Pharmacy Advisor
advertisement

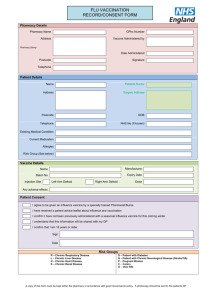
THE PHARMACY ADVISOR A Publication of the Beth Israel Deaconess Medical Center Department of Pharmacy and Pharmacy & Therapeutics Committee Volume II, Issue 5 August/September 2003 Influenza Vaccine Update October will mark the beginning of the 2003-2004 influenza season and all communications from the manufacturers of influenza vaccine and the Centers for Disease Control (CDC) indicate that vaccine production for this influenza season has proceeded satisfactorily. Whereas sufficient supplies will be available for distribution to healthcare providers during October and November to begin immunization programs, the CDC has recommended that the tiered prioritization schedule used for immunization programs in previous years be relaxed and that influenza vaccination programs should be scheduled for all high-risk and healthy persons, individually and through mass campaigns, as soon as vaccine is available. Consistent with this information, the BIDMC has received initial shipments of its annual vaccine order with the majority of vaccine expected to be delivered throughout October. Distribution of vaccine to various clinics and patient care areas will commence as supplies allow and will continue throughout the influenza season. Planned employee immunization programs will begin during October. Specific dates, times and locations will be forthcoming from Employee Health. Annual influenza epidemics cause infection in 10-20% of the population and result in an average of >110,000 hospitalizations and 20,000 deaths in the United States. Influenza vaccination is the primary method for preventing influenza and its severe complications. In recognition of the importance of influenza immunization, continued efforts will be made this year at BIDMC to provide expanded access to influenza vaccine for inpatients. The Massachusetts Department of Public Health (MDPH), the Massachusetts Peer Review Organization (MassPRO), the Department for Health and Human Services and others, have asked all health care providers to vaccinate patients against influenza and pneumococcal disease, which are the most common vaccine-preventable causes of death in the U.S. It is further stated that to avoid missed opportunities, persons at highest risk for complications from influenza should be vaccinated when they are seen for routine health care or are hospitalized. Once adequate supplies of vaccine have been received at the medical center, clinicians at BIDMC will be alerted by the hospital’s Provider Order Entry (POE) system to prescribe influenza immunization for inpatients unless contraindications are present. Additional updates regarding this initiative will be announced throughout the influenza season. The MDPH recommends influenza vaccination for the following groups: I. Persons at Increased Risk for Influenza-Related Complications: All persons > 65 years of age. Persons 6 months – 64 years of age who: o Live in long-term care facilities that house persons of any age with chronic medical conditions. o Have chronic cardiac or pulmonary conditions, including asthma. o Have required regular medical follow-up or hospitalization during the preceding year due to chronic metabolic diseases (including diabetes), renal dysfunction, hemoglobinopathies, or immunosuppression (including immunosuppression caused by medications or HIV). Persons 6 months through 18 years of age who are receiving longterm aspirin therapy. The 2003-2004 trivalent vaccine consists of: H1N1, A/New Caledonia/20/99 H3N2, A/Panama/2007/99 (an A/Moscow/10/99-like virus) B/Hong Kong/330/2001-like virus strain INSIDE THIS ISSUE 1 2 3 4 Influenza 2003-04 Vaccine Update BIDMC Formulary Update: Parenteral Nutrition Update: Clinimix E; Atazanavir (Reyataz ), Bortezumab (Velcade) BIDMC 2003 Renal Dosing Guidelines, Caspofungin Guidelines Spotlight on Pharmacy The Pharmacy Advisor is a publication of the Department Of Pharmacy and the Pharmacy & Therapeutics Committee at the Beth Israel Deaconess Medical Center, Boston, MA 02215 Writing/Editorial Board: Katherine Giampietro, PharmD Christopher McCoy, PharmD Diane Soulliard, PharmD Bruce Bistrian, MD, Co-Chair P&T James Heffernan, MD, Co-Chair P&T Francis P. Mitrano, M.S., RPh Women who will be in the second or third trimester of pregnancy during influenza season. II. Persons Who Can Transmit Influenza to Persons at High Risk: Personnel in both hospital and outpatient settings, including emergency response workers. Employees of long-term care facilities who have contact with patients or residents. Employees at assisted living and other residences for persons in high-risk groups. Persons who provide home care to persons in high-risk groups. Household members of persons in high-risk groups. Household contacts and caretakers of children 0-23 months of age. III. Healthy Persons 50 – 64 Years of Age. IV. Other patient groups may be considered depending upon vaccine availability. Because influenza season in New England generally does not begin until December and does not peak until February, vaccination efforts should continue through December and the entire influenza season, as long as influenza vaccine is available. continued on page 4 The Pharmacy Advisor 1 P&T Formulary Update Parenteral Nutrition Update: The pharmacy department carries a standard premixed amino acid/dextrose solution with electrolytes, which can be used to provide patients short-term fluid and electrolyte supplementation until they are able to be transitioned to either full enteral or parenteral nutrition. The premixed solution facilitates this provision by having a ready-to-use formulation available for patients requiring the initiation or continuation of intravenous nutritional support during the hours that the West Campus IV room is closed. Due to discontinuation by the manufacturer, Baxter’s Quick Mix (Travasol 4.25% with electrolytes in 5% Dextrose) will be replaced by Baxter’s Clinimix E as the premixed peripheral standard solution on Formulary. Clinimix E is a sulfite-free Amino Acid Solution with electrolytes in Dextrose with Calcium. The pharmacy will carry the same standard solution and electrolyte concentration as the previous Quick Mix product (Amino Acid 4.25% with electrolytes in Dextrose 5%) with the single difference being the addition of calcium to the electrolyte profile of the Clinimix E solution. The product profile of Clinimix E is as follows: Amino Acid 4.25% with electrolytes in 5% Dextrose: Sodium 35 mEq / L Potassium 30 mEq/ L Magnesium 5 mEq/ L Calcium 4.5 mEq/ L Acetate 70 mEq/ L Chloride 39 mEq/ L Phosphate 15mmol/L as HPO4= The osmolarity of Clinimix E (Amino Acid 4.25% with electrolytes in 5% Dextrose with calcium) is 815mOsmol/L, allowing it to be administered peripherally or centrally. The caloric content of the admixed product (both protein and dextrose calories) is 340 kcal/L. Additives such as intravenous multivitamins and trace elements are compatible with this solution. Should a patient require supplementation with intravenous fat emulsion, this may be administered concomitantly via Y-type administration. The pharmacy department should be consulted concerning the compatibility of other additives if they are required. Clinimix E is supplied by Baxter in a dual chamber flexible bag, which contains amino acids with electrolytes in one chamber and dextrose with calcium in the other. Prior to use the two chambers are separated by a vertical peel-seal. The pharmacy department will break the seal and mix the solution prior to dispensing for patient use. Additional concentrations of Clinimix E are available from the manufacturer and may be considered for future Formulary use. Changes will be made in POE to reflect the new premixed peripheral parenteral nutrition product. It will be activated in POE early October when the existing inventory of Quick Mix is depleted. It can be ordered in POE during the off-hours when other new peripheral and central parenteral nutrition admixture orders cannot be processed or manufactured. The order tab will read “Premixed Peripheral Standard.” Questions regarding Clinimix E can be directed to the unit-based pharmacists or to the pharmacy clinical call pager at 31195. The following medications have recently been approved for addition to the BIDMC Formulary Atazanavir (Reyataz): Atazanavir is an azapeptide HIV-1 protease inhibitor. FDA Approved Indications: Atazanavir is approved for use in combination with other antiretroviral agents for the treatment of human immunodeficiency virus (HIV-1) infection. Contraindications: Concomitant use with drugs metabolized by CYP3A that may cause serious events if blood levels are elevated [e.g. benzo-diazepines (midazolam and triazolam), the ergot derivatives (dihydroergotamine, ergonovine, and methylergonovine), the GI motility agent (cisapride), and the neuroleptic (pimozide).] Warnings/Precautions: Cardiac conduction abnormalities: atazanavir has been shown to prolong the PR interval of the electrocardiogram in some patients. Use with caution in patients with pre-existing conduction system disease. Hepatic Impairment and Toxicity: Atazanavir concentrations may be increased in patients with hepatic impairment due to decreased metabolism. Hyperbilirubinemia: Symptomatic elevations in indirect (unconjugated) bilirubin related to inhibition of UDPglucuronosyl transferase have been reported. This effect has been observed to be reversible on discontinuation of atazanavir therapy. Hepatic transaminase elevations that occur with hyperbilirubinemia should be evaluated for alternative causes. A change in therapy may be considered if jaundice or scleral icterus is associated with the elevated bilirubin. Dose reduction of atazanavir is not recommended since long-term efficacy of reduced dosages has not been established. Hyperglycemia: Monitor for hyperglycemia. Drug Interactions: Atazanavir is an inhibitor of CYP3A and UGT1A1. Co-administration of atazanavir with drugs primarily metabolized by CYP3A (e.g., calcium channel blockers, HMGCoA reductase inhibitors, immunosuppressants, and sildenafil) or UGT1A1 (e.g., irinotecan) may result in increased plasma concentrations of the other drug that could increase or prolong its therapeutic and adverse effects. Plasma levels are decreased by drugs that increase gastric pH (e.g., antacids, H2 blockers). Concomitant use with St. John’s wort is not recommended due to the potential of decreased atazanavir concentration. Caution should be used when co-administered with medicinal products known to induce PR interval prolongation (e.g., atenolol, diltiazem). Additional drug interactions have been observed. See package insert for full information. Adverse effects: Adverse effects have included GI upset, headache, rash, dizziness, depression, jaundice, scleral icterus, fever, pain, insomnia, cough, fatigue, arthralgia, hyperglycemia, fat redistribution, peripheral neuropathy, hyperbilirubinemia (2 to 5 times the upper limit of normal) Dose: The recommended dose of atazanavir is 400 mg once daily taken with food. When co-administered with efavirenz, atazanavir 300 mg and ritonavir 100 mg should be given with efavirenz 600 mg as a single daily dose with food. When coadministered with didanosine, atazanavir should be given (with food) 2 hours before or 1 hour after didanosine. BIDMC Restrictions: None continued on page 4 The Pharmacy Advisor 2 2003 Renal Dosing Guidelines: The 2003 edition of the BIDMC Renal Dosing Guidelines is currently available from the Department of Pharmacy. This concise pocket card is updated annually and features general dosage and administration recommendations for common medications that require adjustment in patients with renal dysfunction or renal insufficiency. The guidelines are based on published data from several sources referenced on the pocket card and have been further evaluated to optimize available dosage forms of the listed medications as well as convenient dosing schedules. The renal dosing guidelines listed in the pocket card correspond to dose recommendations for renal adjustment in POE. In both cases, it is important to note that while the guidelines serve as a useful reference tool for the majority of patients, patient-specific conditions and clinical circumstances may require dose modification to meet individual patient care needs. Please consult with a unit-based pharmacist to discuss patient-specific medication dosing. Other information found within the Pocket Card includes: Extended-Interval Aminoglycoside Dosing and Monitoring Guidelines, useful formulas for calculating Creatinine Clearance; Ideal, Adjusted and Dosing weights for patients; and recommendations for converting select medications from IV to PO. The estimated daily cost savings for each IV to PO interchange is also provided. For copies of the 2003 Renal Dosing Guidelines, contact a unit-based pharmacist or page the clinical pharmacy pager at ext 31195. ____________________________________________________________________________________________________________ Beth Israel Deaconess Medical Center Pharmacy & Therapeutics Anti-infective Subcommittee Caspofungin (Cancidas) Guidelines (July 2003) (Note: Caspofungin requires Infectious Disease approval) Criteria For Use: Patients with invasive candidiasis, (e.g., candidemia, intra-abdominal abscess, peritonitis, pleural space infection) who are: Intolerant of, or refractory to amphotericin B deoxycholate or fluconazole OR The presumed or identified candidal species is resistant to ampho B deoxycholate or fluconazole Patients with severe candidal esophagitis who are: Intolerant of or refractory to fluconazole or amphotericin B deoxycholate. Patients with presumed or proven invasive aspergillosis who are: Intolerant of or refractory to amphotericin B deoxycholate, liposomal amphotericin B or itraconazole. OR The presumed or identified aspergillus species is resistant to ampho B deoxycholate or itraconazole Amphotericin B deoxycholate intolerance is defined by: A minimum trial of conventional amphotericin B deoxycholate (example: 0.6mg/kg/day x 5 doses) with: An increase of >0.5mg/dl in serum creatinine compared to the baseline prior to therapy in the absence of rapidly reversible causes (i.e. recent contrast, dehydration, etc.) despite adequate hydration and discontinuation of other nephrotoxins, OR Severe or persistent infusion-related adverse events (e.g., fever >100.4 F, rigors, flushing) despite premedication or comedication regimens (pre and post-dose 500 mL NS, pre dose APAP 650 mg, diphenhydramine 25- 50 mg, meperidine, etc.) Refractory treatment to amphotericin B as defined by: Disease progression after > 500mg or 7mg/kg total dose amphotericin B (Example: 1mg/kg daily dose x 7 doses =7mg/kg total dose) Caspofungin without initial challenge to other antifungal agents is reserved for the following patients: Patients with an invasive candidal infection: Identified or presumed to be resistant to fluconazole and amphotericin B OR With a history of severe and/or persistent adverse reactions to these agents Patients with an invasive candidal infection or severe esophageal candidiasis: Identified or presumed to be resistant to fluconazole AND A baseline serum creatinine of >2.5mg/dl or CrCl <40 mL/min Dosing: INDICATIONS DOSE Invasive candidiasis: 70 mg IV x 1 dose, then 50 mg IV qd* Severe refractory candidal esophagitis: 50 mg IV qd (no loading dose) *Dose increases to 70 mg IV qd may be necessary in patients not responding after 72 hours with severe invasive disease. Similar dose increases may be necessary in patients taking rifampin concomitantly or other potent CYP 450 3A4 inducers (e.g., carbamazepine). Dose reductions to 35mg IV qd may be necessary in patients with moderate hepatic dysfunction and in patients on concomitant cyclosporine. Dosing adjustment: Hepatic impairment (Child-Pugh Class B): 35 mg IV qd maintenance dose Premedications: Acetaminophen 650 mg po, Diphenhydramine 25 mg prn infusion related reactions 30 minutes prior. Renal impairment (CrCl <50mL/min): No adjustment required Monitoring Guidelines: Baseline Child Pugh Score based on degree of encephalopathy, ascites, albumin, total bilirubin and PT to determine dose. Weekly AST/ALT, alkaline phosphatase, total bilirubin, albumin and PT. Draw twice weekly if on concomitant cyclosporine for the first week, then once weekly. Infusion related reactions (e.g., flushing, fever, hypotension) during first 30 minutes of initial infusion. Daily tacrolimus levels if on concomitant tacrolimus Signs of hypersensitivity (e.g., rash, laryngeal edema) during initial infusion during first 30 minutes of initial infusion. This guideline has been designed to assist the clinician in the utilization and dosing of caspofungin. It is not intended to replace clinical judgment where individual patient characteristics may require modification of the recommendations. The Pharmacy Advisor 3 Spotlight on Pharmacy: Recognition in Pharmacy is extended to the following members of the BIDMC Department of Pharmacy for their recent accomplishments: Graduate Degrees: Mia Hong, RPh, received her Master of Science Degree in Drug Regulatory Affairs and Health Policy from the Massachusetts College of Pharmacy and Health Sciences. Her Master's Thesis was entitled "At the Crossroads of U.S. Gene Therapy Research". Doctor of Pharmacy: Pharmacists recently completing their Doctor of Pharmacy program include: Lauren Kill, PharmD, Violetta McCarthy, PharmD and Ayu Tesfaye, PharmD. Pharmacy Technician Certification: The following pharmacy technicians have recently received certification having attained a passing score on the national pharmacy technician certification examination: Tewosta Abrha, Jean Beach, Sammy Belton, Julie Lanza, Andrea Nardone, Michelle Walker and Ellen Welter __________________________________________________ Influenza Vaccine Update continued from page 1 FluMist™ (Influenza Virus Vaccine Live, Intranasal), was recently FDA approved as the first influenza vaccine delivered as a nasal mist available in the United States for healthy people. FluMist™ is indicated for active immunization for the prevention of disease caused by influenza A and B viruses in healthy children and adolescents, 5-17 years of age, and healthy adults, 18-49 years of age. FluMist™ is NOT indicated for children less than 5 years or for adults 50 years and older. FluMist™ is contraindicated in persons with hypersensitivity to any component of the vaccine, including eggs; in children and adolescents receiving aspirin therapy or aspirin-containing therapy; in individuals with a history of Guillain-Barré syndrome; and in individuals with known or suspected immune deficiency. The safety and efficacy of FluMist™ have not been established in pregnant women or for patients with chronic underlying medical conditions, including asthma or reactive airway disease; thus this product should not be administered to these patients. Because FluMist™ contains live influenza viruses, a potential exists for transmission of these viruses from vaccines to other persons. The CDC has recommended in the September 26,2003 MMWR, “Using Live, Attenuated Influenza Vaccine for Prevention and Control of Influenza,” that no data are available assessing the risk for transmission of live, attenuated influenza vaccine, from vaccine recipients to immunosuppressed contacts. In the absence of such data, use of inactivated influenza vaccine is preferred for vaccinating household members, health-care workers, and others who have close contact with immunosuppressed persons because of the theoretical risk that a live, attenuated vaccine virus could be transmitted to the immunosuppressed person and cause disease. In accordance with this recommendation, FluMist™ will NOT be available for use as part of the influenza immunization programs for inpatients and employees at BIDMC. P&T Formulary Update continued from page 2 Bortezomib (Velcade) Bortezomib is a potent, selective, and reversible proteasome inhibitor. FDA Approved Indication: Bortezomib is indicated for the treatment of multiple myeloma patients who have received at least two prior therapies and have demonstrated disease progression on the last therapy. Bortezomib is also being studied in metastatic colorectal cancer, advanced non-small cell lung cancer, and various hematologic and solid tumors. Pharmacokinetics: Bortezomib is rapidly cleared from the plasma and is oxidized via cytochrome P450 enzymes (CYP 3A4, 2D6, 2C19, 2C9, and 1A2). However, the major metabolic route is deboronation to inactive metabolites. The elimination half-life is 9 to 15 hours. Plasma protein binding is 83%, while the volume of distribution has not been determined. The impact of age, gender, race, and hepatic or renal function on the pharmacokinetics of bortezomib have not been evaluated. Contraindications, Warnings, And Precautions: Pregnancy: Category D: do not use during pregnancy or breastfeeding. Neuropathy: Monitor for the development of peripheral neuropathy throughout therapy. Thrombocytopenia: Thrombocytopenia is a common adverse event (40%), generally occurring during the first 2 cycles of treatment, but could occur throughout therapy. Some patients may require temporary discontinuation of therapy, especially in those who experience Grade 4 thrombocytopenia. Reinitiate therapy at a reduced dose after resolution of the thrombocytopenia. Hypotension: Orthostatic/postural hypotension occurred in 12% of patients. Use with caution if the patient has a history of syncope, utilizes medications that cause hypotension, or in patients who are dehydrated. GI Effects: Gastrointestinal events, such as nausea, diarrhea, constipation, and vomiting may be severe enough to warrant therapy with an antiemetic or antidiarrheal agent. Fluid and electrolytes may be necessary to avoid dehydration. Renal/Hepatic dysfunction: The impact of hepatic or renal dysfunction on the elimination of bortezomib is unknown. Adverse Reactions: The most commonly reported adverse effects have included thrombocytopenia, peripheral neuropathy, nausea, vomiting, diarrhea, constipation, fatigue, malaise, weakness, anorexia, decreased appetite, pyrexia, and anemia. Consult the package insert for a complete list of adverse reactions reported with bortezomib . Drug Interactions: No formal drug interaction studies have been conducted. Bortezomib is a substrate of cytochrome P450 3A4, 2D6, 2C19, 2C9, and 1A2 so it may be at risk of drug interactions involving these enzyme systems. Recommended Monitoring: Complete blood counts, including platelet counts, should be monitored frequently throughout bortezomib therapy. Blood glucose levels should be closely monitored in patients with diabetes. Dosing: The FDA-approved dosing regimen is 1.3 mg/m2/dose administered as a bolus IV injection twice weekly for 2 weeks followed by a 10-day rest period. Dose adjustments are required if the patient develops Grade 3 non-hematological toxicities, Grade 4 hematological toxicities, or neuropathic pain and/or peripheral sensory neuropathy. In these situations the therapy should be withheld until the problem is resolved. If therapy is restarted, the dose should be reduced by 25% in most of these situations. BIDMC Restrictions: FDA approved indications. The Pharmacy Advisor 4