Rabies report
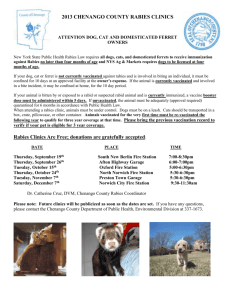
advertisement

Rabies, the Fury Disease Although rabies is most affected countries of Asia, Africa, and Latin America is a primarily a disease of dogs, the species most commonly affected in the U.S. are skunks, bats raccoons, and foxes. Although this disease is maintained in these species, most human exposure is from contact with rabid or possibly rabid domestic animals. Because control of wildlife rabies is so difficult, rabies in the U.S. is now primarily controlled by creating an immune barrier of vaccinated domestic animals between the wild animals and humans. Every year, approximately 30,000 people are given postexposure rabies prophylaxis. Good diagnosis and reporting are essential in following the movement and identifying patterns of disease. The epidemiology of rabies varies greatly from one part of the country to another. Countries affected mostly by wildlife rabies, such as the U.S., Canada, and many parts of Europe, have fewer rabies exposures than the majority of the countries of Asia, Africa, and Latin America, where rabies in dogs continues to pose the greatest problem. In these latter countries, the number of people treated for rabies exposures (bites or scratches by rabid animals or by animals that might be rabid) is from 6 to 25 times the number treated in countries with predominant wildlife rabies. Finally, there are several countries, most of which are islands, that are rabies free; these include England, Ireland, Australia, New Zealand, Japan, Taiwan, many of the Caribbean islands, Sweden, Norway, and Spain. The countries with predominant wildlife rabies make up 10% of the world. They include the U.S. (with rabid skunks, raccoons, foxes, and insectivorous bats), Canada (with rabid foxes and skunks), countries of Europe (with rabid foxes), and South Africa and the larger Caribbean islands (with rabid mongooses). In the U.S., Canada, and Europe, the main public health problem is with the domestic species-dogs, cats, and cattle-associated with humans-even though the disease is maintained in wild animals. In fact, most of the human rabies exposures in the U.S. are from dogs rather than wild animals, and epidemiologic studies have shown that in the U.S., people are most often vaccinated following dog bites, not bites from wild animals. For example, in one 1968 study in Illinois, a state with a sizable skunk rabies problem since the 1950’s, more than 60% of the reported rabid animals are skunks, but exposure to these animals accounted to only 12% of the total human vaccinations. In contrast, only 18% of the reported rabid animals were dogs and cats, but exposure to these animals accounted for 62% of the human vaccinations (Schnurrenberger 1969). The rabies endemic in the U.S. results in 25,000 to 30,000 people being treated annually for exposure to rabid animals or animals that might be rabid, especially ones that escape after biting (especially dogs). In 1958, a major change occurred in the course of rabies in the U.S., because for the first time more cases of rabies were reported in wild animals than in dogs. This declined in canine rabies began after WWII and was the result of the combined effort of potent vaccines and organized control programs. Before 1945, there was no potency test for rabies vaccines, and after the test was developed, few vaccines were found to be potent. The control programs resulted in hundreds of thousands of dogs being vaccinated in organized urban campaigns in cities throughout the country (Figure 1). With the availability of potent vaccines and organized programs, the rabies epidemiology in the country underwent an important change (Table 1). No longer were there outbreaks of rabid dogs in urban areas, and the number of human deaths plummeted. Whereas 47 people in the U.S. died of rabies in 1938 and 53 in 1944, an average of one person per year has died of rabies in the U.S. since 1960 (Figure 2). As would be expected, almost all human rabies cases since the early 1960’s have resulted from exposures to rabid bats, skunks, and foxes-not exposures from rabid dogs. The present mid-Atlantic outbreak in raccoons started in 1979, with the diagnosis of the disease confirmed in abnormally acting raccoons used in radiotelemetry studies at the National Zoological Park in Front-Royal, Virginia. There has been a rapid increase in cases in Virginia since then (Center of Disease Control 1982). But how did the disease get to Virginia and then spread to West Virginia, Pennsylvania, and Maryland? It either came from raccoons that were bitten by local rabid bats or from translocation raccoons. The second theory is based on the fact that heavy traffic of raccoons from Florida and Georgia, states known for both problem raccoons and rabies since 1955 (Kaplan 1987), to the central Atlantic states. In on e shipment, two rabid raccoons were found among 165 raccoons being shipped from Florida to a North Carolina hunting club. Although the two raccoons were destroyed, the rest of the raccoons were released and it is believed that at least ¼ of the 165 raccoons had picked up the disease, but were not showing signs at the time of release. Similar outbreaks to the one occurring in the Mid-Atlantic States can be readily found. One such outbreak was reported in the 1940’s in N.Y. (Baer 1983), where the disease suddenly appeared in foxes, although the infection was most likely due to spread from other local species. The investigators who looked at the outbreak suggested that the disease was present in foxes well before it exploded in 1944 and 1945. This suggestion was based on two reports in 1941 and 1943 where rabid foxes were reported. These reports emphasize the importance of good reporting to follow the movement of the disease. A much larger outbreak in foxes began in foxes on the border between Poland and Germany in 1939 and 1940, in the Oder-Neisse region, and spread across Germany in the 1950’s, Austria in 1966, Switzerland in 1967, France in 1968, and Italy in 1977. In spite of limited success in controlling the disease by den gassing, this control method has not proven practical or efficient in reducing the disease (Debbie 1972). The outbreak in the U.S. have been dramatic, but it is the disease that remains in the wake of these new extensions, the “endemic disease,” which maintains the constant level of wildlife cases in this country. Skunk rabies, for instance, has been responsible for maintaining the disease in the Midwest since the early 1950’s (Winkler 1982) (Figure 2), and this species causes most of the cases in cattle, dogs, and cats. The location of cases in these three species can be superimposed on the “skunk map,” where there is skunk rabies, there is also most of the domestic species rabies. This transmission from wild animals to the domestic species is seen, although to a lesser extent, with raccoons in the southeast and Mid-Atlantic States and foxes in the northeast and Appalachia. The control of wildlife rabies is difficult. Although population reduction had been used in the past, it is not possible to kill enough animals to effectively control the disease, except for short periods of time in limited areas. Another method is to mass immunize wild animals. Mass immunization would permit control of the disease in the endemic species, especially skunks. Research on this method of control is being done currently in the U.S., Canada, and various countries in Europe. Rabies in the U.S. is primarily controlled by creating an immune barrier of vaccinated dogs and cats between the rabid wild animals and humans. It is this barrier that results in the reduced number of cases in domestic animals, especially dogs. Veterinarians reduce the rabies danger by following certain practices: *Faithfully vaccinate dogs and cats and keep these shots current. *Make every effort to have the maximum number of animals in the community vaccinated. *Be sure the report any case of rabies in a vaccinated animal. *Avoid contact with abnormally acting animals and friendly wild animals. *Do not own any wild pets. *Be sure that you have the preexposure immunization for rabies. Table 1: Change in number and percentage of animals reported rabid in the U.S. in 1938 and 1988 animal Dogs Cats Cattle Horses Sheep Goats Swine Others Man totals 1938 1988 number percentage number percentage 8542 89.9 119 3.6 207 2.1 96 2.9 413 4.4 205 6.2 32 0.3 39 1.2 164 1.7 3 0.1 11 0.1 4 0.1 42 0.4 3 0.1 44 0.4 2825 85.6 47 0.4 4 0.1 9412 3298 *Others include bats, skunks, raccoons, foxes, coyotes, bobcats, weasels, wolves, mink, squirrels, caribou, bear, deer, woodchucks, ferret, and weasels. Pathogenesis of Rabies Most warm-blooded animals are susceptible to rabies virus infection, and with rare exceptions, infection ends in death. In the natural setting of the virus in feral animal populations, this outcome serves to circumvent the development of any degree of natural “herd immunity” which would otherwise be a deterrent to the movement, persistence, and reintroduction of the virus. In nature, rabies virus cycles in concert with the emptying and repopulating of its reservoirs host econiche. Often the emptying is a result of epizootic rabies, and the repopulation that follows is a result of migration and birth of new generations of susceptibles. The slow course of infection in the individual reservoir host assures that virus will survive until the new susceptible host generation repopulates the econiche to a density necessary for efficient virus transmission. If the lethality of rabies infection in the individual wild animal is the key to its life cycle in the whole populations, then the question of why the infection is so lethal has added interest. This question of disease pathogenesis is also pertinent in discussions of rabies in populations of domestic animals-there is no difference in the pathogenetic behavior of the virus in dogs and cats, but there is in foxes, skunks, and raccoons. Virus Invasion, Local Infection, and Transit to the Central Nervous System Following the deep introduction of rabies virus by the bite of a rabid animal, initial virus replication occurs in striated muscle cells at the site. This infection of muscle, which was first found in experimentally infected hamsters and later in skunks, can serve as an amplifying source of the virus for an assault upon the exposed endings of the peripheral nervous system. Muscle may also be the site of the sequestration of the virus during long incubation infections, but this has never been proven. Deep in the muscles, the peripheral nervous system is exposed in neuromuscular spindles (the sensory stretch proprioceptors made up of modified muscle cells wrapped in unmyelinated nerve endings). In studies of street rabies viruses in hamsters and skunks, spindles were the second tissue to become infected; from such studies it was concluded that these exposed sensory nerve endings were an important site of virus entry into the nervous system. Another site deep in the muscles where the virus may enter the nervous system is the motor end plates (the motor nerve endings in muscles). In the olfactory end organ in the nares, neuroepithelial cells are in direct contact with the body surface; these cells extend without interruption into the olfactory bulb of the brain. Olfactory neuroepithelium is easily infected and is the key to efficient aerosol transmission of rabies virus in bat caves. Similarly, the many sensory nerve endings of epithelial and subepithelial tissues of the skin and mucous membranes may serve as a site for virus entry when exposed by superficial abrasion. Superficial abrasion, although not as efficient as deep entry routes, has been implicated in some human rabies cases and probably is the key to transmission among animals in the absence of fury. The entry of rabies virus into nerve endings begins an infection phase in which neuronal infection and centripetal (towards the center) passive movement of viral nucleic acid within axons leads to invasion of the central nervous system, first in the spinal cord and then in the brain. The slow course of virus movement to its ultimate target organ, the brain would seem to provide opportunity for the full spectrum of host defenses to come to bear. Nonspecific inflammatory response may be stimulated by the trauma at the bite site, but this does not seem to interfere with the initiation of infection. Rabies virus proteins easily stimulate specific antibody and cell-mediated immune responses in model systems, but in nature these host defenses fail. Them most likely reason for this is that little virus antigen is presented to trigger host response. There are several possible explanations for this (1) There may be very little virus and virus antigen delivered into the bite site-enough virus to initiate infection but not enough antigen to evoke an immune response; (2) There may be very little virus and virus antigen produced in muscle early in the infection, and that which is produced may remain hidden within muscle cells which are not damaged by infection; (3) There may be very little virus and virus antigen produced in peripheral nerves, and that which is produced may remain hidden beneath the myelin sheaths which surround the nerves (here too there is no damage caused by the virus which would stimulate inflammation); (4) There may be very little virus and virus antigen released from infected neurons in the central nervous system. Even rather late in rabies infection, when neuronal infection is widespread, the immunologically sequestered environment of the brain (free of most lymphocyte trafficking and lymphatic drainage) keeps virus antigen from triggering an immune response (Murphy 1987). Basically, the host response to rabies infection has reason to delay and of minimal intensity until it is too late to matter. This is the case in natural rabies infections of the wild or domestic animals-or even of man. Neutralizing antibody and inflammatory infiltration are usually absent at the time of onset of encephalitic signs and reach substantial levels only at the time of death. Pathogenetic Events in the Brain Following the entry of virus into the Central Nervous System, usually in the spinal cord, an ascending wave of neuronal infection and neuronal dysfunction occurs. This is seen clinically as ascending paralysis and experimentally as an ascending wavefront of infectivity within the brain is the most likely of specific clinical signs including fury. R.T. Johnson states: The greater localization of infection to the limbic system with relative sparing of the neocortex provides a fascinating clinicopathologic correlate with at alertness, loss of natural timidity, aberrant sexual behavior and aggressiveness that may occur in clinical rabies. No other virus is so diabolically adapted to selective neuronal populations that it can drive the host in fury to transmit the virus to another animal. Clinical signs of fury, of limbic system dysfunction, and of release of cortical control represent a stage in the ascending neuronal infection in the brain. Later, as infection reaches the neocortex, clinical signs match those of dumb rabies, the form of the disease in which no fury is seen at any stage. In dumb rabies and in the terminal stage of furious rabies, it is the infection and dysfunction of neurons of the higher centers of the brain that result in depression and coma. Death follows respiratory arrest. One of the most remarkable aspects of this pathogenic pattern is that it has become a necessity for the survival of the virus-rabies has no alternate life cycle that could assure virus survival (Murphy 1987). Virus Transit to the Site of Transmission As if the necessity for such a precise pattern of infection in the brain were not remarkable enough, consider the added that for transmission to occur, virus must be delivered into saliva at the same time as the animal become furious. In order to accomplish this, the infection, which until this point has been specifically neurotropic (muscle accepted), broadens to involve mucous cells of the salivary gland. This infection site, initiated from nerves entering the glands, is very productive, delivering in some reservoir host species, such as the dog, fox, and skunk, up to one million infectious units of virus per milliliter of saliva (Figure 1). One more remarkable characteristic of rabies infection concerns the site of growth of the virus in the various target organs. In the nervous system most virus is formed upon membranes within cells which are not actually destroyed by the infection; this virus is trapped and hidden from the immune system and inflammatory systems of the host. However, in the salivary glands nearly all virus is formed upon plasma membranes of mucous cells and is therefore immediately delivered into saliva by normal secretory flow. Late in the rabies infection, other tissues and organs are infected by the same route as used by the virus to reach the salivary glands, which is by nerves leading centrifugally (from the center) to nerve endings located in contact with susceptible nonneuronal cells. For example, rabies virus commonly infects the adrenal cortex and the pancreas. Nevertheless, it is difficult to attribute any important aspect of the pathogenesis of the infection to virus activity anywhere other than in the nervous system and salivary glands. To search too hard for the hypothetical significance of other extraneural target sites of the infection seems to place too little emphasis on the invariably lethal progression of the central nervous system infection (Murphy 1984). Rabies Histopathology The histopathology of street rabies encephalitis contributes little to our understanding of the pathogenesis of the disease. Typically, there are no gross pathologic changes other than a variable degree of cerebral edema. Microscopic changes of perivascular mononuclear inflammatory infiltration, inflammatory destruction of neurons (neuronophagia), and neuronal necrosis are sparse in relation to the extent of the infection as visualized by fluorescent antibodies. When the fluorescent antibody technique is applied to frozen sections of brain from terminal street rabies cases, the usual conclusion is that every neuron everywhere in the brain is reached by electron microscopic examination of brain specimens (figure 2). Light microscopic histopathology, which all too often has focused only on the Negri body, the inclusion body found in the cytoplasm of neurons (figure 3), underestimates the widespread distribution of rabies virus in the brain late in the course of the encephalitis. But it does reemphasize the extraordinary dichotomy of minimal cellular destruction associated with maximal neurologic dysfunction (Murphy 1984). The Ecologic Significance of the Pathogenetic Pattern of Rabies Infection Consideration of all of the elements of rabies pathogenesis in the individual animal may tempt the conclusion that virus survival in nature, without human influence, is tenuous. This temptation might be reinforced by consideration of the ecologic hurdles faced by the virus. It is clear that rabies virus is a most successful parasite. In its diverse econiches, including those involving dogs and cats, there is enough transmission to assure virus perpetuation and even entrenchment-entrenchment meaning that eradication will prove to be impossible or at least very difficult. In reality, the same elements of rabies pathogenesis and ecology that might be used to predict tenuous survival probabilities can be used to describe the pathogenetic basis for entrenchment in the environment. Through evolutionary adaptations, the virus has become entrenched in its traditional econiches but is still capable of invading new econiches such as those of civilized man. If rabies is to be controlled and eradicated from its diverse econiches, so as to minimize the risk of disease in humans and animals, its pathogenesis must be examined for “weak links” in the infection and transmission chain (Bear 1983). The Pathogenetic Basis for Rabies Prevention, Postexposure Treatment, and Control For most of its path from its entry site in the bite of a rabid animal to its arrival in the brain, rabies virus must be considered to be vulnerable to antiviral chemicals and biologics. Antiviral chemicals and biologics might be anticipated to work best at a stage where they can interrupt or intercept the virus before it invades the privileged environment of the peripheral nervous system. If multiple virus growth cycles occur at the bite site, such as in muscle, and only progeny of this growth gain access to the nervous system, then prophylactic and postexposure treatment regimens may have the time and opportunity for action at the entry site. Alternatively, regimens aimed at late interception of the virus, after nervous system invasion, might be expected to be without benefit or even to be the cause of exaggerated immunopathologic disease. Many attempts to deny this conclusion have ended in failure, and in many efforts in clinical practice, ideas have fallen to the wayside. For example, antiviral chemicals, which shut down the viral synthetic processes used by rabies virus, do not interrupt the course of neurologic spread of rabies infection in vivo. Biological products, like interferon and antibody, do not interrupt the course of rabies infection once the virus has gained the protected surroundings of the peripheral nerves. Prevention of rabies in animals and in humans at high risk of exposure, such as veterinarians and wildlife workers, and preexposure treatment of individuals who have been exposed to the virus requires the immediate delivery of antiviral products to the site of virus entry. This is the same rationale that was first used by Pasteur. Practically, this means that preexposure immunization of dogs, cats, and man should be accomplished with the most potent vaccines available, and research should be continued toward developing even more potent vaccines. Prophylactic administration of a potent vaccine is the only way to ensure that enough antibodies will be present at any bite site at the time of virus entry. Administration of a potent vaccine as a booster after exposure in previously immunized individuals is the best way to ensure that antibody titer will be amplified quickly. In nonimmunized humans exposed to rabies, the injection of hyperimmune rabies globulin (HRG) into the area of the bite delivers antiviral activity of maximum potency at the most important time. These strategies are complimented by the age-old advice to wash and disinfect all wounds immediately after exposure. Rabies control depends on the development of effective population immunity. Immunization of dogs and cats, and even wildlife species, so as to break the virus transmission cycle, must be aimed at the single weak link in the pathogenetic pattern of infection-the bite site. Shutting down virus growth at this point prevents the subsequent problems of death of the animal and transmission to the next animal (please see the recommended immunization procedures, vaccines, and principles of rabies control written by the Compendium of Animal Rabies Vaccines in 1993 at the end of this report). Laboratory Diagnosis of Rabies Since rabies virus is impossible to detect just from looking at an animal (although the “fury” and “coma” stages are good indicators for sickness), it is necessary for modern laboratory techniques to provide accurate and rapid diagnosis. Let me make this clear before I start that living animal are not accepted for rabies diagnosis. They are considered a danger to the veterinarian or wildlife worker and can affect other animals in the transport. All pets exposed are treated with multiple expensive vaccinations. Only humans and dead animals are effectively tested for rabies. There are multiple ways in the laboratory to diagnosis rabies. I will not go into depth on these, but if you would like further information I would recommend you investigate the article marked with an * in the literature sited. Dead animals are usually tested through samples of the brain using necropsies to collect the sample and test through the fluorescent antibody test, tissue culture isolation tests, and histopathology test for Negri bodies. Since humans are not dead and I doubt they would let you take a sample of their brain while still alive, the rabies antibody tests to confirm enough antibody to effectively fight off the virus in people who have already been vaccinated for the virus. They usually give you a titer shot just in case. If you do not already have the vaccinations, Multiple shots are give between 24-30 in a 2-month period with constant tests of antibodies. The Cost of Prevention Rabies prevention and control strategies in the United States have succeeded in lowering the number of human rabies deaths to an average of one to two per year. However, the reason for this low mortality level is a prevention program estimated to cost $230 million to $1 billion per year (13-15). This cost is shared by the private sector primarily the vaccination of companion animals) and by the public (through animal control pro-grams, maintenance of rabies laboratories, and subsidizing of rabies PET). Accurate estimates of these expenditures are not available. The number of PETs given annually in the United States is unknown, although the total must be substantially greater than the minimum of 20,000 estimated in 1980 to 1981 (16) when vaccine distribution was more tightly regulated. As rabies becomes epizootic or enzootic in a region, the number of PETs increases (17). Although the cost varies, a course of rabies immunoglobulin and five doses of vaccine given over a 4-week period typically exceeds $1,000. Potential exposure to a single rabid kitten in New Hampshire recently led to the treatment of more than 650 persons at an estimated cost of $1.5 million (18). Surveillance-related costs also rise as rabies becomes entrenched in wildlife. During 1993, the New York State rabies diagnostic laboratory received approximately 12,000 suspected animal submissions. This compares with approximately 3,000 submissions in 1989, before raccoon rabies became epizootic. In New Jersey, rabies prevention expenditures in two counties increased from $768,488 in 1988, before the raccoon epizootic, to $1,952,014 in 1990, the first full year of the epizootic (15); vaccination of pet animals accounted for 82% of this total. Vaccinated domestic animals are normally administered a booster vaccine dose after a known or suspected rabid animal exposure (19). This further increases costs, as wildlife rabies epizootics escalate. The cost per human life saved from rabies ranges from approximately $10,000 to $100 million, depending on the nature of the exposure and the probability of rabies in a region (20). What's more, most economic analyses do not take into account the psychological trauma caused by human exposure to rabies, the subsequent euthanasia of pets, or the loss of wildlife resources during rabies outbreaks. Rabies in wildlife has now reached historically high levels in the United States (12), and the costs of preventing human rabies are mounting. There is no immediate answer just to continue studies for more effective plans of treatment and more effective vaccines. Literature Cited: *Baer, G.M. 1983. Control of the rabies virus infection of animals and man. New York, Academic Press. pp 553-562. Baer, G.M. 1985. The natural history of rabies, vol. II. New York, Academic Press. Centers for Disease Control: Rabies-Mid-Atlantic States. 1982. Morbidity and Mortality Weekly Report 31:592-593. Debbie, JG, and M.K. Abelsth. 1972. The use of commercially available vaccines for the oral vaccination of foxes against rabies. American Journal of Epidemiology 96:231235. Grave, L.M., E.S. Tierkel, H.G. Tuggle, and S.L. Wadley. 1950. Effective control of an outbreak of rabies in Memphis and Shelby county, Tennessee. American Journal of Public Health. 40:1084-188. Kaplan, C. 1987. Rabies, the facts. London, Oxford Press. Murphy, F.A. and F. Brown. 1984. Animal virus vaccines: genetic engineering technology in rabies vaccine. New York, Marcel Dekker Inc. Murphy, F.A. 1987. Rabies pathogenesis-a brief review. Arch Virology. 54:279-297. Steck, F. 1992. Oral immunization of foxes against rabies. Comparative immunology and Microbiology of Infectious Diseases. 5:165-171. Schnurrenberger, P.R. 1969. Epidemiology of human exposure to rabid animals in Illinois. Public Health Report 84:1079-1084. Winkler, W.G. 1982. Rodent rabies in the U.S. Journal of Infectious Disease. 125(5):565-567.