DO I NEED A RABIES PREVENTION VACCINE
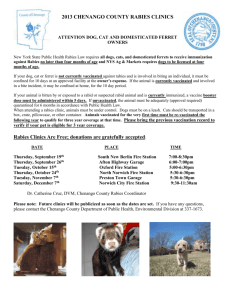
advertisement

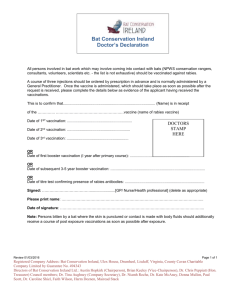
DO I NEED A RABIES PREVENTION VACCINE when working with BEHAVIOUR DOGS? Rabies is a viral infection that is transmitted to humans through close contact with the saliva of an infected animal, most often by a bite or scratch, or by licks on broken skin or mucous membranes, such as the eyes, nose or mouth. Worldwide, dog bites are responsible for most human cases of rabies. You may want to review the information below and make your own decision about whether you need a vaccine. Note that vaccine supplies can be limited and your doctor will need to support your decision. Cause - The rabies virus is the type species of the Lyssavirus genus, in the family Rhabdoviridae, order Mononegavirales. How Could I Get Rabies? - Risk varies depending on location, purpose and duration of trip, as well as lifestyle, activities, and access to medical care. Travellers who engage in activities which place them in close contact with animals, such as camping, hiking, or cycling in areas where rabies is found, may be considered high risk. People who work in close contact with animals, such as veterinarians, animal control or wildlife workers, or laboratory workers handling rabies specimens, hunters and trappers in high-risk areas, spelunkers (cave explorers) are at high risk, especially from bites as the virus tends to concentrate in the salivary glands. It would be reasonable to assume dog behaviour specialists, particularly those handling feral animals, might be at risk. Children are also considered at high risk because they often play with animals and are less likely to report bites or scratches. Bites in children are usually higher on the trunk or face and are often more severe. It is a legal requirement in Ontario Regulation 567 under the Health Protection and Promotion Act for all dog and cat owners to immunize their animals against rabies. However, the majority of domestic biting incidents in Ontario involve un or under-vaccinated animals. (1 As of April 2010, between 60-75% of domestic animals involved in bite investigations by public health are not current on their rabies vaccinations.) How Can I Tell if a Dog Has Rabies? – Of course, you need to check with your veterinarian if you suspect a dog might have rabies to make a diagnoses. In dogs, the incubation period is under four months in about 80% of cases (and is usually about three to twelve weeks). Signs you can look for include that might indicate rabies include changes in temperament, fever and irritation at the site of the bite where the infection entered. Virus is in the saliva seven days before symptoms appear and the animal usually dies within a week or ten days after that. There are two types of rabies – in one the dog will tend to hide, drool, show paralysis in the jaw, neck and back legs and have trouble swallowing. In the other, more common type, they become irritable, have difficulty swallowing and a changed bark because their larynx is paralyzed, tremble, snap, be very restless and irritable, attack and swallow inanimate objects (sometimes breaking their teeth and hurting their mouths). Severity and Spread - Once symptoms appear, rabies is almost always fatal. Rabies is spread when virus from the saliva of an infected animal enters the nervous system of the victim through a bite, scratch, broken skin, or the mucous membranes (eyes, nose, mouth). Worldwide, this often occurs through a dog bite or scratch, and there have been three rare reports in the east of virus being shed in the saliva of a healthy dog with rabies immunity. Person-to- person transmission is theoretically possible, but rare and not well documented. On rare occasions, transplants have caused rabies in recipients as has drinking milk from a rabid cow. Airborne spread has been demonstrated in a cave where bats were roosting and in laboratory settings, but this occurs very rarely. While dog bites are generally easy to identify, bat transmission is not so clear (can occur from bite and in some cases of Lyssavirus from bats an airborn spread has been suggested). If anyone comes into contact with a sick bat, it is strongly recommended that a quarantine or rabies test be considered for the bat. Only a small number of people who died from the bat rabies variants showed any bite wounds. This may be because the wound left by a bat is very small. Picture 1: Puncture wound of a bite from a silver-haired bat (A, arrow) and skull of silver-haired bat (B) How long does the rabies virus last outside the body and in dead animals? The life span of the rabies virus depends on the duration of its exposure to air and climatic conditions. Freezing does not kill the virus. Always assume that a dead animal may still have the virus. What is the incubation period of rabies in humans? - The incubation period, which is the time period between exposure to the virus and the onset of symptoms, can range from approximately three weeks to eight weeks, but can be as short as nine days or as long as seven years. The incubation period depends on a number of factors, including the severity of the wound, the location of the bite and the susceptibility of the person to infection. People who are immunocompromised will most likely be more susceptible to rabies. What are the signs and symptoms of rabies in humans? - In humans, rabies usually begins with fever, cough, or sore throat and is followed in several days by more serious and rapidly progressing symptoms such as hallucinations and seizures. Symptoms progress quickly as the central nervous system is attacked, and the illness generally presents in one of two ways: "Furious rabies" is more common, and is characterised by anxiety and psychological disturbances (confusion, agitation, delirium, rage, hallucinations, and hydrophobia). "Dumb rabies" occurs in approximately 20% of patients and presents with paralysis. In both "furious" and "dumb" rabies, death usually is within seven days due to breathing failure caused by paralysis of the respiratory system. Rabies still poses diagnostic problems, particularly the paralytic form, which closely resembles Guillain-Barré syndrome, or when a patient is comatose and cardinal signs may be lacking. Molecular methods allow reliable detection of rabies-virus RNA in biological fluids or tissue before death. What medical attention do I need if I am exposed to rabies? - If you are bitten by a suspected rabid animal or if infectious material (such as saliva) from a suspected rabid animal gets into your eyes, nose, mouth, or a wound, then you should wash the area with soap and water immediately. Wounds should be washed thoroughly. Ethanol, while irritating, can be applied to open wounds. Large volumes of 20% aqueous soap solution or quaternary ammonium disinfectant should be applied under pressure to bites. All in-contact individuals should report immediately to a doctor to determine whether a rabies post-exposure vaccination is required. Rabies vaccinations will be administered promptly if the risk of exposure to the virus is high. Is there a Preventive Vaccine? – Yes, although pre-exposure vaccination does not eliminate the need for additional therapy after a rabies exposure, it simplifies therapy by eliminating the need for RIG and decreasing the number of doses of vaccine needed. Preexposure prophylaxis might protect persons whose postexposure therapy is delayed and might provide protection to persons at risk for unapparent exposures to rabies. Preexposure vaccination can be given either intramuscularly or intradermally and consists of three injections, one injection per day on days 0, 7, and 21 or 28. What are Ontario’s Ministry of Health and Long-Term Care recommendations on who should receive PreExposure vaccination? - Pre-Exposure rabies vaccination is usually recommended for those who do high risk work. What About the U.S. Food and Drug Administration Recommendations? - Preexposure vaccination should be offered to persons in high-risk groups, such as veterinarians, animal handlers, and certain laboratory workers. Veterinarians and their staff are classified in either the frequent or infrequent risk categories based on whether they are in rabies enzootic areas. Persons in the rabies enzootic areas are considered to be in the frequent-risk category and should have a serum sample tested for rabies antibody every 2 years; if the titer is less than complete neutralization at a 1:5 serum dilution by the RFFIT, the person also should receive a single booster dose of vaccine. Veterinarians, veterinary students, and animal-control and wildlife officers working in areas with low rabies rates (infrequent exposure group) do not require routine preexposure booster doses of vaccine after completion of primary preexposure vaccination. For bat exposure: In an adult, a bat landing on clothing would be considered reason for an intervention only if a bite, scratch, or saliva exposure into a wound or mucous membrane could not be ruled out. In a child, any direct contact with a bat should be considered a reason for an intervention, including contact through clothes, as a history to rule out a bite, scratch, or mucous membrane exposure may not be reliable. When a bat is found in the room with a child or an adult who is unable to give a reliable history, assessment of direct contact can be difficult. Factors indicating that direct contact may have occurred include the individual waking up crying or upset while the bat was in the room, or observation of an obvious bite or scratch mark. Intervention is defined as testing the bat for rabies, if it is available, and/or post-exposure vaccine as indicated. What Happens if Your are Exposed – What is the Vaccine Like? - If an unknown animal has bitten you and the animal cannot be quarantined, you will need post-exposure shots. You will need: one dose of immune globulin, then 5 doses of rabies vaccine over a 28 day period (days 0,3,7,14,28) after the first vaccination. The shots in the arm are almost painless - the shots previously administrated in the stomach are no longer given! How Can You Tell if the Vaccine is Still Protecting You Later in Life? - The incidence of side effects (not life threatening) does increase with booster doses. You can test to see if it is still protecting you enough to avoid a booster (2 doses over three days or, a more recently recommended single-visit, 4-site ID booster regimen). In a nutshell, to check if the antibodies are still strong in your blood: First, one mL of blood is drawn. The sample is then diluted. Titer levels, expressed as ratios, indicate how many times blood can be diluted before no antibodies are detected. If blood can be diluted a 1000 times and still show antibodies, the ratio would be 1:1000. This is a “strong” titer. A titer of 1:2 would be weak. Ontario Rabies Status Am I in an area where animals have rabies (enzootic) in southern Ontario ? – YES (though lower risk than some around the globe) Source: World Health Organization 2008 Global Map of Rabies Risk – RABIES IN ONTARIO WILDLIFE (not including bats) 2011 -- 1 case in a cow, 23 bats (as of Sept. 30, 2011) 2010 -- 10 cases (all in Grey County skunks/cluster around Mount Forest) 2009 -- 18 cases 2008 -- 41 cases 2007 -- 44 cases 2005 -- The last case of raccoon rabies (a U.S. strain) Once home to the largest concentration of terrestrial rabies in North America, Ontario has made major efforts to fight rabies since 2007 – efforts that have helped push raccoon rabies out of the province and are now being used to wipe out fox rabies. Skunks are still a challenge to vaccinate. Bat rabies is being addressed through public education campaigns. In the summer of 2011, Ontario distributed 366,000 baits containing rabies vaccine in the following [read enzootic] areas: Throughout southwestern Ontario. In the Niagara region between Welland Canal and Niagara River, including Navy Island. On Wolfe, Howe and Hill islands in St. Lawrence River as well as a small area on the mainland near Brockville. The flavoured baits immunize most skunks, foxes and raccoons that eat them. Baits are small and khaki green, with a tollfree rabies hotline number stamped on them. If you see baits, please leave them undisturbed. If a person or a pet comes in contact with the vaccine in the bait, contacting a doctor or veterinarian as a precaution is recommended. Ontario had 43% of the cases in Canada, the most affected species were bats (356/956 or 37%) and skunks (226/ 956 or 24%) E-Sources accessed October, 2011: Wikipedia Health Canada (website) Government of Ontario – Health Protection and Promotion Act (online laws), Ontario Ministry of Health and Long-Term Care Government of Ontario – Ministry of Natural Resources (website) Principles and practice of clinical virology - Arie J. Zuckerman, Jangu E. Banatvala, Paul Griffiths) U.S. Federal Drug Administration (FDA)