Bacterial Vaginosis - the NHS Tayside Sexual Health and Wellbeing
advertisement

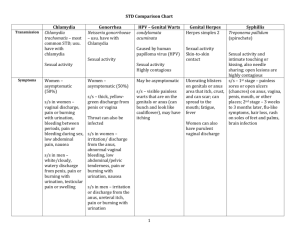
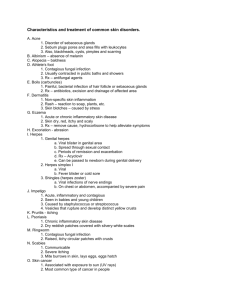
Contents Page No 1. General points & who to refer to the Sexual Health Clinic (SHC) previously known as GUM. 2 2. Taking a sexual history 3 3. Which tests to take? 3 4. 4 Causes of Vaginal Discharge Management of Specific Causes of Vaginal Discharge Bacterial vaginosis Trichomonas Vaginalis Candida albicans Chlamydia trachomatis Neisseria gonorrhoea 12 Causes of Male Urethral Discharge & Dysuria Management of specific causes of Male Urethral Discharge & Dysuria Non- gonococcal urethritis Chlamydia trachomatis Neisseria gonorrhoea Herpes Simplex Virus 13 Causes of Genital Ulceration Management of specific causes of genital ulceration Herpes Simplex Syphilis 7. Balanitis 16 8. Vulval skin problems 16 9. Causes of Genital Lumps Management of Genital Warts 18 5. 6. Further information: See www.doctors.net.uk for excellent online courses on sexual health and sexual history taking. See www.bashh.org for guidelines on the management of all STIs. Qualifying Statement The authors have taken all possible care to ensure that these guidelines are accurate and that the correct dosages and routes of medication have been given. However, it remains the responsibility of the prescribing clinician to ensure the accuracy and appropriateness of the advice given. As with all guidelines, they do change with time but it is planned to regularly update them. 1. General Points & Who to refer to GUM Please refer any patients who wish an asymptomatic screen to a sexual health clinic. The waiting time for an appointment at any of the clinics in Tayside is around one week at present. Patients can also attend a walk-in clinic. These run every afternoon in the SHC at Ninewells and on a Monday and Thursday morning at the SHC at Perth Royal Infirmary. Please return to the home page of this website for further information about this service. Symptomatic patients can be referred via the GP direct- access phone line on 01382 425533, or the patient can refer themselves on 01382 425542. These numbers are for the SHC at Ninewells Hospital which is open Monday to Friday. If the patient wants to be seen in Perth or Arbroath please see the relevant pages on this website for contact information. Please send a brief letter with the patient if you want information for your records. We do not see patients with genital warts urgently, and only need to see these patients if they wish to have a full STI screen. We know that 20% of patients presenting with warts will have another STI. First line treatment for genital warts is Podophyllotoxin (Warticon) cream for women or perianal warts in either sex and Podophyllotoxin (Warticon) paint for men with penile warts. These treatments should not be used in pregnancy. Patients should be advised that the treatment can take up to 12 weeks to work. Smokers should be advised that they may take longer to clear their warts than nonsmokers. HIV testing is routinely offered to all patients attending a SHC. Only those patients who are felt to be at ‘high risk’ of infection are offered accelerated HIV testing. ‘Low risk’ patients will be asked to phone for their results 2 weeks after their appointment. Patients who have been screened in the community and are found to have an STI should be referred to GUM for partner notification. We are in the process of setting up a service to provide partner notification to patients diagnosed with an STI out with the sexual health services. Once our plans are finalised we will send you more information on this development. A Young Persons Clinic runs in the SHC at Ninewells on a Thursday afternoon from 1.30pm. This clinic is aimed at 12-18 year olds, and offers screening for STIs, together with contraception while assessing any child protection issues. Appointments can be made on 01382 632600. However, the clinic also runs as a walk-in and patients who arrive between 1.30 and 4.00 will be seen that day. Genital Skin Problems Women with genital skin problems can be referred to the Joint Vulval Skin Clinic which is based in The Sexual Health Clinic at Ninewells. Referral should be made by letter in the normal way. There is a significant waiting list for this clinic at present. We are however able to triage urgent patients so if this is the case please indicate this on the referral letter. Male patients with genital skin problems are seen in the routine SHC, for which there is no waiting list. 2 2. Taking a sexual history in Primary Care A sexual history in Primary Care does not have to be as detailed as one taken in a SHC setting. As with any history it is good practice to observe the following: 3. Ensure privacy at all times Explain why you are asking such detailed questions Remind the client that these are questions we ask everyone who may have a problem which may be related to sex Only ask relevant questions It is good practice to enquire about the number of sexual partners in the previous 6 months as this will help with partner notification, should the patient be diagnosed with an STI. Which tests to take in Primary Care? The following is a guide to tests which can be taken in Primary Care as part of a sexual health screen. Asymptomatic Female Endocervical swab for N. gonorrhoea (black charcoal) Endocervical swab or a vulvo-vaginal swab for Chlamydia trachomatis +/- Syphilis serology and HIV antibody screening Symptomatic Female As for Asymptomatic female but include: High Vaginal swab (charcoal) this is to look for pathogens which can cause a vaginal discharge eg. Candida sp., Bacterial vaginosis, Trichomonas vaginalis and Streptococci pH – the normal vaginal pH is 3.5-4.5. It can be useful to put a sample of the discharge on a piece of pH paper at the time of swab taking. Bacterial vaginosis and vaginal Trichomonas are associated with a high pH >5. However seminal fluid and blood will also increase the vaginal pH. A quicker diagnosis may be reached by doing microscopy and if this is required it would be appropriate to refer the patient to a SHC. Asymptomatic Heterosexual Male (preferably patient has not PU’d for >1 hour) Urethral swab for N. gonorrhoea (charcoal) First Void urine for Chlamydia trachomatis +/- Syphilis serology and HIV antibody testing Symptomatic Heterosexual Male As for asymptomatic male. However, a quicker diagnosis may be reached by doing microscopy and if this is required it would be appropriate to refer this patient to a SHC. It is not possible to diagnose Non-gonococcal urethritis (NGU) outside the SHC setting. 3 Men who have sex with men (MSM) The same tests should be taken as outlined for a Heterosexual male but the following tests should be added: Throat swab (charcoal) for N. gonorrhoea Rectal swab for Chlamydia trachomatis Rectal swab for N. gonorrhoea (charcoal) Check Hepatitis B core antibody to look for evidence of previous infection. If non-immune, vaccinate. Check Hepatitis A IgG and if no evidence of previous immunity or history of prior vaccination, offer to vaccinate. 4. Causes of vaginal discharge Vaginal discharge is a common presenting symptom in Primary Care. A sexual history should be taken and a sexual health screen offered if the history dictates. Those at highest risk of having a sexually transmitted infection are all sexually active women aged under 25 and women over 25 who have had a recent change of sexual partner or who have had more than one sexual partner in the last year. –see SIGN guidelines for further information. The most common cause of vaginal discharge is Bacterial vaginosis. The list below outlines causes of Vaginal discharge and these should be considered when a patient attends complaining of a vaginal discharge. Bacterial vaginosis Candidiasis Trichomonas vaginalis Neisseria gonorrhoea Chlamydia trachomatis HSV Foreign body e.g. retained tampon Physiological Cervical cancer Fistula Bacterial Vaginosis Most common cause of vaginal discharge. Caused by overgrowth of Gardnerella vaginalis, Mobilluncus and other anaerobic organisms. It is not an STI Signs Malodourous vaginal discharge, often worse after sexual intercourse Doesn’t usually cause itching or discomfort Investigations 4 HVS pH - >4.5 Treatment Metronidazole 400mg BD for 1 week or 2G stat (the stat dose should not be used in pregnancy) Clindamycin 300mg BD for 7 days Points to tell the patient Not an STI Partners do not need treatment Recurrences can be brought on by menstruation and sexual intercourse due to the fact that sperm and blood increase the vaginal pH (condoms can help reduce recurrences), and overwashing. Associated with the IUCD, smoking, Black ethnicity To prevent recurrences: Consider removal of the IUCD Consider using a method of contraception which decreases the frequency of menstruation e.g. Depo provera Use of condoms prevent sperm causing alkaline pH in vagina and therefore reduces recurrences Consider referral to a SHC for management of patients with recurrent BV. Trichomonas vaginalis Very uncommon diagnosis Signs/symptoms Malodourous, itchy vaginal discharge Superficial dyspareunia Vaginitis Abdominal pain Investigations HVS (black charcoal swab) pH – >4.5 Treatment 5 Metronidazole 400mg BD or 2G stat (do not use the stat dose in pregnancy) Important points Must have Test of Cure (TOC) 1-2 weeks following treatment Metronidazole resistance not uncommon, but consider reinfection also. – refer to SHC. Partner notification required. Male partners need treatment. If a Cervical smear is reported as showing Trichomonas like organisms, this is not sufficient to make a diagnosis of TV. A black charcoal HVS should be sent for confirmation before making this diagnosis. Candida (Thrush) Most cases are caused by Candida albicans but need to consider other Candida sp. if patient appears to be resistant to treatment. Signs/symptoms Itchy, white vaginal discharge Superficial dyspareunia Vulval oedema Vulval erythema Investigations HVS – Black charcoal swab pH – usually normal (3 -4) Urinalysis – exclude diabetes Treatment Clotrimazole pessary 500mg stat PV Clotrimazole 10% VC PV Fluconazole 150mg stat (do not use in pregnancy) Important points Partners do not usually need treatment No benefit of yeast free diets Use of a soap substitute and exclusion of perfumed washing products is important. Please see the vulval skin section. 6 Recurrent candidiasis – refer to SHC after giving the patient information about the exclusion of all perfumed washing products, fabric softners and baby wipes. See vulval skin section for patient information leaflet on this. Chlamydia Trachomatis Who to test for Chlamydia? Tayside has the highest rates of Chlamydia infection in those under 25 in Scotland, with 22% of young men and 14% of young women being infected. (2005 figures) In Scotland as a whole, though the highest rates of infection are in the under 25 population, over half the tests for Chlamydia are performed in those over 25. Despite young men having the highest rates of infection, the majority of tests are performed in women. The majority of male testing occurs in SHC when men attend because they have symptoms or are asked to attend as contacts of Chlamydia. Targeting of Chlamydia screening to the most appropriate population groups is required . Those who should be targeted for screening include: All sexually active men and women under the age of 25 Individuals with a new sexual partner Individuals who have had more than one sexual partner in the last year. Individuals who require testing for Chlamydia include: Those with symptoms –see below Infants with conjunctivitis and pneumonitis, and if found to be positive for Chlamydia their parents. Sexual contacts of a Chlamydia positive individual. Once infected with Chlamydia the infection can persist or resolve spontaneously. Two thirds of the sexual partners of Chlamydia positive individuals are also Chlamydia positive. Symptoms and Signs Women: o 70% Asymptomatic o Post coital or intermenstrual bleeding (always think about the possibility of Chlamydia) o Vaginal discharge o New lower abdominal pain o Deep dyspareunia o Dysuria (sterile pyuria can be caused by Chlamydia) o Cervicitis and contact bleeding Men: o 50% Asymptomatic 7 o Urethral discharge o Dysuria Note: Pharyngeal Chlamydia is usually asymptomatic. Rectal Chlamydia may be asymptomatic but may cause rectal discharge and discomfort. Over the last few years there has been an increase in the number of cases of Lymphogranuloma venereum (LGV) which is caused by a different serovar of Chlamydia trachomatis. This infection is found mainly amongst men who have sex with men (MSM), many of whom are HIV positive. It presents as a severe proctitis or genital ulceration with prominent inguinal lymphadenopathy. For this reason if a rectal sample is found to be positive for Chlamydia, the sample should be sent to the LGV Reference Laboratory in Edinburgh, by the Microbiology Department in Ninewells. Therefore, if your patient has significant rectal symptoms please alert the laboratory to this by noting this on the microbiology form. Complications of Chlamydia Some women who have Chlamydia will develop Pelvic Inflammatory Disease (PID) o Many will have no or only mild symptoms. o The risk of developing PID increases with each recurrence of Chlamydia. Epididimo-orchitis Adult conjunctivitis Neonatal conjunctivitis and pneumonitis Sexually acquired reactive arthritis Investigations A nucleic acid amplification test (NAAT) is used in Tayside to test for Chlamydia. Women: An endocervical swab is the preferred method for testing in women. The test requires endocervical columnar cells so the swab should be inserted into the cervical os and rotated firmly against the walls of the endocervix. A vulvo-vaginal swab can be performed by the clinician without a speculum or be self-taken by the patient. A first voided urine sample. Men: A first voided urine sample. Recent research would suggest that urine does not require to be held for a fixed length of time prior to providing a urine sample. A urethral swab if the patient is unable to pass urine. What to do with a positive result? The microbiology lab will contact you if your patient has a positive Chlamydia result. 8 There are two options: 1. You treat your patient and ask them not to have any sexual contact until their partner has also been treated. They should wait 7 days after taking Azithromycin. Please then refer to for partner notification and screening for other STIs. A health advisor from SHC will contact the patient by phone (mobile number preferred) to ensure that the patient has been treated for chlamydia and has not been reinfected. Screening for other sexually transmitted infections in the SHC will be offered. Many patients particularly if they are asymptomatic decline further testing and therefore do not attend the SHC. Partner notification can be arranged over the phone. Patients must be made aware that a health advisor will contact them, but that they do not necessarily need to attend the clinic. 2. If you feel that your patient needs to be seen in the SHC, for whatever reason (often if there is concern as to whether they will abstain from sexual intercourse until after their partner is treated) then do not treat. We will see them in GUM within 48 hours of your referral. We will ask them to attend with their partner so that they can be treated together. Patients can be referred direct to a health advisor at Ninewells 5 days per week on 01382 632600 Treatment Indications for therapy: A positive Chlamydia PCR test On epidemiological grounds if a recent sexual partner has confirmed Chlamydia infection. (But such an individual also requires to be tested for Chlamydia to allow ongoing contact tracing.) Uncomplicated infection of the Pharynx, Genitalia and Rectum. Azithromycin 1g single dose orally (preferably on a empty stomach) OR Doxycycline 100mg twice daily orally for 7 days OR Ofloxacin 400mg once daily for 7 days. Pregnant patients. Azithromycin 1G stat OR Erythromycin 500 mg twice daily orally for 14 days OR Erythromycin 500mg qds. for 7 days 9 Azithromycin is not licensed for use in pregnancy; however there is no indication that any adverse events have been caused by the drug when it has been used in this situation. The WHO advocates the use of Azithromycin in pregnancy. Up to 25% of patients (non pregnant) who take Erythromycin fail to complete the course due to side effects. Untreated chlamydial infection in pregnancy can result in preterm birth, IUGR, neonatal conjunctivitis and pneumonitis. For the above reasons a pregnant patient who has been diagnosed with Chlamydia should be offered treatment with all of the above regimens. She needs to be told that Azithromycin is an unlicensed treatment for Chlamydia in pregnancy. Ultimately it is the patient’s decision as to which drug regime she wishes to take. Whichever treatment course is chosen, a test of cure (TOC) should be performed three weeks or more after completing treatment. All Chlamydia Positive Patients: Should be advised to abstain from all sexual intercourse (oral, genital and anal sex and even sex with a condom) for seven days after being treated with Azithromycin, or until they have completed their treatment course with another antibiotic. All patients who are found to have Chlamydia should be offered a screen for other sexually transmitted diseases and should be encouraged to have an HIV test. Complicated infection Males Epididymo-orchitis Treatment: Ofloxacin 400mg twice daily orally for 14 days Females Pelvic Inflammatory Disease Treatment: Ofloxacin 400 mg twice daily orally for 14 days AND Metronidazole 400 mg twice daily orally for 10-14 days OR Doxycycline 100mg twice daily orally for 14 days AND Metronidazole 400mg twice daily orally for 10-14 days Chlamydial conjunctivitis Adults Treatment: As for uncomplicated chlamydia infection 10 Ofloxacin eye drops can be considered Neonates Erythromycin syrup orally Neonatal infection results in infection of the conjunctivae and nasopharynx and therefore systemic treatment is required. Follow up: Contact tracing In asymptomatic patients the look back period is 6 months or the last sexual partner if this time period is longer. If a man presents with symptoms of urethritis, partner notification should include all sexual partners from the previous 4 weeks. Patients should be advised to have no sexual contact (oral, genital or anal) even with a condom until both they and their partner(s) have completed treatment. The patient must wait 7 days after treatment with Azithromycin or until they have completed a 7 day course of treatment with another antibiotic. Epidemiological treatment of partners. All patients should be followed up to check compliance with antibiotic therapy and to make sure that there is no risk of re-infection from an untreated partner. It may be appropriate to do this by phone in the majority of patients, as they would not otherwise be required to come back to the clinic. Routine test of cure (TOC) is not necessary in all patients. The following patients should have a test of cure (urine or endocervical swab) no sooner that 3 weeks after completion of antibiotic therapy: o Patients who remain symptomatic o Pregnant women o Patients who may be re-infected or who have not complied with antibiotic therapy (should be re-treated as well as re-tested) o Patients who request a TOC o Patients not treated with optimal antibiotic therapy, such as Erythromycin Neisseria Gonorrhoea Who to screen: Men with a urethral discharge Women with a vaginal discharge, Bartholin’s abscess Heterosexual men, MSM and females who are asymptomatic but request a full STI screen Male and female contacts of Gonorrhoea. Which test: Heterosexual man o Urethral swab. MSM o Urethral, rectal and throat swab. Women 11 o Urethral and endocervical swab. A standard black charcoal bacteriology swab should be used. The swab needs to get to the laboratory to be plated out onto special medium and then placed in a CO2 incubator within six hours of being taken. If this is not possible (eg. Friday afternoon), the discharge from the urethra or endocervix can be placed on a slide and air dried, before being placed in a slide carrier for transport to the lab. Please write the patients details onto the slide. The slide can then be Gram stained in the lab and viewed. A culture swab should also be sent, and if negative can be repeated at a later date depending on the microscopy result. Treatment: Cefixime 400mgs stat Partner Notification: A full sexual history must be taken to allow appropriate contact tracing. Patients will often not attend the sexual health clinic (SHC) if they have already been treated and therefore it is often easier for us if you do not treat the patient but ask them to attend the SHC. If you contact a health advisor with your patients details she will contact them (provided the patient is aware that this will happen) which allows us to undertake partner notification and to arrange treatment that day or the following day (depending on the time patient is referred). Please phone 01382 632600. (direct line) Approximately 50% of sexual partners will also be infected and therefore we will usually treat partners epidemiologically depending on the circumstances. All partners need to be tested for infection even if epidemiologically treated. Between 25% and 50% of patients who have Gonorrhoea will be co-infected with Chlamydia. If the Chlamydia result is negative the patient does not require treatment, but if the result is not available/unknown it is worth adding Azithromycin 1G stat. All patients who are found to have a sexually transmitted infection, such as Gonorrhoea, should be tested for HIV and Syphilis. 5. Male dysuria/discharge Chlamydia trachomatis Neisseria gonorrhoea Non-gonococcal urethritis HSV UTI Chemicals Urethral stricture Non-Gonococcal Urethritis (NGU) This diagnosis is made at microscopy and therefore can only occur in the SHC setting. Testing for NGU is now only undertaken in SYMPTOMATIC males. A urethral swab from a male patient is smeared onto a glass slide, fixed using heat and then Gram stained. At microscopy, if there are >5 polymorphonuclear leucocytes 12 (PMNL) per high power field, a diagnosis of Non-Gonococcal Urethritis (NGU) is made. This diagnosis only affects men but female partners should be epidemiologically treated. NGU is the new name for Non-Specific Urethritis (NSU). Urethitis is most commonly caused by chlamydia and therefore treatment is with standard Chlamydia therapy. However a number of patients with NGU will be Chlamydia negative and therefore the urethritis may be caused by another organism such as Mycoplasma or Ureaplasma. At present there are no routine tests available for genital strains of these organisms in our laboratory. Therefore, often we will not know exactly what organism caused the infection. Treatment Treat as for Chlamydia trachomatis infection with 1g Azithromycin stat OR Doxycycline 100mgs bd for 7 days Partner notification - refer to HA Avoid SI for 1 week after treatment and until partner has also been treated. Patients with recurrent NGU should be referred to the SHC. There we will ensure that the patient’s regular partner has been treated and offer treatment with Azithromycin 500mgs stat followed by Azithromycin 250mgs daily for a further 4 days AND Metronidazole 400mgs bd for 5 days 6. Genital ulceration The two main causes of genital ulceration in this country are Herpes Simplex and Syphilis (mainly in men who have sex with men) However a fuller list of causes of genital ulceration is given below. Genital herpes will be discussed in more detail. A high index of suspicion is needed for Syphilis. All patients who present with a genital sore should have syphilis serology checked, ESPECIALLY if they are men who have sex with men. If there is a possibility that a patient has syphilis they should be referred urgently to the SHC for further investigation and management. Please do not treat with antibiotics prior to referral. The management of syphilis is therefore not discussed here in any further detail. Causes of genital ulceration Herpes Simplex Virus (Types 1 & II) Syphilis Bechets disease Lympogranuloma Venereum LGV Fixed drug eruption Trauma Dermatoses Malignancy 13 Chancroid Donovanosis Herpes Zoster (Unilateral ulceration) Genital Herpes Simplex Virus Infection Genital Herpes infection is caused by Type 1 (>50% cases) and Type 2 Herpes simplex Virus (HSV). Clinically there is no way of telling which virus has caused the genital lesions but there are some important prognostic differences. Therefore anyone seen complaining of genital pain should be examined and a swab taken for HSV PCR. (green tube). This is worth doing even if you want your patient to be seen in GUM, as we will be able to access the result of your investigation, and once the patient is commenced on Aciclovir the test we take may be negative. Though many patients acquire HSV infection from a long term regular partner they should all be offered a screen for the other sexually transmitted infections. All patients with genital ulceration should as a minimum have syphilis serology performed, because of the increasing incidence of syphilis in the UK at present. The majority of individuals with HSV infection are asymptomatic- they do not suffer from oral or genital ulceration but they can intermittently shed herpes simplex virus from these sites, and infect their sexual partners. This is called asymptomatic shedding and occurs twice as frequently in HSV 2 than HSV 1 and occurs for longer periods in women than in men. Men are more likely to have asymptomatic carriage of HSV 2 which explains why women are more likely to acquire HSV 2 over time. It is uncommon for this to happen during casual sexual encounters therefore and is seen more frequently in longer term relationships. It is quite reasonable to reassure a patient who is in a long term relationship that developing an acute attack of primary herpes does not necessarily mean that their sexual partner has been unfaithful. Management of recurrent episodes of HSV Patients with recurrent episodes of infection should be reassured that they do not need to take antiviral treatment with each episode of ulceration. Often patients become unnecessarily stressed about the need to get to their GP or to the hospital to get Aciclovir, because they believe that the infection will not get better without taking treatment. Treatment is only effective if started during the prodrome or within 24 hours of lesions developing, and in this situation can shorten the duration of symptoms and viral shedding by a median of 1-2 days. However for many patients the length of each episode of ulceration is not altered by taking anti-virals, and the benefits of taking treatment are outweighed by the stigma of taking tablets. In a minority of cases, treatment started in the prodrome may avert the episode of ulceration. The application of Betadine Paint has been shown to be beneficial in the management of recurrent genital herpes. However it is important to be sure from the history and virology results that the patient is really suffering from HSV. It is common to see patients who believe they are getting recurrent attacks of herpes when in fact this is not the cause of their symptoms at all. Many patients who are seen in the SHC presenting for the management of their recurrent ‘HSV’ have never had a herpes culture/PCR to confirm their diagnosis and often do not have HSV at all but a genital dermatosis. Patients with recurrent symptoms of self described genital ulceration, but nothing to see on examination should be given a herpes swab kit (same bottle as Chlamydia) and asked 14 to take a self taken sample for herpes PCR as soon as ulcers appear. They then need to hand their sample in to your practice as soon as possible after being taken, to be sent to the lab. If this self taken swab is negative it makes the diagnosis of recurrent genital HSV very unlikely. Women with recurrent genital symptoms and a negative HSV virology swab can be referred to the Joint Vulval Skin Clinic. This is based in the SHC at Ninewells and runs twice per month. Type 1 Genital herpes will only cause recurrences in around 50% patients. It is unusual to see such patients in the SHC with troublesome recurrences. 90% of patients with Type 2 HSV will go on to have further recurrences. It is difficult to generalise in HSV infection but patients will often have frequent (monthly) recurrences within the first 6-12 months following infection. However if they are asked to keep a diary they will often notice that the gap between symptoms starts to lengthen from 6 months onwards, as the patients own immune system starts to control the infection. Modern management of recurrent HSV infection would suggest that it is better to defer Aciclovir suppressive therapy until at least a year after diagnosis to allow the individual’s own immune system to control the infection. Most patients are happy to do this when the reasons for this are explained. Herpes and Pregnancy All pregnant women who are known to have had HSV in the past should be advised to tell their midwife at booking. However most women in this group will be able to have a normal delivery without risk to the neonate. If they were to have an outbreak of HSV at the time of delivery some Obstetricians would offer them a Caesarian Section. In this case it is important that they are not examined vaginally and the membranes should obviously not be ruptured. If a women has her first attack of HSV during pregnancy she should be offered treatment with Aciclovir. There is no evidence that Aciclovir is harmful to the fetus. Depending on the stage of the pregnancy she may be offered an elective Caesarian Section as the mode of delivery. Type specific antibody testing. If a male partner suffers from recurrent HSV infection and his female partner is planning a pregnancy or is in fact pregnant it may be worth considering type specific antibody testing for the pregnant woman. This will give an indication as to whether the female partner already has antibody protection to HSV and is therefore at no ongoing risk, or infact has no antibody protection. In this situation the male partner may wish to consider HSV prophylaxis to reduce shedding of virus plus the use of condoms and avoidance of unprotected close genital contact once a pregnancy is achieved. Type specific antibody testing can also be used to test patients who believe that they are having severe recurrent attacks of HSV. >60% of individuals will have evidence of antibody to type 1 HSV but only around 20% of the UK population will have antibody to Type 2 HSV. If there is no evidence of antibody to type 2 HSV in a patient who complains of severe recurrent genital problems, herpes is probably not the cause of the symptoms. 15 This service is not offered routinely by the Microbiology department at Ninewells. However, samples can be sent to London for testing if it will benefit patient management. See patient information on website. 7. Balanitis This is inflammation of the glans penis. There are a number of different causes for this and these are listed below. Often the cause is not related to an STI. Causes of balanitis Candida albicans Streptococcal and Staphlococcal Infection Anaerobes Allergans/irritants Circinate balanitis Syphilis Herpes simplex virus Plasma cell (Zoon’s) balanitis Dermatoses e.g. Lichen sclerosis Penile intraepithelial neoplasia Trichomonas vaginalis Management: Investigations: Sub-preputial swab for bacterial culture and yeasts (Aimes) Microscopy for yeasts Urinalysis Sexual health screen to exclude syphilis, TV, HSV. Urinalysis to exclude glycosuria Biopsy may be required if an underlying dermatosis is suspected and symptoms do not settle with treatment. Treatment: Often simple measures such as salt-water bathing with the foreskin retracted twice a day is all that is required. For the longer term patients should be advised to avoid scented soaps and shower gels and to use soap substitutes instead. See genital skin washing advice. If the sub-preputial swab is positive for anaerobes, a course of metronidazole can be given, if the patient is still symptomatic after following the above measures. If the sub-preputial swab grows candida, this can be treated with 1% clotrimazole cream applied twice a day for 7 days, again if the patient is still symptomatic. Often subpreputial swabs will grow organisms which are commensals and if the patient becomes asymptomatic on the simple treatment measures above then no treatment is needed. If the balanitis doesn’t respond to simple measures or the lesions look suspicious, please refer to the SHC at Ninewells. A skin biopsy may be required. 8. Genital Skin Problems Genital skin problems are common and are often caused by washing with products which irritate the skin. 16 If your patient is complaining of genital itch, discomfort, cracking or tearing and there is no evidence of an underlying dermatosis on examination, it is worth giving them the following skin care information leaflet (see below). However also exclude glycosuria. If they fail to improve, after following all of the instructions on this leaflet for several months, then they should be offered specialist referral. Women should be referred to the combined vulval skin clinic at the Sexual Health Clinic (SHC) at Ninewells Hospital. Men can be referred to the SHC at Ninewells. Please mark the referral for Dr. Paterson. If you think that your patient does have a dermatosis please refer immediately to the appropriate clinic as mentioned above. GENITAL SKIN WASHING ADVICE (For patients) You have been diagnosed as having genital skin problems which are related to the use of perfumed washing products. This is an extremely common problem. The products that you use at present dry the skin out and cause cracks to develop which will cause itch and discomfort. Some creams will improve these symptoms in the short term but the skin will not get better until perfumed washing products are avoided. To ensure that your skin settles down we advise you to change the way you wash as outlined below. 1. Stop using the products that you presently use to wash your skin. Even simple soaps and products designed for babies, can irritate the skin, but using plain water can dry the skin out too much. It is therefore important to use a soap substitute. 2. Use a soap substitute to wash ALL of your body in the bath or shower. If you use a soap substitute to wash the genital skin but your normal soap on other parts of the body you will still get some of this soap product onto the genital skin and your skin problems will not improve completely. 3. You can buy soap substitutes from the sensitive skin counter at Boots. Look for: o Aveeno, o Oilatum, o Boots Own Brand. These brands produce products that can be used instead of soaps and shower gels. Alternatively the dispensary of the chemist will sell you: (these products can also be prescribed by your GP) o Diprobase Cream in a 500mls canister o Dermol 500 (Both products can be used to wash your body like a shower gel.) o Balneum Plus bath Oil is a suitable product for the bath, and is a good to use if the skin is very itchy as it will settle symptoms down quickly. It can make the bath very slippery so warn those who also use the bath. 17 Washing-up liquid is the best way to clean the bath after using Balneum Plus Bath Oil. 4. Never wash your hair in the bath. 5. Never put bubble baths, other perfumed products or essential oils into the bath water. 6. When washing hair in the shower do not stand under the shower, but put your head under the stream of water and keep your lower body out. 7. Do not use fabric softeners, even those marked as ‘sensitive’ when washing your clothes. Do not use 2 in 1 products such as Bold as these contain a fabric softener. The fabric softener stays on towels and underwear and will irritate the skin, and prevent it from settling. 8. Do not use baby wipes to clean the genital skin after going to the toilet. The alcohol in these products (even those marketed for sensitive skin) can harm the genital skin. It is better to use the Diprobase cream, or Dermol 500 (mentioned above) on some cotton wool for this purpose. 9. Coloured toilet tissue contains chemicals which can irritate the skin so always use white toilet roll. Do not use any creams on the genital area without discussing with staff in the clinic. 10. For women: Avoid feminine hygiene products. Avoid panty liners which are perfumed, look for low irritant sanitary and incontinence pads eg. Natracare. If you follow these guidelines closely for 3 to 4 months your symptoms should settle. If you continue to have problems with the genital skin, ensure that you have excluded all perfumed washing products and have not reintroduced any products as time has gone on. If you continue to have problems after 3 months, and you think that you are doing everything right, please phone the Sexual health Clinic for an appointment on 01382 425542. 9. Causes of Genital Lumps Genital warts Molluscum contagiosum Pearly Penile Papules Sebaceous cysts Folliculitis Bartholin’s cysts GENITAL WARTS Genital warts are caused by the Human Papilloma Virus (HPV) and are very common (80% of the adult population have evidence at some time of HPV infection on molecular and serological studies) but visible warts only represent 1% of infected cases. Most infections are subclinical and transient. This explains why it is very common for only one partner in a relationship to have genital warts. Patients in this situation often worry, unnecessarily, about fidelity. 18 Warts are transmitted from one person to another during sex or close genital contact. Genital warts are caused by HPV 6,11,16 and 18. CLINICAL ISSUES Most visible genital warts are caused by HPV types 6 and 11. Types 16 and 18 cause SIL - squamous intraepithelial lesions and all patients with warts should be advised to give up smoking in order to reduce the risk of any potential long term health issues. Women with genital warts need to participate in the standard cervical screening programme. Patients with warts have a 20-30% chance of having another STI, and should be offered screening to exclude these infections. Patients who do not wish to attend GUM should as a minimum have a urine test for Chlamydia. Treatment options: Patients should be told that treatment takes time to work and that 90% of individuals will clear their warts within 12 weeks. Most people with genital warts clear their warts without any treatment by producing antibodies to the wart virus. The treatments help patients produce these antibodies. o Cryotherapy o Podophyllotoxin (Warticon) This comes as a solution-normally used for penile warts, and a cream-female warts and perianal warts. The product is applied bd for 3 consecutive nights followed by 4 days of no application. This is continued for up to 12 weeks. (3 packs of Warticon paint or solution) The treatment can cause localised erythema and discomfort. Only if there is a severe reaction to treatment should the podophylotoxin be stopped. o Imiquimod (Aldara) is an immune modifier and it is applied on 3 nonconsecutive nights each week. Eg. Monday/Wednesday/Friday. The cream is then washed off the next morning. The treatment course can continue for up to 16 weeks. Warts in pregnancy Neither of the above products should be used in pregnancy. It is very difficult to get rid of warts in pregnancy and unless the warts are massive and at risk of obstructing labour, when surgery can be an option, we generally do not treat. Women should be told that any warts which are present at the end of the pregnancy will normally resolve completely, and without treatment, in the first 6 weeks post partum. If this does not occur treatment can be arranged at this point. HPV Vaccine A vaccine is now available to prevent genital wart virus infection with types 6,11, 16 and 18. The vaccination of girls will commence in schools in September 2008. See patient information on website 19