis - high BP - high pulse - Sweating or chills - Arrhythmia - Tension -
Anxiety - Anger - Hypervigilance - Euphoria - Impaired functioning and judgment.
[23] Q. WHAT ARE THE MAIN COMPLICATIONS OF OPIOIDS?
A - Physical:
- weakness - malaise - tremor - miosis - constipation - impotence - IV complications: skin ulcers - vein thrombosis - liver and kidney damage.
B - Psychological:
- Depression - personality deterioration - apathy etc...
C - Social:
- Financial problems - marital and family conflicts - problems at work and school.
[24] Q. WHAT ARE THE MAIN FEATURES OF CANNABIS INTOXICATION?
A -
Motor incoordination - Euphoria - Sense of slowed time - Impaired judgment -
Perceptual disturbances - Tachycardia - increased appetite - Dry mouth -
Conjunctival injection.
- 13
ANXIETY DISORDERS
[25] Q. WHAT ARE THE FEATURES OF GENERALIZED ANXIETY DISORDER
(GAD)?
A - Psychological:
- fearful anticipation - irritability - feeling of restlessness - sensitivity to noise - excessive worries - poor concentration - subjective report of poor memory.
- Physical:
1 - Respiratory : - difficulty in inhaling - feeling of constriction in the chest.
2 - Cardiovascular: - feeling of discomfort over the heart - palpitation - awareness of missed beats.
3 - GI: - difficulty in swallowing - dry mouth - epigastric discomfort - disturbed bowel habits.
4 - Neurological: - tinnitus - dizziness - prickling sensations - blurring of vision - headache.
5 - Genito-urinary: - increased frequency and urgency of micturation - failure of erection - reduced libido.
6 - Musculo-skeletal: - aching and stiffness especially in back and shoulders - trembling hands.
7 - Sleep disturbances: - initial and middle insomnia - bad dreams.
[26] Q. HOW WOULD YOU MANAGE G.A.D.?
A - Management includes:
a - Physical measures, may include:
1 - Benzodiazepines (short term to avoid dependence).
2 - Tricyclic antidepressants in small divided doses (e.g. Imipramine 10mg TDS).
3 - B-blockers (mainly for physical symptoms like palpitation).
4 - Serotonin reuptake inhibitors e.g. Fluvoxamine.
b - Psychological: - Relaxation training - Reassurance & counseling.
c - Social: to reduce current social stresses.
[27] Q. MENTION THREE MEDICAL ILLNESSES THAT CAN CAUSE ANXIETY?
A -
1 - Hyperthyroidism.
2 - Phaeochromocytoma.
3 - Hypoglycemia.
- 14
[28] Q. WHAT DOES THE TERM “PHOBIA” MEAN?
A - Phobia is an abnormal intense fear of certain objects (or situations) accompanied by a strong wish for avoidance.
[29] Q. WHAT DOES THE TERM “AGORAPHOBIA” MEAN?
A - Strictly speaking it means fear of open places. But often used for a fear of:
- crowds - shops and supermarkets - buses and trains.
[30] Q. WHAT ARE THE FEATURES OF AGORAPHOBIA?
A - Anxiety symptoms (psychological and physical... see Q [25].
- Anxiety thoughts are characteristically centered on ideas of fainting or losing control.
- Patient may become housebound or dependent on others.
[31] Q. WHAT DOES PANIC ATTACK MEAN?
A - A distinct avoidance of intense fear develops abruptly and reaches a peak within 10 minutes. It’s features include:
* palpitation * shaking * sweating * feeling of choking * dizziness * fear of losing control, fainting or dying * chest pain or discomfort * Nausea * paraesthesia
* depersonalization * derealization.
- It may occur with or without agoraphobia.
[32] Q. WHAT IS SOCIAL PHOBIA?
A - Fear and avoidance of situations in which the individual may be observed by other people (especially those unfamiliar).
[33] Q. HOW WOULD YOU TREAT “PHOBIA” IN GENERAL
A -
1 - Physical: anxiolytic drugs to reduce symptoms in the short term.
or antidepressants e.g. Impramine in small divided doses e.g. 10mg. TDS.
2 - Psychological - behaviour therapy: to overcome avoidance by systemic desensitization:
* Training the patient to relax.
* Constructing, with the patient, a hierarchy of anxiety - arousing situation.
* Presenting phobic item from the hierarchy in graded way whilst the patient inhibited the anxiety by relaxation.
3 - Social: to reduce stresses and to encourage improvement.
- 15
[34] Q. WHAT ARE THE MOST OBSESSIONAL THEMES?
A -
1 - Contamination and dirt
2 - Orderliness
3 - Aggressive actions
4 - Religious (e.g. ablutions)
5 - Sexual deviations
6 - Obsessional doubts
7 - Obsessional phobia.
[35] Q. WHAT ARE THE MAIN DIFFERENTIAL DIAGNOSES OF OBSESSIVE
COMPULSIVE DISORDER (OCD)?
A -
1 - Depression
2 - Phobia
3 - Non-pathological repetitive behaviour
4 - Obsessive compulsive personality
5 - Psychotic disorders.
[36] Q. HOW WOULD YOU MANAGE A CASE OF OCD?
A -
1 - Physical: antidepressant drugs with anti-obsessional effect like:
* Clomipramine (TCA) * SSRI (e.g. Prozac)
- Also treat any associated depression or anxiety.
2 - Psychological: - Supportive psychotherapy
- Behavioural therapy (response prevention & thought stopping technique).
3 - Social: involving other family members in the treatment program.
- 16
He has been washing for two hours and yet the idea of persistent contamination is still intruding into his mind.
- 17
SOMATOFORM DISORDERS
[37] Q. WHAT IS HYPOCHONDRIASIS?
A - It is a psychiatric disorder characterized by:
- Preoccupation with serious illness based on misinterpretation of bodily symptoms.
- Despite reassurance (after appropriate investigations) preoccupations persist.
- Excessive concern with health in general.
[38] Q. WHAT ARE IT’S DIFFERENTIAL DIAGNOSES?
A -
1 - Depression (sometimes associated with hypochondrical thoughts)
2 - Somatization (multiple complaints not related to a particular system)
3 - Generalized anxiety disorder
4 - Obsessive compulsive disorder
5 - Monosymptomatic hypochondrical delusion
6 - Body dysmorphic disorder.
[39] Q. HOW WOULD YOU MANAGE A CASE OF HYPOCHONDRIASIS?
A -
1 - Psychological: * Reassurance and explanation (the role of psychological factors in the symptoms).
2 - Social: to reduce social stresses
- to search for meaning of symptoms in social and family setting where appropriate
(e.g. the father recently died of cancer).
3 - Physical: * TCA may help some patients especially those who have depressive or anxiety symptoms.
* Avoid over investigations.
[40] Q. WHAT IS SOMATIZATION DISORDER?
A - It is a psychiatric disorder characterized by:
- multiple (at least 8) physical complaints starting before age of 30 years, involving several systems (GI, GUS, nervous, etc...)
- complaints can not be explained by a known medical disease.
[41] Q. WHAT ARE IT’S DIFFERENTIAL DIAGNOSES?
A -
1 - Depression (sometimes is associated with multiple physical complaint)
- 18
2 - Generalized anxiety disorder.
3 - Hypochondriasis.
4 - Medical diseases: SLE - chronic infections - hyper parathyroidism.
5 - Chronic fatigue syndrome.
[42] Q. HOW WOULD YOU MANAGE A CASE OF SOMATIZATION?
A - * Exclude possible physical causes.
* Aim to increase the patient’s awareness of the possibility that psychological factors are involved in the symptoms.
* See the patient in regular scheduled visits (e.g. monthly), the visits should be relatively brief.
* Avoid excessive investigations.
* Treat any associated psychiatric disorder (e.g. depression).
[43] Q. WHAT IS CONVERSION DISORDER?
A -
* It is a psychiatric disorder characterized by: conversion of intrapsychic emotional conflicts into certain physical symptoms (affecting sensory or motor functions).
* Hysteria includes:
1 - Hysterical conversion (conversion disorder)
2 - Hysterical dissociation (dissociative disorders: psychogenic fugue, psychogenic amnesia, dissociative personality and depersonalization disorder).
[44] Q. WHAT ARE THE CLASSIC CONVERSION SYMPTOMS?
A -
1 - Paralysis
3 - Aphonia
5 - Anaesthesia
2 - Blindness
4 - Deafness
6 - Gait disturbance
7 - Abdominal pain 8 - Fits (pseudo seizures).
[45] Q. HOW WOULD YOU DIFFERENTIATE SEIZURE FROM PSEUDO
SEIZURE, CLINICALLY?
A -
FEATURE preceded by: cyanosis
TRUE SEIZURE aura common
PSEUDO SEIZURE emotional stress none
- 19
self-injury incontinence body movements affected by suggestion post-ictal confusion gain common common
Tonic /
Clonic
No present
No rare rare asynchronic
Yes
None
Yes
[46] Q. WHAT IS “PRIMARY GAIN” IN HYSTERICAL CONVERSION?
A - It is the resolution of intrapsychic anxiety after developing the physical disability through conversion.
[47] Q. WHAT IS “SECONDARY GAIN”?
A - The advantage that the patient gets (e.g. drawing the attention of others).
- 20
AFFECTIVE DISORDERS
[48] Q. WHAT ARE THE MAIN FEATURES OF MANIA?
A -
1 - A distinct period of abnormal mood (elevated or irritable) for at least one week.
2 - Grandiosity
3 - Hyperactivity
4 - Hypertalkativeness
5 - Pressure of thoughts
6 - Flight of ideas
7 - Insomnia
8 - Poor judgment
9 - Clang association
10 - Over familiarity
11 - Over spending
12 - Increased libido.
[49] Q. MENTION THE MAIN DIFFERENTIAL DIAGNOSES OF MANIA
A -
1 - Schizophrenia (with affective components)
2 - Schizoaffective disorder
3 - Substance abuse especially stimulants, like amphetamine
4 - Organic mental disorders (e.g. frontal lobe syndrome).
[50] Q. HOW WOULD YOU TREAT A MANIC EPISODE?
A -
1 - Admission (for in-patient psychiatric care)
2 - Antipsychotics e.g. Haloperidol (20-40 mg/day) orally or IM.
3 - Mood - stabilizer (Lithium or Carbamazepine) (See Q [80] - [83]).
[51] Q. WHAT ARE THE MAIN FEATURES OF MAJOR DEPRESSION?
A -
1 - Low mood
2 - Low interest
3 - Chest tightness
4 - Crying bouts
5 - Pessimistic thoughts
6 - Death wishes
- 21
7 - Suicidal ideation
8 - Psychomotor retardation (sometimes agitation)
9 - Early morning wakening
10 - Fatigue and loss of energy
11 - Worthlessness
12 - Guilt feeling
13 - Poor concentration
14 - Reduced appetite and weight loss
15 - Reduced libido.
* At least two weeks period is required for the diagnosis.
[52] Q. MENTION THE MAIN DIFFERENTIAL DIAGNOSES OF DEPRESSION.
A -
1 - Anxiety: sometimes associated with depressive features
2 - Adjustment disorder with depressed mood or with mixed emotion
3 - Grief: sadness appropriate to a real loss
4 - Somatization disorder.
5 - Hypochondriasis.
* Organic causes of depression include: a - Neurological: dementia - Parkinson’s disease, multiple sclerosis, etc...
b - Endocrine: hypothyroidism - Cushing/s disease, etc...
c - Infections: T.B. influenza.
d - Systemic illnesses: SLE, RA.
e - Pharmacological: NSAID - antifungal drugs....
* Dysthymic disorder is a chronic mild depression for at least 2 years.
[53] Q. HOW WOULD YOU MANAGE A DEPRESSED PATIENT?
A - Assess the severity, admit if:
1 - suicidal, 2 - severely retarded, 3 - psychotic (patient develops hallucinations or delusions secondary to his depression).
B - ECT for those with severe depression, especially those with marked biological and psychotic features of depression.
C - Antidepressant medications (see Q [69] - [73]).
D - Cognitive behavior therapy (cognitive restructuring) and other psychological treatments if required e.g. family therapy.
- 22
- 23
SCHIZOPHRENIA
[54] Q. WHAT ARE THE CRITERIA USED TO DIAGNOSE SCHIZOPHRENIA?
A -
1 - 6 months period of disturbance (including prodromal or residual features).
2 - At least one month period of: * delusion * hallucination * disorganized speech * catatonic or disorganized behavior, or * negative features.
3 - Significant functional impairment.
4 - Exclusion of organic and other psychotic disorders.
[55] Q. WHAT ARE THE SUBTYPES OF SCHIZOPHRENIA?
A - According to DSM-4:
3- Disorganized.
5 - Residual.
2- Paranoid. 1- Catatonic.
4-Undifferentiated.
B -According to ICD-10:
3- Hebephrenic. 2- Paranoid, 1- Catatonic.
4- Undifferentiated. 5- Residual. 6 - Simple.
[56] Q. WHAT ARE SCHNEIDER’S FIRST-RANK SYMPTOMS OF
SCHIZOPHRENIA?
A -
1 - Thought insertion - withdrawal - broadcasting.
2 - Auditory hallucinations: voices commenting - arguing and/or discussing.
3 - Somatic passivity experiences.
4 - Audible thoughts (thought echo).
5 - Delusional perception (attributing a new meaning to a normal perceived object without any reason).
[57] Q. WHAT ARE THE FEATURES OF CHRONIC SCHIZOPHRENIA
(NEGATIVE FEATURES)?
A -
1 - Social withdrawal
2 - Poor self-care
3 - Lack of volition and initiation
4 - Poverty of speech and thought
5 - Thought block
6 - Slowness
7 - Blunted affect and apathy.
- 24
[58] Q. MENTION THE MAIN DIFFERENTIAL DIAGNOSES OF
SCHIZOPHRENIA.
A -
1 - Schizophreniform disorder (duration is less than 6 months)
2 - Schizoaffective disorder
3 - Delusional disorders
4 - Affective disorders (Mood disorders)
5 - Drug Abuse (especially stimulants)
6 - Personality disorders (e.g. paranoid, schizoid, schizotypal)
7 - Organic mental disorders (e.g. complex partial seizure of temporal lobe origin).
[59] Q. WHAT ARE THE LINES OF MANAGEMENT OF SCHIZOPHRENIA?
A -
1 - Physical: Antipsychotic drugs e.g. Chlorpromazine or Haloperidol (oral or depot injections = long acting)
2 - Social: Rehabilitation of the patient (day hospitals), Social skill training.
3 - Psychological: Counseling with the family, Token economy.
[60] Q. MENTION THE MAIN GOOD PROGNOS-TIC FACTORS OF
SCHIZOPHRENIA?
A -
1 - Acute onset
2 - Presence of a precipitating factor
3 - Prominence of affective symptoms
4 - Older age at onset
5 - Good premorbid personality and social relationships.
- 25
EMERGENCY PSYCHIATRY
[61] Q. HOW WOULD YOU MANAGE A VIOLENT PATIENT WHO HAS BEEN
BROUGHT TO A/E?
A -
1 - Providing a calm, reassuring and consistent environment in which the provocation is avoided.
2 - Major tranquilizer: e.g.
- Haloperidol (or Droperidol) IM 5 or 10 mg (may be repeated) or
- Chlorpromazine 50-100mg IM
3 - Physical restraints (by enough staff) to protect him and others from his potential dangerousness and to give him IM drugs if he refuses oral treatment.
4 - Admission into a close psychiatric ward for further assessment and management.
[62] Q. WHAT ARE THE DIFFERENTIAL DIAGNOSES OF VIOLENCE?
A - Causes of violence include:
1 - Psychiatric: * Schizophrenia * Mania * Personality disorders * M.R. *
Psychoactive substance abuse e.g. amphetamine.
2 - Medical:
(a) CNS problems: TLE - Delirium ...etc.
(b) Systemic: hypoglycemia - electrolyte imbalance...etc...
3 - Others: Self - defense - retaliation.
[63] Q. HOW WOULD YOU DEAL WITH A SUICIDAL PATIENT?
A -
I - Assessment of:
The risk of suicide and further deliberate self-harm.
* What were the patient’s intentions when he harmed himself?
- planning in advance
- precautions to avoid discovery
- no attempts to obtain help afterwards
- dangerous method
- final acts (e.g. writing a suicidal not)
* Does the patient now wish to die?
* What are true current problems?
* Is there any psychiatric disorder?
- 26
* Is treatment required and will the patient agree to it?
II - Management:
* Admission to protect the patient and others (e.g. spouse)
* Further evaluation of the case
* Treatment of any underlying psychiatric disorder e.g. major depression: ECT or antidepressants.
* Close observation as in-patient
* Resolving psychological and social stresses and distress
* Problem - solving counseling to: - resolve difficulties and - to deal with future crises without resorting to self harm.
* When there are interpersonal problems, it is often helpful to interview the other person involved, first alone and then with the patient.
[64] Q. WHAT ARE THE CAUSES OF SUICIDE?
A - These include: a) Psychiatric disorders:
1 - severe depression
2 - schizophrenia
3 - alcoholism
4 - drug abuse
5 - personality disorder (e.g. borderline).
6 - delirium b) Medical diseases:
* Chronic painful or disabling physical illness. c) Social:
* Stressful event
* Living alone e.g. old lady (Western countries)
* Lack of support.
- 27
PERSONALITY DISORDERS
[65] Q. HOW WOULD YOU DEFINE PERSONALITY DISORDERS?
A - They are maladaptive deeply ingrained patterns of behavior, recognizable in adolescence or earlier, continuing throughout most of adult life, either the patient or others
have to suffer, there is an adverse effect on the individual or society.
B- More commonly diagnosed in age group 18-35 years.
[66] Q. HOW WOULD YOU CLASSIFY PERSONALITY DISORDERS?
A - According to DSM 4:
Cluster A: Paranoid - schizoid - schizotypal
Cluster B: Antisocial - histrionic - narcissistic - borderline
Cluster C: Avoidant - dependent - obsessive-compulsive + personality disorders not otherwise specified.
[67] Q. MENTION THE MAIN FEATURES OF (PARANOID, SCHIZOID, ...ETC)
PERSONAL- ITY DISORDER WITH IT’S DIFFERENTIAL DIAGNOSIS (DDX)
A -
1 - Paranoid personality disorder:
* Distrust and suspiciousness of other’s motives.
* Secretive
* Argumentative
* Stubborn
* Sensitive
* Hypervigilant
* Verbally aggressive
* Projects feeling on to others
* Self important.
DDX:
1- other personality disorders: schizotypal - schizoid, etc...
2 - delusional disorders
3 - paranoid schizophrenia.
2 - Schizoid personality disorder:
* Detachment of social relationships
* Restricted range of emotional expression
* Fantasy
* Introspection
- 28
DDX:
1 - other personality disorder: avoidant - dependent, etc...
2 - schizophrenia.
3 - Schizotypal personality disorder:
* Pattern of eccentricities of behavior and oddities of: perception - though - communication.
* Social anxiety with idea of reference.
DDX:
1 - other personality disorders: paranoid - avoidant, etc...
2 - schizophrenia
3 - drug abuse.
4 - Antisocial personality disorder:
* Disregard for and violation of the rights of others
* Lack of guilt and remorse
* Impulsive behavior
* Lack of loyalty in interpersonal relationships
* Law conflicts
* Failure to learn from experience.
DDX:
1 - other personality disorders: borderline - histrionic, etc...
2 - drug abuse (may coexist)
3 - adult antisocial behavior
4 - mood disorders.
5 - Histrionic personality disorder:
* Attention seeking with excessive shallow emotion
* Self-dramatization and exaggeration
* Provocative and seductive behavior (exhibitionistic style)
* Highly dependent relationships.
DDX:
1- other personality disorders: borderline - narcissistic
2 - hysteria (conversion and dissociative disorders)
3 - somatization
4 - brief psychosis.
6 - Narcissistic personality disorder:
* Constant seeking of admiration, and crave attention
- 29
* Exaggerated self-importance and grandiosity
* Preoccupied with fantasies, success, power and intelligence
* Exploit others and seeks favor but do not return them.
DDX:
1 - other personality disorders: histrionic - obsessive - compulsive
2 - mood disorders .
7 - Borderline personality disorder:
* Instability in emotions, relationships and self - image
* Impulsivity and deliberate self - harm
* Feeling of boredom and emptiness
* Transient psychosis (paranoid) and dissociative symptoms.
DDX:
1 - other personality disorders: antisocial - narcissistic, etc...
2 - drug abuse (may coexist)
3 - schizophrenia.
8 - Avoidant personality disorder:
* Avoids new responsibilities, timid and cautious about new responsibilities
* Hypersensitive to negative evaluation
* Fearful of disapproval, criticism, and rejection
* Persistently anxious with social inhibition and feeling of inadequacy
DDX:
1 - other personality disorders: schizoid - dependent
2 - social phobia.
9 - Dependent personality disorder:
* Submissive and clinging behavior related to excessive need to be taken care of
* Week - willed
* Subordinates own needs
* Needs advice and reassurance
* Lacks self-reliance and avoids responsibilities.
DDX:
1 - other personality disorders: avoidant - schizoid, etc...
2 - agoraphobia.
10 - Obsessive - compulsive personality disorder:
* Preoccupation with perfectionism and orderliness
- 30
* Rigid, inflexible attitude with lack of adaptability
* Judgmental
* Indecisive
* Lost in detail.
DDX:
1 - other personality disorders: schizoid - paranoid, etc...
2 - obsessive - compulsive disorder (may coexist).
[68] Q. WHAT DO YOU KNOW ABOUT PROGNOSIS OF PERSONALITY
DISORDERS?
A - They tend to be rather less disordered as the patient grows older, however problems of personal relationships may persist (especially in antisocial personality disorder).
- 31
DRUGS AND ECT
[69] Q. WHAT ANTIDEPRESSANT DRUGS DO YOU KNOW?
A - There are three main groups of antidepressants: a - Tricyclic antidepressants (TCA): that include:
1 - Amitriptyline (has sedative effect)
2 - Imipramine (has less sedative effect)
3 - Clomipramine (has anti-obsessional effect). b - Serotonin - Selective - reuptake inhibitors (SSRI):
1 - Fluvoxamine (has sedative effect)
2 - Flouxetine (has no sedative effect)
* Both have anti-obsessional effect. c - Mono - Amino - Oxidase Inhibitors (MAOI):
1 - Phenelzine
2 - Tranylcypromine
3 - Isocarboxazid
* Used mainly in: 1 - resistant depression, 2 - social phobia.
[70] Q. MENTION THE MAIN SIDE EFFECTS OF EACH GROUP OF
ANTIDEPRESSANTS.
A -
a - Side effects of TCA:
* Anticholinergic effects: dry mouth - constipation - blurred vision - urinary retention - worsening of closed - angle glaucoma.
* Alpha-adrenoceptor blocking effects: postural hypotension - drowsiness - sexual dysfunction.
* Cardiac: arrhythmia - tachycardia - fibrillation or block (high doses).
b - Side effects of SSRI: nausea - vomiting - drowsiness - anorexia.
c - Side effects of MAOI: dry mouth - constipation - urinary retention - postural hypotension - hypertensive crises (dangerous).
N.B.: in clinical practice therapeutic effects outweigh side effects.
[71] Q. WHAT ARE THE MAIN USES OF TCA?
A -
1 - Depressive illness (major depression – dysthymic disorder)
2 - Obsessive compulsive disorder (Clomipramine to be used preferentially)
3 - Nocturnal enuresis in children (Imipramine)
- 32
4 - Phobic disorders.
[72] Q. WHAT ARE THE MAIN CONTRAINDICATIONS FOR TCA?
A -
1 - Heart block, 2 - Mania, 3 - Recent myocardial infarction.
[73] Q. WHAT ARE THE MAIN CONTRAINDICATIONS FOR MAOI?
A -
1 - Cardiovascular disease.
2 - Pheochromocytoma.
3 - Hepatic disease.
4 - Epilepsy and cerebrovascular disease.
[74] Q. HOW WOULD YOU CLASSIFY ANTIPSYCHOTIC DRUGS?
A - a - Phenothiazines: e.g. Chlorpromazine - Thioridazine - Trifluoperazine, etc...
b - Butyrophenones: e.g. Haloperidol - Droperidol.
c - Thioxanthenes: e.g. Flupenthixol - Zuclopenthixol.
d - Atypical antipsychotics: e.g. Clozapine.
[75] Q. WHAT ARE THE MAIN SIDE EFFECTS OF ANTIPSYCHOTICS?
A -
1 - Antidopaminergic: acute dystonia - akathisia - parkinsonism - tardive dyskinesia.
2 - Antiadrenergic: postural hypotension - inhibition of ejaculation.
3 - Anticholinergic: dry mouth - constipation - blurred vision - urinary retention.
4 - Hormonal: amenorrhea - galactorrhea - gynecomastia - weight gain.
5 - Others: allergic reactions - hepatic - hematological.
N.B.: Chlorpromazine has recognized sedative effect and it decreases BP. whereas Haloperidol has recognized extrapyramidal side effects, and less sedative and hypotensive effects.
[76] Q. WHAT DO YOU KNOW ABOUT ANTIPARKINSONIAN DRUGS?
A - These are group of drugs that are used in psychiatry to control the extrapyramidal side effects of antipsychotics. They have anticholinergic effect. Most commonly used are: Procyclidine-Benztropine and Benzhexol. Can be given P.O. or IM.
They may exacerbate the anticholinergic side effects of antipsychotics.
- 33
[77] Q. MENTION THE MAIN DRUGS USED AS ANXIOLYTICS.
A -
1 - Benzodiazepines.
2 - Beta-adrenergic antagonists.
3 - Phenothiazines (in small doses).
4 - Tricyclic anti depressants.
[78] Q. WHAT ARE THE MAIN GROUPS OF BENZODIAZEPINES?
A -
1 - Long-acting (duration is more than 24 hours): Diazepam - Nitrazepam.
2 - Medium-acting (12-24 hours): Lorazepam - Flunitrazepam.
3 - Short-acting (< 11 hours): Temazepam - Oxazepam.
[79] Q. WHAT ARE THE SIDE EFFECTS OF BENZODIAZEPINES?
A -
1 - Drowsiness.
2 - Ataxia.
3 - Release of aggression.
4 - Dependence (if given for several weeks in large doses) - withdrawal symptoms include: insomnia - irritability - anorexia - seizures - tremor.
[80] Q. WHAT DRUGS ARE USED AS MOOD STABILIZERS?
A -
* Lithium
* Carbamazepine
* Sodium Valproate.
[81] Q. WHAT ARE THE ACCEPTED SERUM LEVELS OF LITHIUM AND
CARBAMAZEPINE?
A - Lithium Serum Level: between 0.6-1.2m mol/l.
Carbamazepine Level: 8-12 ng/ml.
[82] Q. MENTION THE MAIN CONTRAINDICATIONS AND SIDE EFFECTS OF
LITHIUM:
A - Contraindications:
1 - Renal insufficiency
2 - Untreated hypothyroidism
3 - Addison’s disease.
- 34
Side-effects: nausea - vomiting - diarrhea - fine tremor - polyuria - polydepsia - teratogenicity weight gain - risk of toxicity.
Lithium Toxicity (level > 2m mol/l): hyperreflexia - drowsiness - ataxia Coarse tremor - dysarthria - blurred vision - syncope - coma - convulsions psychosis - oliguria.
N.B.: Long-term lithium use: nephrotoxicity - thyroid function disturbances (hypo or hyperthyroidism). Check renal and thyroid functions at least every six months.
[83] Q. WHAT ARE THE MAIUN SIDE EFFECTS OF CARBAMAZEPINE?
A -
* Dizziness - Diplopia - Diarrhea - Nausea - vomiting - blood disorders dermatological disorders.
[84] Q. WHAT IS ECT?
A - ECT means Electro convulsive therapy which is the application of an electric current to the skull of an anaesthetized patient to produce seizure activity while the consequent motor effects are prevented by giving a muscle relaxant.
The treatment effect depends on the cerebral seizure, presumably on the neurotransmitter changes that accompany it.
[85] Q. WHAT ARE THE MAIN INDICATIONS FOR ECT?
A -
1 - Depressive disorders especially:
* Depressive stupor
* High suicidal risk
* Failure to eat or drink
* Resistant depression, (unresponsive to drug treatment).
2 - Catatonic Schizophrenia.
3 - Post-partum psychiatric disorder (to resume the care of her baby as quickly as possible).
4 - Resistant mania.
[86] Q. WHAT ARE THE MAIN CONTRAINDICATIONS TO ECT?
A -
* Actually no absolute contraindication though some references may consider increased intracranial pressure as the only absolute contraindication.
* However relative contraindications include:
- 35
1 - Any medical disorder that increases the risk of the anesthetic procedure to an unacceptable degree.
2 - Cardiac infarction (especially 3 months - 2 years).
3 - Brain tumor.
4 - CVA.
[87] Q. WHAT ARE THE MAIN SIDE EFFECTS OF ECT?
A - Headache, short - term loss of memory - mania induction in bipolar subjects.
[88] Q. WHAT WOULD YOU DO WHEN A PSYCHOTIC PATIENT IS NOT
COMPLIANT WITH HIS ORAL ANTIPSYCHOTIC DUGS?
A - I would give him long-acting depot injection of antipsychotic like Haldol decanoate or Depixol every four weeks or so (Test dose: 1/4 full dose 3-5 days before).
- 36
CHILD PSYCHIATRY
[89] Q. WHAT IS INFANTILE (CHILDHOOD) AUTISM?
A - It is a pervasive developmental disorder of behavior starting in early childhood after a period of normal development (before 30 months).
[90] Q. MENTION IT’S MAIN FEATURES.
A -
1 - Inability to relate (no warm emotional relationships with people, no response to parents affectionate behavior by smiling or cuddling. A characteristic sign is gaze avoidance.
2 - Speech and language disorders: speech may develop normally and then decline or develop late, or never develop.
3 - Resistance to change: may prefer the same food, insist on wearing the same clothes or engage in the same repetitive games.
4 - Odd behavior and mannerism
5 - Other features: overactivity - poor sleep - emotional lability - mental subnormality (75% of them) seizures (25% of them - around adolescence).
[91] Q. WHAT ARE THE MAIN FEATURES OF HYPERKINETIC SYNDROME
(ATTENTION - DEFICIT HYPERKINETIC DISORDER)?
A -
- poor attention
- sustained motor activity and extreme restlessness.
- impulsiveness and recklessness.
- learning difficulty.
- tempers and aggression.
- fluctuation of mood (depressive mood is common).
[92] Q. WHAT DRUGS MAY BE USED IN TREATMENT OF HYPERKINETIC
SYNDROME?
A - Stimulant drugs such as dextroamphetamine and methyl-phenidate. They reduce hyperactivity through stimulation of cortical inhibition.
There side effects include: anorexia-growth inhibition - depression.
[93] Q. WHAT IS CONDUCT DISORDER?
A -
- 37
- It is a childhood psychiatric disorder characterized by severe and persistent antisocial behavior (aggressive behavior to other children, rebellion against the parents, disobedience, lying, stealing, vandalism, fire setting, truancy...).
- It is common psychiatric problem in the community.
[94] Q. WHAT EMOTIONAL DISORDERS OF CHILDREN DO YOU KNOW?
A -
- Emotional disorders are group of childhood disorders that have much the same meaning as neurosis in adult psychiatry.
- They include:
* Anxiety disorders: separation anxiety - phobic disorder - school refusal.
* Somatization.
* Obsessive-Compulsive behavior.
* Depressive disorder.
[95] Q. WHAT ARE THE MAIN FEATURES OF CHILDHOOD ANXIETY
DISORDER?
A -
* overdependence * Fearfulness
* Excessive worrying * sleep disturbances
* physical symptoms: headache, nausea, vomiting, abdominal pains, bowel disturbances.
[96] Q. WHAT IS SCHOOL PHOBIA?
A - It is a childhood psychiatric disorder characterized by persistent reluctance or refusal to go to school in order to stay with major attachment figure.
[97] Q. WHAT ARE THE MAIN CAUSES OF SCHOOL REFUSAL?
A -
1 - Separation anxiety.
2 - Fear of travel.
3 - General social withdrawal.
4 - Specific fears at school.
N.B.: Their academic attainments usually are good or superior
Boy: Girls - equal
- 38
[98] Q. WHAT IS FUNCTIONAL ENURESIS?
A - Repeated involuntary voiding of urine after an age at which continence is usal (5 years) in the absence of any identified physical disorder.
- Nocturnal = bed wetting.
- Diurnal = occurring during waking hours.
- Primary: if there has been no preceding period of urinary continence for at least 1 year.
- Secondary: if there has been period of urinary continence for this period.
[99] Q. WHAT IS THE TREATMENT OF NOCTURNAL ENURESIS?
A -
1 - Treat any physical disorder (e.g. UTI).
2 - Treat any psychological problems.
3 - Fluid restriction before bedtime.
4 - Behavioral therapy: star charts, Bell and pad alarm.
5 - Advice to parents (not to criticize the child...).
6 - Tricyclic antidepressants (e.g. Imipramine small doses).
[100] Q. WHAT IS FUNCTIONAL ENCOPRESIS?
A - Repeated passing of faeces into inappropriate places after the age at which bowel control is usual (4 years).
[101] Q. HOW WOULD YOU ASSESS A CHILD WITH FUNCTIONAL
ENCORPRESIS?
A -
* Full history, mental state and physical examinations.
* Exclude a primary cause e.g. chronic constipation.
* Assess parental attitude, emotional factors in the child, and the child’s concerns about the problem.
- 39
PSYCHOTHERAPY
[102] Q. WHAT IS PSYCHOTHERAPY?
A -
* Generally speaking psychotherapy includes non-pharmacological (psychological) therapeutic techniques like:
- behavioral therapy
- cognitive therapy
- psychoanalytic therapy
- family therapy
- group therapy, etc...
* Strictly speaking psychotherapy means:
- informed and planful application of techniques (other than behavioral) which lead to under standing, integration and acceptance of self.
[103] Q. WHAT DO YOU KNOW ABOUT BEHAVIOUR THERAPY?
A -
* Behavior therapy is a kind of psychological treatments based on experimental psychology (classical and operant conditioning) that aims to correct maladaptive behavior by deconditioning and reconditioning.
- It is indicated in:
* phobias
* compulsions
* nocturnal enuresis
* sexual dysfunctions
* tics
* anxiety
* obesity
* smoking, etc...
[104] Q. WHAT DO YOU KNOW ABOUT COGNITIVE THERAPY?
A -
* It is a kind of psychological treatments based on the theory that behavior is secondary to the way in which individuals think about themselves and their roles in the world. It aims at correcting cognitive distortions (errors in thinking) that lead to psychological suffering.
* It is indicated in:
- 40
- depression (mild to moderate)
- anxiety disorders
- substance abuse
- to increase compliance with medication.
- 41
TEST QUESTIONS
1 - How would you test attention and concentration?
2 - What are the cognitive functions?
3 - How would you differentiate Psychoses from Neuroses?
4 - What is the most important investigation that you should request before starting a patient on lithium?
5 - What are the various types of delusions?
6 - Compare and contrast Mania and Schizophrenia?
7 - What is the mechanism of Tardive Dyskinesia?
8 - What is Nihilistic delusion?
9 - What is the differential diagnosis of weight loss?
10 - Compare hallucinations in Schizophrenia with hallucinations in severe major depression?
11 - Compare Wernicke’s encephalopathy with Korsakoff’s psychosis?
12 - What do you know about anorexia nervosa?
13 - What is the differential diagnosis of acute psychosis?
- 42
- 43
SECTION - B
MCQ
- 44
- 45
Patients are human being, while cars are not.
- 46
- 47
THE MULTIPLE CHOICE QUESTIONS (MCQs)
* The multiple choice questions (MCQs) are now widely used in examinations.
* The most commonly used format is the “multiple true - false”.
* In psychiatric MCQs, words such as:
“commonly - frequently - characteristic” should be carefully considered.
* MCQs Terms:
[1] Always: 100% (rarely used in good MCQs).
[2] Never: 0% (hardly ever used in good MCQs).
[3] Invariably: 98 - 99% of time.
[4] Usually: 60% or more.
[5] Majority: 50% or more.
[6] Frequently: 30-50%.
[7] Commonly: 50% or more (but sometimes mean as little as 20-25%).
[8] Rarely: Less than 5%.
[9] Characteristic: A feature that is of some diagnostic significance. If such feature is absent the diagnosis would be in doubt.
[10] Pathognomonic: A feature that occurs only in the disorder named.
[11] Specific: Sometimes used as a synonym of Pathognomonic, but sometimes not so clear.
[12] Is associated with: more commonly than chance expectation.
- 48
PSYCHOPATHOLOGY
1 - CATATONIC FEATURES INCLUDE: a - posturing b - negativism c - waxy flexibility d - elective mutism e - catalepsy.
2 - DELUSIONS ARE: a - misinterpretation of external stimuli. b - out of the cultural background of the patient. c - invariably occur in schizophrenia. d - considered as cognitive disturbances. e - diagnostic of delusional disorders.
3 - HALLUCINATIONS: a - disturbances of thought process. b - visual type are common in schizophrenia. c - can be secondary to mood disorders. d - best treated by antipsychotic treatment. e - all the above are true.
4 - PSEUDOHALLUCINATIONS: a - occur in bereavement. b - occur in normal people. c - usually indicate psychosis. d - common in schizophrenia. e - all the above are false.
5 - FLIGHT OF IDEAS: a - associated with rapid speech. b - associated with pressure of thought. c - occur in delirium. d - occur in hypothalamic lesion. e - all the above are true.
SCHIZOPHRENIA
6 - FEATURES OF SCHIZOPHRENIA:
- 49
a - delusion of persecution b - chronic relapsing course c - flight of ideas d - abstract thinking e - guilt feeling.
7 - AETIOLOGY OF SCHIZOPHRENIA: a - is still not well known. b - twin studies revealed no genetic factors. c - dopamine receptors are hypersensitive. d - psychological factors have a role. e - autoimmune process may have a role.
8 - FIRST RANK SYMPTOMS: a - are pathognomonic of schizophrenia. b - include thought echo. c - include delusional mood. d - may occur in mood disorders. e - respond to antipsychotic medications.
9 - TREATMENT OF SCHIZOPHRENIA: a - oral haloperidol b - holoperidol injections. c - long acting depot injections. d - clozapine for resistant cases. e - resperidone is a new drug with good results.
10 - IN SCHIZOPHRENIA: a - simple schizophrenia has good prognosis. b - gradual onset is a bad prognostic factor. c - relapse rate decreases if the family is overprotective.
d - amphetamine abuse may precipitate the illness. e - all the above are true.
MOOD DISORDERS
11 - MANIA: a - is invariably associated with grandiose delusion.
b - clang association is a feature.
c - punning is a feature.
- 50
d - if a patient has a paranoid delusion the diagnosis of mania is remote.
e - brief minor depressive feelings can occur during manic episode.
12 - DIAGNOSIS OF BIPOLAR MOOD IDSORDER: a - requires manic and depressive episodes.
b - one manic episode is enough for the diagnosis.
c - one major depressive episode is enough for the diagnosis.
d - schizoaffective disorder should be excluded.
e - mixed episodes (mania and depression) are considered as bipolar mood disorders.
13 - MAJOR DEPRESSION: a - one week period is required for diagnosis.
b - auditory hallucinations occur in severe cases.
c - high risk of suicide.
d - early morning wakening is a characteristic feature.
e - can resolve without treatment.
14 - ORGANIC CAUSES OF DEPRESSION INCLUDE: a - SLE b - Hypothyroidism c - Addison’s disease d - Parkinsonism e - Multiple sclerosis.
15 - BIPOLAR MOOD DISORDERS: a - genetic factors have a role in the etiology.
b - carbamazepine is indicated in rapid cyclers.
c - ECT is sometimes indicated.
d - all the above are true.
e - unipolar depression is more common in female patients.
- 51
ANXIETY DISORDERS
16 - GENERALIZED ANXIETY DISORDER: a - is also called anxiety neurosis.
b - late insomnia is a feature.
c - hyperthyroidism should be excluded.
d - can be associated with obsessional thoughts.
e - is usually treated by chlorpromazine.
17 - SOCIAL PHOBIA: a - it is a type of anxiety disorders.
b - in some patients it leads to alcohol abuse.
c - avoidant personality disorder may coexist.
d - agoraphobia is a differential diagnosis.
e - Propranalol is indicated.
18 - AGORAPHOBIA: a - is associated with panic attacks in some patients.
b - is also called “house bound syndrome”.
c - is associated with a stable family back ground.
d - the most effective treatment is benzodiazepine.
e - common in children.
19 - OBSESSIVE COMPULSIVE DISORDER: a - patient usually has good insight.
b - most of patients do not come early to psychiatric clinic.
c - it is considered as anxiety disorder.
d - obsessional phobia is a feature.
e - may be the early presentation of schizophrenia in some patients.
20 - HYPERVENTILAYTION SYNDROME: a - hyperventilation causes respiratory acidosis.
b - calcium level in the blood increases.
c - fainting is a feature.
d - carpopedal spasm is a feature.
e - treated by oxygen.
ORGANIC PSYCHIATRY
21 - DELIRIUM: a - cognitive impairment in clear consciousness occurs.
- 52
b - is regarded as organic psychosis.
c - alcohol withdrawal could be a cause.
d - is a medical emergency.
e - IV diazepam 50mg is indicated.
22 - DEMENTIA: a - the course is episodic.
b - perseveration of speech occurs.
c - catastrophic reaction is a feature.
d - confabulation occurs.
e - depression is an important differential diagnosis to be excluded.
23 - HEAD INJURY: a - posttraumatic amnesia is a sequel.
b - noncommunicating hydrocephalus is a sequel.
c - retrograde amnesia is a good guide to the severity.
d - is sometimes followed by personality changes.
e - leads to multi-infarct dementia.
24 - MULTI-INFARCT DEMENTIA: a - is also called vascular dementia.
b - brain CT scan is indicated.
c - the course is downhill chronic course.
d - is associated with focal neurological deficit.
e - occurs in hypertensive patients.
25 - PSYCHOSIS IN EPILEPSY COULD BE DUE TO: a - epileptic ictus.
b - post-ictal confusion.
c - overdose of anticonvulsants.
d - structural brain abnormality.
e - all of the above.
- 53
PERSONALITY DISORDERS
26 - DIAGNOSIS OF PERSONALITY DISORDER: a - is usually difficult.
b - is based on etiological factors.
c - schizophrenia is a differential diagnosis.
d - once established, schizophrenia is excluded.
e - all are false.
27 - CLASSIFICATION OF PERSONALITY DISORDERS: a - cluster A includes paranoid, schizoid and antisocial.
b - cluster B includes histrionic, borderline and avoidant.
c - in cluster C patients are emotional, dramatic and erratic.
d - ICD-10 system includes schizotypal personality disorder.
e - all are false.
28 - ANTISOCIAL PERSONALITY DISORDER: a - lack of remorse.
b - chronic feelings of emptiness.
c - recurrent suicidal behavior.
d - sense of entitlement.
e - viewing self as socially inept.
29 - BORDER LINE PERSONALITY DISORDER: a - identity disturbance.
b - unwillingness to get involved with people unless certain of being liked.
c - perfectionism that interferes with task completion.
d - appearing indifferent to praise or criticism by others.
e - chronic feeling of emptiness.
30 - THE MANAGEMENT OF PERSONALITY DISORDER: a - little can be done to change personality.
b - the relationship with the doctor is important.
c - drug treatment has little value.
d - improving low self-esteem is required.
e - avoid prescribing hypnotic drugs.
- 54
SUBSTANCE ABUSE
31 - THE FOLLOWING STATEMENTS ARE TRUE: a - dependence includes withdrawal states and tolerance.
b - tolerance: features that appear when the substance is stopped.
c - intoxication: features that appear when the substance is eliminated.
d - withdrawal: features that disappear when the substance is reduced.
e - Gamma GT is increased in alcoholics.
32 - COMPLICATION OF ALCOHOL ABUSE: a - anxiety b - dementia c - cardiomyopathy d - cerebellar degeneration e - hallucinations.
33 - TREATMENT OF ALCOHOL ABUSE: a - asses the extent of drinking.
b - vitamin B supplement.
c - disulfiram is commonly used.
d - social support.
e - all are true.
34 - ABUSE OF HYPNOTICS: a - includes heroin.
b - physical tolerance develops more rapidly than psychological.
c - intoxication and withdrawal resemble that of alcohol.
d - withdrawal is treated by phenothiazines.
e - avoid phenobarbitone in the treatment of withdrawal.
35 - ABUSE OF OPIOIDS: a - includes pethedine.
b - leads to overactivity and paranoid psychosis.
c - includes cocaine.
d - leads to amotivational syndrome.
e - opioids are derived from the plant cannabis sativa.
- 55
SOMOTOFORM DISORDERS
36 - SOMATIZATION: a - usually starts after the age of 30 years.
b - it involves multiple systems.
c - SLE is a differential diagnosis.
d - is sometimes intentionally produced by patients.
e - patients usually consult many doctors demanding more investigations.
37 - HYPOCHONDRIASIS: a - preoccupation with serious illness.
b - repeated investigations are not encouraged.
c - depression should be excluded.
d - occurs more in obsessional persons.
e - tricyclic antidepressants help some patients.
38 - PSYCHOGENIC PAIN: a - is consistent with the anatomical distribution of CNS.
b - intentionally produced by the patient.
c - analgesic drugs give a reasonable relief.
d - responds better to antipsychotic drugs.
e - responds better to tricyclic antidepressants.
39 - CONVERSION DISORDER (HYSTERIA): a - is also called dissociative disorder.
b - intentionally produced by the patient.
c - involves sensory system.
d - involves motor system.
e - over protection made by the family may aggravate it.
40 - BODY DYSMORPHIC DISORDER: a - preoccupation with an imagined defect in appearance.
b - depression could be the cause.
c - seen in Plastic Surgery.
d - exclude hypochondriasis.
e - easy to treat.
- 56
PSYCHOPHARMACOLOGY AND ECT
41 - ANTIDEPRESSANTS: a - imipramine has a good sedative effect.
b - fluoxetine (prozac) belongs to SSRI group.
c - clomipramine has been used to treat obsessions.
d - may induce mania.
e - usually lead to dependence due to tolerance.
42 - ANTIPSYCHOTICS: a - are used in the treatment of manic episode.
b - are used in the treatment of delirium.
c - acute dystonia is a recognized side effect.
d - clozapine is a subtype of antipsychotics.
e - they reduce the level of prolactin.
43 - MOOD STABILIZERS: a - include sodium valproate.
b - accepted carbamazapine blood level is 0.6 - 1.2ml-l.
c - fine tremor is a sign of lithium toxicity.
d - lithium may lead to hyperthyroidism.
e - lithium is teratogenic.
44 - BENZODIAZEPINES: a - have a good sedative effect.
b - risk of dependence is more with long acting benzodiazepines.
c - withdrawal symptoms include seizure.
d - ataxia is a side effect.
e - are used in the treatment of delirium tremens.
45 - E.C.T. : a - usually done under local anesthesia.
b - indicated for depressive stupor.
c - indicated for resistant mania.
d - cardiac infraction is an absolute contraindication.
e - it is a hazardous procedure.
PSYCHIATRIC EMERGENCY
46 - SUICIDE:
- 57
a - common causes include depression and alcoholism.
b - presence of a serious physical illness is a risk factor.
c - could occur in delirious patient.
d - more common among old males.
e - hospitalization is essential.
47 - VIOLENCE: a - could be due to hypoglycemic attack.
b - major depression is a known cause.
c - confrontation is required to control the patient.
d - haloperidol IM gives good results.
e - amphetamine intoxication should be excluded.
48 - DELIBRATE SELF-HARM: a - common in borderline personality disorder.
b - occurs more in young females.
c - drug overdose is common.
d - is usually well planned.
e - sometimes ends by death.
- 58
PSYCHOLOGICAL TREATMENT
49 - BEHAVIOUR THERAPY: a - is based on experimental psychology.
b - includes relaxation training.
c - exposure is effective in agoraphobia.
d - aims to change the maladaptive ways of thinking.
e - could be used in schizophrenic patients.
50 - CONGNITIVE THERAPY: a - aims to correct maladaptive behavior then thinking.
b - used in schizophrenia.
c - gives good results with mildly depressed patients.
d - depends on psychoanalysis.
e - used in anxiety.
- 59
ANSWERS - MCQs
[1] a - (T) b - (T) c - (T) d - (F) e - (T)
[2] a - (F) b - (T) c - (F) d - (F) e - (F)
[3] a - (F) b - (F) c - (T) d - (T) e - (F)
[4] a - (T) b - (T) c - (F) d - (F) e - (F)
[5] a - (T) b - (T) c - (T) d - (T) e - (T)
[6] a - (T) b - (T) c - (F) d - (F) e - (F)
[7] a - (T) b - (F) c - (T) d - (T) e - (T)
[8] a - (F) b - (T) c - (F) d - (T) e - (T)
[9] a - (T) b - (T) c - (T) d - (T) e - (T)
[10] a - (F) b - (T) c - (F) d - (T) e - (F)
[11] a - (F) b - (T) c - (T) d - (F) e - (T)
[12] a - (F) b - (T) c - (F) d - (T) e - (T)
[13] a - (F) b - (T) c - (T) d - (T) e - (T)
[14] a - (T) b - (T) c - (T) d - (T) e - (T)
[15] a - (T) b - (T) c - (T) d - (T) e - (T)
[16] a - (T) b - (F) c - (T) d - (T) e - (F)
[17] a - (T) b - (T) c - (T) d - (T) e - (T)
[18] a - (T) b - (T) c - (T) d - (F) e - (F)
[19] a - (T) b - (T) c - (T) d - (T) e - (T)
[20] a - (F) b - (F) c - (T) d - (T) e - (F)
[21] a - (F) b - (T) c - (T) d - (T) e - (F)
[22] a - (F) b - (T) c - (T) d - (T) e - (T)
[23] a - (T) b - (F) c - (F) d - (T) e - (F)
[24] a - (T) b - (T) c - (F) d - (T) e - (T)
[25] a - (T) b - (T) c - (T) d - (T) e - (T)
[26] a - (T) b - (F) c - (T) d - (F) e - (F)
[27] a - (F) b - (F) c - (F) d - (F) e - (T)
[28] a - (T) b - (F) c - (F) d - (F) e - (F)
[29] a - (T) b - (F) c - (F) d - (F) e - (T)
[30] a - (T) b - (T) c - (T) d - (T) e - (T)
[31] a - (T) b - (F) c - (F) d - (F) e - (T)
[32] a - (T) b - (T) c - (T) d - (T) e - (T)
[33] a - (T) b - (T) c - (F) d - (T) e - (F)
[34] a - (F) b - (F) c - (T) d - (F) e - (F)
- 60
[35] a - (T) b - (F) c - (F) d - (F) e - (F)
[36] a - (F) b - (T) c - (T) d - (F) e - (T)
[37] a - (T) b - (T) c - (T) d - (T) e - (T)
[38] a - (F) b - (F) c - (F) d - (F) e - (T)
[39] a - (F) b - (F) c - (T) d - (T) e - (T)
[40] a - (T) b - (T) c - (T) d - (T) e - (F)
[41] a - (F) b - (T) c - (T) d - (T) e - (F)
[42] a - (T) b - (T) c - (T) d - (T) e - (F)
[43] a - (T) b - (F) c - (F) d - (T) e - (T)
[44] a - (T) b - (F) c - (T) d - (T) e - (T)
[45] a - (F) b - (T) c - (T) d - (F) e - (F)
[46] a - (T) b - (T) c - (T) d - (T) e - (T)
[47] a - (T) b - (T) c - (F) d - (T) e - (T)
[48] a - (T) b - (T) c - (T) d - (F) e - (T)
[49] a - (T) b - (T) c - (T) d - (F) e - (T)
[50] a - (F) b - (F) c - (T) d - (F) e - (T)
- 61
SECTION - C
CASES
Do not forget full physical assessment
- 62
- 63
CASE - 1
Salim is 59 year-old in-patient Saudi male, known case of DM and CCF for the last 13 years, referred by his Chest Physician with 3 days history of disturbed behavior shouting, agitation and fearfulness.
Q. 1: What is the most likely diagnosis?
A: Acute organic brain syndrome (delirium).
Q. 2: What is the most important feature you should look for?
A: Disturbance of consciousness.
Q. 3: What are the most likely causes of his delirium?
A: Those related to his medical illness: hypoxemia - hypoglycemia - electrolyte disturbances and side effects of his medicines.
Q. 4: Would you treat him in a psychiatric ward?
A: No, he should be treated in a medical ward because his psychiatric problem is due to medical illnesses. and needs medical care.
Q. 5: What about the prognosis?
A: 1 - Short-term prognosis is good, he is expected to improve within days after treating his acute medical problem.
2 - Long-term prognosis: he is expected to have another similar episodes whenever his medical condition deteriorates.
- 64
CASE - 2
Ayisha is 75 year-old Kuwaiti lady brought to outpatient psychiatric clinic by her concerned son with the following: increasing forgetfulness, always keeps talking about her adulthood and very remote events. She also became more rigid and tough even towards strangers. That is for two years.
Q. 1: What is the most likely diagnosis?
A: Chronic organic brain syndrome (dementia).
Q. 2: How would you proceed with this case?
A: + Further assessment: * obtaining full history
* physical examination
* baseline investigations.
+ Exclusion of functional psychiatric disorders e.g. depression.
+ Looking for treatable causes e.g. low B12.
+ Psychological treatments including.
a - supportive therapy with the help of the family.
b - repeated orientation, memory aids.....
+ Social treatment: a - respect and tolerate the patient with her deficits.
b - encourage social contacts, self-care.
+ Symptomatic drug treatment:
- small doses of thioridazine e.g. 10MG nocte (at night).
+ Support for relatives.
Q. 3: What about the long term prognosis?
A: It depends on the cause, if it is non-treatable e.g. degenerative disease. The prognosis would be poor.
CASE - 3
Ali is 29 year-old accountant, referred by a medical team to the psychiatric clinic with 6 months history of recurrent bouts of sudden extreme fear accompanied by sweating, shortness of breath, palpitation and dizziness. His physical assessment showed no abnormality. Recently he started to have anxiety features in open places like markets.
Q. 1: What is your differential diagnosis?
A: 1 - Panic disorder with agoraphobia.
2 - Generalized anxiety disorder.
- 65
3 - Endocrinopathies e.g. hyperthyroidism.
4 - Psychoactive substance abuse.
Q. 2: How would you manage this patient?
A: 1 - Reassurance and explanation.
2 - Further assessment to clarify the diagnosis and to exclude possible medical causes.
3 - Pharmacological treatment of his anxiety features * short term anxiolytics or
* divided doses of antidepressants.
4 - Supportive psychotherapy.
5 - Behavioral therapy.
Q. 3: Do you think that Beta - blockers would help in blocking panic attacks?
A: No, they are not useful in blocking panic attacks but may enhance the response to behavioral therapy for phobia by reducing the peripheral manifestations of anxiety.
- 66
CASE - 4
Asma is 30 year-old Saudi lady working as teacher, mother of 5 children referred to
Psychiatric clinic by primary care physician with 3 years history of: always being tense and worried, watchful feeling, tension headache dizziness and palpitation.
Q. 1: What is the most likely diagnosis?
A: Generalized anxiety disorder.
Q. 2: What medical conditions that could give such a picture?
A: 1 - Hyperthyroidism
2 - Pheochromocyctoma
3 - Hypoglycemia.
Q. 3: How would you treat her?
A: 1 - Reassurance and explanation about her unrealistic fear.
2 - Relaxation training.
3 - Reducing current stresses.
4 - Psychotropic drugs:
a - short-term (few weeks) small doses of benzodiazepines e.g. Lorazepam
0.5mg tds.
b - small divided doses of tricyclic antidepressents e.g. Imipramine 10mg tds.
c - B-blockers (e.g. Propranalol 20mg tds) to control some of autonomic symptoms like palpitation.
- 67
CASE - 5
Khlaid is 27 year-old single man, works as a teacher, presented with 5 years history of feeling tense and anxious in social situations. During delivering a lecture he experiences mouth dryness, palpitation and shaking limbs.
Q. 1: What is the most likely diagnosis?
A: Social phobia.
Q. 2: What are other Psychiatric problems he may also have?
A: 1 - Depression.
2 - Avoidant personality.
3 - Other anxiety disorder e.g. agoraphobia.
Q. 3: What are the drugs used to treat social phobia?
A: 1 - MAOI particularly phenelzine and tranylcypromine * “moclobemide” a new
MAOI-A reversible - very safe.
2 - Beta-blockers are effective to control physical features.
3 - Alprazolam (benzodiazepine) has been found to be good but there is a high risk of dependence.
4 - Tricyclic antidepressants are found to be effective.
- 68
CASE - 6
Huda is 22 year-0ld Saudi female, student presented with history of being increasingly preoccupied with thoughts that she can not dispel. She spends hours each night ruminating about the days events, especially interactions with friends. Showering, combing her hair and putting on her clothes, all demand perfectionism.
Q. 1: What is your diagnosis?
A: Obsessive compulsive disorder.
Q. 2: What are other Psychiatric problems she may also have?
A: 1 - Depression.
2 - Obsessive compulsive personality.
3 - Anxiety.
Q. 3: How would you treat her?
A: 1 - Antiobsessional drugs like clomipramine, fluoxetine or fluvoxamine.
2 - Behavioral therapy: response prevention & thought stopping.
3 - Supportive psychotherapy.
4 - Social: involving other family members to help the patient.
Q. 4: What about the prognosis?
* Two thirds of cases improve by the end of one year
* Cases lasting more than one year usually run a fluctuating course, with periods of partial or complete remission lasting a few months to several years.
* Poor prognosis is associated with:
1 - Obsessive compulsive personality traits.
2 - Prolonged course with severe symptoms.
3 - Continuing stressful events in patient’s life.
CASE - 7
Saleh 32 year-old male primary school graduate works as a governmental employee came to Psychiatric clinic with 4 years history of low self-esteem, lack of initiative, chronic fatigue and social withdrawal.
Q. 1: What is your differential diagnosis?
A: 1 – Dysthymic disorder(chronic mild depression).
2 - Major depression.
3 - Depression due to organic causes.
4 - Substance abuse.
- 69
Q. 2: What further history do you need to clarify the diagnosis?
A: 1 - Biological features of depression especially early morning wakening.
2 - Death wishes and suicidal thoughts.
3 - Presence of a medical illness / drugs treatment e.g. antihypertensive medications.
Q. 3: How would you treat him? (a case of dysthymic disorder)
A: 1 - Psychological:
a - supporting psychotherapy.
b - cognitive - behavior therapy: to correct cognitive distortions.
c - interpersonal psychotherapy.
2 - Pharmacological:
* MAOI may be more beneficial than TCA.
* SSRI (e.g. fluoxetine) found to be effective.
Q. 4: Would you hospitalize this patient?
A: No, hospitalization is usually not indicated for dysthymic disorder; however when the condition is severe or when there is a need for extensive diagnostic procedures hospitalization is indicated.
CASE - 8
Ibrahim is 45 year-old Saudi businessman, referred to Psychiatric clinic by medical team with overconcern about his physical health particularly his liver functions.
Physical examination and laboratory investigations revealed no abnormality.
Q. 1: What is the most likely diagnosis?
A: Hypochondriasis.
Q. 2: What other psychiatric problems he may also have?
A: 1 - Depression.
2 - Anxiety.
Q. 3: At what medical specialty hypochondrical patients are seen more?
A: 1 - Gastroenterology.
2 - Cardiology.
3 - Neurology.
4 - Rheumatology.
Q. 4: What factors appear to predispose one to develop “Illness behavior”?
A: 1 - Culture, certain cultures, appear to be more accepting of illness than others.
- 70
2 - Inadequate social support system.
3 - Low self-reliance.
4 - Life stress.
5 - Psychological resolution (illness behavior is more likely when it can resolve psychological problems e.g. reducing blame for failure.
- 71
CASE - 9
Jawaher is 25 year-old lady, divorced 5 weeks ago presented to the out-patient psychiatric clinic with one week history of anxiety, worry, low mood, fearfulness. Her functional capacity as a teacher is impaired by her psychological problem.
Q. 1: What is your differential diagnosis?
A: 1 - adjustment disorder.
2 - major depressive episode.
3 - anxiety.
4 - non pathological reaction to stress.
Q. 2: Would you consider the diagnosis of post-traumatic stress disorder?
A: No, in post-traumatic stress disorder psychological stressor determines diagnosis. Stressor is outside the range of normal human experience. e.g. war, rape, floods, mass catastrophe.
Q. 3: What about the course and prognosis of adjustment disorders?
A: Most symptoms diminish overtime without treatment, especially after stressor is removed; subgroup maintains chronic course with risk of secondary depression, anxiety & psychoactive substance abuse.
Q. 4: How would you treat her?
A: 1 - Psychological treatment is the treatment of choice.
* provide support
* encourage alternative ways of coping.
* offer empathy.
2 - Pharmacological - short-term benzodiazepines.
- 72
- 73
REFERENCES:
1 - SYNOPSIS OF PSYCHIATRY: Kaplan - Sadock - Grebb (1994).
2 - OXFORD TEXTBOOK OF PSYCHIATRY: Gelder - Gath - Mayou (1993).
3 - CONCISE OXFORD TEXTBOOK OF PSYCHIATRY: Gelder - Gath - Mayou
(1994).
4 - BASIC NOTES IN PSYCHIATRY: M. Levi (1989).
5 - DIAGNOSTIC AND STASTICAL MANUAL OF MENTAL DISORDERS - DSM IV
(1994).
6 - POSTGRADUATE PSYCHIATRY: Appleby - Forshaw (1990).
7 - COMPANION TO PSYCHIATRIC STUDIES: Kendell - Zeally (1993).
8 - PSYCHIATRIC SECRETS: Jacobson - Jacobson (1996).
9 - PSYCHIATRY DIAGNOSIS AND THERAPY: Faherty - davis (1988).
10 - THE CLINICAL PROCESS IN PSYCHIATRY: Nurcombe - Gallagher (1986).
11 - EMERGENCY PSYCHIATRY FOR THE HOUSE OFFICER: Fauman (1983).
12 - CASE STUDIES IN PSYCHIATRY: David Tomb (1987).
13 - EXAMINATION NOTES IN PSYCHIATRY: J. Bird (1987).
14 - PSYCHIATRIC DIFFERENTIAL DIAGNOSIS: J. Pfeffer (1987).
15 - PSYCHIATRY A PROBLEM-ORIENTED APPROACH: H. Moffic (1988).
16 - CASE HISTORIES IN PSYCHIATRY: E. Fottrell (1983).
17 - CASE PRESENTATIONS IN PSYCHIATRY: D. Bhugra (1993).
- 74
©
Mohammed Abdullah Al-Sughayir, 1996
King Fahd National Liabrary Cataloging-in-Publication Data
Al-Sughayir, Mohammed Abdullah
Rapid review of psychiatric disorders - Riyadh
...... p. , ..... cm
ISBN: 9960-02-238-0
1- Mental illness
616.891 dc
I- Title 2- Psychiatry
0195/17
Legal Deposit no. 0195/17
ISBN: 9960-02-238-0
ىلولأا ةعبطلا
م 1996 ـ ـه 1417
فلؤملل ةظوفحم عبطلا قوقح
- 75