Curriculum for psychological interventions for people with

Curriculum for psychological interventions for people with psychosis or bipolar disorder
Anthony D. Roth, Stephen Pilling & Gemma Halliday
University College London
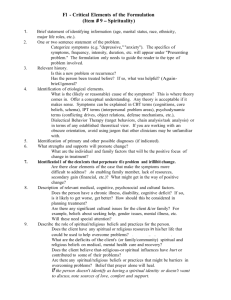
1
Curriculum for psychological interventions for people with psychosis or bipolar disorder
Anthony D. Roth, Stephen Pilling & Gemma Halliday
University College London
Background
The curriculum outlines the knowledge and skills required to deliver psychological interventions for people with psychosis and bipolar disorder. Its content is based on the competence framework for work with people with psychosis and bipolar disorder (Roth &
Pilling (2013), available online at www.ucl.ac.uk/CORE/.
The competence framework contains more detailed information regarding the knowledge and skills outlined in the curriculum, and should be cross-referenced when developing programmes.
Application
The curriculum is intended to be indicative, not prescriptive; it offers specific guidance about content, but is not intended to define how this content should be delivered or structured.
Although it could be read as suggesting a linear programme (for example, progressing from core skills through to specific interventions), there are good arguments for integrating material across units. This is especially – and critically – the case in relation to Units 2 and 6 which contain overarching competences ( ‘therapist stance, values and style’, and
‘metacompetences’). These have application across the whole framework, and while it makes sense for them to be conveyed explicitly, it is important that they are integrated with the other units (because they will influence the way in which the skills described in these units should be delivered).
The curriculum
The units of the curriculum are as follows:
UNIT 1 CORE COMPETENCES FOR WORK WITH PEOPLE WITH
PSYCHOSIS AND BIPOLAR DISORDER
Page
3
UNIT 2
UNIT 3: GENERIC THERAPEUTIC COMPETENCES
UNIT 4 ASSESSMENT AND FORMULATION
UNIT 5
THERAPIST STANCE, THERAPIST VALUES AND THERAPIST
STYLE
SPECIFIC
INTERVENTIONS
CBT FOR PSYCHOSIS
FAMILY INTERVENTIONS FOR PSYCHOSIS
AND BIPOLAR DISORDER
CBT FOR BIPOLAR DISORDER
PSYCHOEDUCATION FOR BIPOLAR
DISORDER
UNIT 6 METACOMPETENCES
10
12
18
27
40
48
62
65
Accrediting prior learning/ experience
As indicated at the head of Units 1 and 3, experienced staff may already be able to demonstrate some or all of the core, generic and assessment competences. How their skills and knowledge is assessed is for local determination, but there should be scope within programmes to accredit prior learning and experience.
2
UNIT 1
CORE COMPETENCES FOR WORK WITH PEOPLE WITH
PSYCHOSIS OR BIPOLAR DISORDER
The content of this curriculum is based on the competence framework for work with people with psychosis and bipolar disorder (Roth & Pilling (2013), published at: www.ucl.ac.uk/CORE/
The framework contains more detailed information regarding the knowledge and skills outlined in this curriculum, and should be cross-referenced when developing programmes
Introduction
All interventions with people with psychosis and bipolar disorder rest on the deployment of the core competences set out in this unit. They represent the basic underpinning to all work in this field, and need to be present for effective and safe work to take place. The term ‘core’ should not be taken to imply that these are simple competences; many of these represent complex areas of work. A better term might be ‘essential’, because without them interventions are less likely to be effective’.
Assessment of core competences in current workers
Some workers will have already covered the topics set out in this unit, either in their preregistration training or as part of their professional development. Where this is the case they should be exempted either from the whole unit, or from those parts where they have demonstrable competence. Equally, it should not be assumed that workers already possess these competences.
Overview of unit content
A. Knowledge of the range of presenting issues and diagnostic criteria in people with psychosis and bipolar disorder
B. Knowledge of, and ability to work within, relevant professional and medico-legal frameworks:
1. Knowledge of legal frameworks relating to working with people with psychosis and bipolar disorder
2. Knowledge of, and ability to operate within, professional and ethical guidelines
3. Knowledge of, and ability to work with, issues of confidentiality and consent
4. Knowledge of, and ability to assess, capacity
C. Ability to work with difference
D. Ability to work within and across organisations
3
E. Ability to engage and work with families and carers
F. Knowledge of psychopharmacology in child and adolescent work
G. Knowledge of common physical health problems in people with psychosis and bipolar disorder
General learning outcomes from the unit
At the end of the unit participants will be able to demonstrate:
1. Knowledge of the ways in which people with psychosis and bipolar disorder present, and of the usual course and development of these problems
2. Knowledge of ethical and medico-legal frameworks pertinent to work with people with psychosis and bipolar disorder and their families, and their application to clinical contexts
4. Knowledge of professional and ethical guidelines and a capacity to apply this knowledge in a clinical context
5. Knowledge of the ways in which issues of confidentiality, consent and capacity are managed in a clinical context, and a capacity to apply this knowledge in a clinical context
6. Knowledge of the ways in which the difference and diversity among service users relates to their experience, receptiveness and responsiveness to services, and how this is taken into account as part of routine practice
7. Knowledge about the factors which commonly promote and restrict inter-agency working, and a capacity to apply this knowledge in a clinical context
8. Knowledge of issues related to the process of engaging people with psychosis and bipolar disorder and their families/carers, and a capacity to apply this knowledge in a clinical context
9. Knowledge of the psychopharmacological interventions commonly offered to people with psychosis and bipolar disorder
10. Knowledge of the elevated risk for physical health problems in people with psychosis and bipolar disorder and how these can be identified and managed
Specific learning outcomes from the unit
A. Knowledge of the range of presenting issues and diagnostic criteria in people with psychosis and bipolar disorder
1.
2.
Knowledge of the ways in which psychosis and bipolar disorder presents in children/young people and in adults or older adults
Knowledge of the social, psychological, family and biological factors associated
3. with the development and maintenance of mental health problems (and specifically for factors associated with psychosis / bipolar disorder)
Knowledge of the diagnostic criteria for psychosis and for bipolar disorder specified in the main classification systems (i.e. DSM 5 and ICD-10), including
4
the key features that differentiate these diagnostic groups, and the diagnostic challenges within each group
4. Knowledge of problems which commonly co-occur with psychosis and bipolar disorder (e.g. depression, anxiety, substance misuse, personality disorder, trauma)
5. Knowledge of the incidence and prevalence of psychosis and bipolar disorder across different cultures/ethnicities/social groups
6. Knowledge of factors that promote well-being and emotional resilience (e.g. good physical health, high self-esteem, secure attachment to caregiver, higher levels of social support)
7. Knowledge of the ways in which psychosis/ bipolar disorder can impact on functioning and individual development (e.g. maintaining intimate, family and social relationships, or the capacity to maintain employment and study)
B. Knowledge of, and ability to work within, relevant ethical and medico-legal frameworks
B1. Knowledge of legal issues relating to working with people with psychosis and bipolar disorder
1. Knowledge that clinical work with people with serious and long-term mental health problems and their carers is underpinned by a legal framework, and of the relevant legislation and policies that apply to the settings in which interventions take place
2. Knowledge of relevant aspects of mental health legislation
3. Knowledge of the legal framework which determines the criteria for capacity and informed consent
4. Knowledge of equality legislation designed to protect people from discrimination when accessing services
B2. Knowledge of, and ability to operate within, professional and ethical guidelines
1.
2.
3.
Knowledge that ethical and professional guidance represents a set of principles that need to be interpreted and applied to unique clinical situations
Knowledge of relevant codes of ethics and conduct that apply to all professions, and to the profession of which the worker is a member
Knowledge of local and national policies in relation to capacity and consent, confidentiality, and data protection
4. Knowledge of procedures for identifying and minimising the potential for harm
5
5. Knowledge of legal and clinical issues related to the process of gaining consent from service users regarding consent to an intervention
6. Knowledge of legal and clinical issues related to the maintenance of confidentiality
7. Knowledge of the importance of professional boundaries and the maintenance of professional standards
8. Knowledge of the importance of maintaining standards of competence and responding to issues that threaten a practitioner ’s fitness to practise
9. Knowledge of the importance of maintaining accurate and comprehensive records and of sharing these appropriately (including with the service user/carers)
10. Knowledge of the principle that service users and carers should be actively involved in their care (e.g. be involved in care planning, have their concerns listened to, have their complains responded to without prejudice to their care)
B3. Knowledge of, and ability to work with, issues of confidentiality and consent
1.
2.
3.
Knowledge of legal definitions of consent to an intervention
Knowledge of procedures relevant to gaining consent to an intervention by service users and their carer(s)
Knowledge of the ways in which the duty of confidentiality impacts on information sharing with service users and their carer(s), or with other agencies involved in the care of the service user
4. Knowledge of the limits on the duty of confidentiality and the circumstances under which information about the service user can be shared with relevant parties
5.
6.
Knowledge of ways in which service users and their carer(s) can be informed about the practical implications of issues relating to confidentiality (for example, how information will be shared)
Knowledge about the circumstances under which information can be shared, and in a manner than conforms with relevant legal and professional guidance regarding the extent and form of any disclosure
B4. Knowledge of, and ability to assess, capacity
1. Knowledge of the legal definition of capacity of individuals to give consent to an intervention
6
2. Knowledge of procedures for assessing capacity that take into account factors that may make it hard for service users to understand or receive communication, and of strategies that can be adopted to overcome this
C. Knowledge of, and ability to practice professional skills and values
C1. Working with difference (cultural competence)
1. Knowledge of different forms of difference, and their significance for practice
2. Knowledge of social and cultural factors which may impact on access to services
3. Knowledge of the importance of communicating an interest in, and a respect for, the diversity of backgrounds from which service users and their carers are drawn
4. Knowledge of the ways of in which clinicians can gain an understanding of their clients’ experience of difference, and the ways in which this understanding can be used to guide the formulation and intervention
5. Knowledge of the ways in which communication can be adapted where service users do not share the same language as the clinician, or where they have a disability
6. Knowledge of when and how standardised assessments/measures are adapted and interpreted to take account of the demographic membership of the service user and their carer(s)
7. Knowledge of the circumstances under which social and cultural differences will have implications for the effectiveness of interventions, and the ways in which interventions can be adapted to safeguard their potential benefit
8. K nowledge of the potential impact on the therapeutic relationship of the clinician’s own background, and the ways in which this knowledge can be utilised
9. Knowledge of ways in which clinicians can identify and challenge inequality in relation to service design and delivery
C2. Ability to operate within and across organisations
1. Knowledge of the responsibilities of the worker’s own agency and of external agencies
2. Knowledge of the rationale for initiating work across organisations
7
3. Knowledge of local policies and of relevant legislation
4. Knowledge of interagency procedures
5. Ability to judge when and how it is appropriate to share information
6. Ability to communicate effectively with other agencies
7. Ability to coordinate work with other agencies
8. Ability to recognising challenges to interagency working
D. Ability to engage and communicate with families and carers
1. Knowledge of the of importance of engaging all members of the family, and of strategies for achieving this
2. Knowledge of the ways in which the language, pace and content of sessions can be adjusted in order to match the strengths, abilities and capacities of family members, and of the use of additional communication aids where this is indicated
3. Knowledge about strategies for ensuring that family members understand the nature of any interventions and any related procedures (including issues of confidentiality and consent and information-sharing)
Knowledge of the importance of sharing information appropriately with family members, and working within the rules of confidentiality to ensure relatives have the information they need to support family members and manage risk
4. Knowledge of strategies for promoting a collaborative working style with family members
5. Knowledge of factors which aid the development of a positive alliance
6. Knowledge of strategies for monitoring and responding to threats to engagement
E. Knowledge of psychopharmacology when working with people with psychosis and bipolar disorder
1. Knowledge of the role of medication in the treatment of psychosis and bipolar disorder
2. Knowledge of medications commonly prescribed in psychosis and bipolar disorder, and the conditions for which they are employed
8
3. Knowledge of evidence for the benefits of both medication-alone and medication offered in combination with psychological interventions
4. Knowledge of the potential benefits and risks of medication
5. Knowledge of how the potential role of medication can be discussed with service users and, where appropriate, their families/carers
6. Knowledge of significant side-effects of medication and strategies for supporting the service user in medication management
F. Knowledge of common physical health problems in people with psychosis and bipolar disorder, and their management
1. Knowledge of the elevated risk of poor physical health in people with psychosis and bipolar disorder and of the conditions with which they commonly present
2. Knowledge of the side-effects of anti-psychotic medication that directly contribute to physical health problems
3. Knowledge of targeted interventions aimed at improving physical health, including interventions for acute and chronic physical health conditions
4. Knowledge of potential links between symptoms of psychosis, lifestyle choices and physical health issues and the way these can be used to formulate tailored interventions
9
UNIT 2
THERAPIST STANCE, THERAPIST VALUES AND THERAPIST STYLE
The content of this curriculum is based on the competence framework for work with people with psychosis and bipolar disorder (Roth & Pilling (2013), published at: www.ucl.ac.uk/CORE/
The framework contains more detailed information regarding the knowledge and skills outlined in this curriculum, and should be cross-referenced when developing programmes
Introduction
There is a clear professional consensus that the effectiveness of work with people with psychosis and bipolar disorder is strongly influenced by the therapist’s stance, values and style. The competences in this section are not abstract ideas, but form an underpinning to the way in which interventions are delivered. As such the content needs to be embodied in
(and exemplified within) teaching of more concrete clinical skills described in other units of this curriculum (an observation that also applies to the unit setting out metacompetences).
General learning outcomes from the unit
At the end of this unit participants will be able to demonstrate knowledge and skills relating to the adoption of a therapeutic stance, therapist values and therapist style associated with good practice in the implementation of interventions with people with psychosis or bipolar disorder.
Specific learning outcomes from the unit
In what follows the term ‘client’ is used to denote both individuals, families and carers
A: Therapeutic stance
1. Ability to form a collaborative relationship with people with psychosis and bipolar disorder and with their families and carers (e.g. by respecting their choices, enabling them to have a sense of direction and control, and by drawing on their strengths)
2. Ability to work with each client to develop a shared language that embodies their model and understanding of their experience problems and concerns
3. Knowledge that unusual perceptual experiences and extremes of mood can be seen as part of the continuum of normal experience, and that it is the interpretation or appraisal of psychotic phenomena that cause distress rather than the experiences themselves
4. Ability to try to understand psychotic experiences and mood swings from a psychological perspective (e.g. by trying to comprehend and empathise with the
10
cli ent’s behaviour, viewing the client as a rational person trying to makes sense of their experiences, or seeing strategies that carers develop as ways of trying their best to manage a difficult situation)
B: Therapist values
1. Ability to hold in mind that it is not psychotic phenomena or extreme mood states/swings per se that are clinically relevant but the amount of distress, disability or risk associated with them, and wherever possible to focus an intervention on reducing distress in the those areas the client/carers identify as important
2. An ability to hold in mind that psychotic phenomena and mood swings may be functional and valued by a client
3. Ability to focus on the person in the context of their individual, cultural and spiritual preferences, and on their strengths, resources and assets
4. Ability for the practitioner to reflect on their own beliefs, attributions and assumptions about factors that contribute to recovery and relapse, and their ability to help clients to achieve the goals to which they aspire
C: Therapist style
1. Ability to maintain an open, responsive and honest therapeutic style (e.g. by using active listening skills, acknowledging when something has been misunderstood, being willing to explain the rationale for an intervention or to answer questions straightforwardly)
2. Ability to develop a relationship of mutual respect whereby the practitioner learns from client’s expertise by experience, and clients learn from the practitioner’s expertise (based on their training and clinical work) and so address the risk of clients/significant others feeling disempowered
11
UNIT 3
GENERIC THERAPEUTIC COMPETENCES
The content of this curriculum is based on the competence framework for work with people with psychosis and bipolar disorder (Roth & Pilling (2013), published at: www.ucl.ac.uk/CORE/
The framework contains more detailed information regarding the knowledge and skills outlined in this curriculum, and should be cross-referenced when developing programmes
Introduction
Psychological interventions for people with psychosis or bipolar disorder are underpinned by a set of generic therapeutic competences that apply to all modalities of therapy, and are highly relevant to their effective delivery.
Assessment of generic therapeutic competences in current workers
Some workers will have already covered the topics set out in this unit, either in their preregistration training or as part of their professional development. Where this is the case they should be exempted either from the whole unit, or from those parts where they have demonstrable competence. Equally, it should not be assumed that workers already possess these competences.
Overview of unit content
A. Knowledge of models of intervention and their employment in practice
B. Ability to foster and maintain a good therapeutic alliance, and to grasp the client’s perspective and ‘world view’
C. Ability to deal with the emotional content of sessions
D. Ability to manage endings and service transitions
E. Ability to make use of measures (including monitoring of outcomes)
F. Ability to make use of supervision
G. Ability to deliver group-based interventions
12
General learning outcomes from the unit
At the end of the unit participants will be able to demonstrate:
1. Knowledge of the therapeutic models being employed in services
2. Knowledge of the therapeutic alliance, and an ability to act on this knowledge to develop and maintain a therapeutic alliance with clients, and to identify and address any stains that develop in the alliance in the course of an intervention
3. An ability to manage the emotional content of sessions, by helping clients to identify and articulate their emotions, and by structuring sessions and responding to clients in a manner that allows for the expression and management of strong emotions
4. An ability to manage planned and unplanned endings and transitions from one service to another
5. An ability to make use of measures both as a part of the process of assessment and in order to track the progress that clients are making
6. An ability to make use of supervision as an active participant
7. An ability to apply knowledge of group processes to the delivery of interventions in a group format
Specific learning outcomes from the unit note that throughout the term ‘client’ is used to denote all potential parties to the intervention – i.e. the service user, and their family/ carers
A. Knowledge of models of intervention and their employment in practice
1. Knowledge of the theory and principles underpinning therapeutic models relevant to people with psychosis and bipolar disorder, and particularly those applied in the setting within which the practitioner is working (e.g behavioural, cognitive behavioural and family therapies)
2. Knowledge of the evidence base as it relates to the models employed in services
3. Knowledge of factors common to all therapeutic approaches (e.g. offering support, creating opportunities for learning, and for putting ideas into practice)
4. Ability to apply the principles underlying the intervention being applied (i.e. using these principles to inform the application of the specific techniques which characterise the model)
B. Ability to foster and maintain a good therapeutic alliance, and to grasp the client’s perspective and ‘world view’
1. Knowledge of the three components of the therapeutic alliance seen as contributing to the maintenance of the alliance (i.e. bonds, tasks and goals)
13
2. Knowledge of therapist factors commonly associated with the promotion of the alliance and an ability to ensure that these are present when interacting with clients
3. Knowledge of therapist factors which reduce the probability of forming a positive alliance and an increased sensitivity to these factors in people with psychosis and bipolar disorder, and an ability to ensure that these are absent or appropriately managed when interacting with clients
4. Knowledge of client factors which may affect the probability of forming a positive alliance in people with psychosis and bipolar disorder
5. A bility to listen to the client’s concerns in a manner which is non-judgmental, supportive and sensitive, and which conveys a comfortable attitude when the client describes their experience
6. Ability to gauge whether the client understands the rationale for the intervention and to help them articulate any concerns or queries
7. Ability (where appropriate) to normalise and validate the client’s concerns and experiences
8. Ability to apprehend the ways in which the client characteristically understands themselves and the world and to aid the establishment of their ‘world view’ with openness and acceptance
9. Ability to recognise when strains in the alliance threaten the progress of therapy and to actively deploy appropriate remedial actions both to detect and address the likely causes of these strains
B. Ability to deal with the emotional content of sessions
1. Ability to manage strong emotions which interfere with effective change, by:
helping the client process emotions, by acknowledging and/or containing emotional levels that are too high (e.g. anger, fear, despair) or too low (e.g. apathy, low motivation) and distinguishing expression of strong affect from possible indicators of relapse
helping the client express their feelings while also being alert to the risk that strong affects may exacerbate both positive and negative symptoms
monitorin g the client’s tolerance of emotional expression
offering in-session strategies that help to manage any emotional difficulties that emerge
introducing techniques designed to manage strong emotions (such as aggressive behaviour) and indicating where behaviour is socially appropriate or inappropriate
helping families/carers to support the client’s capacity to express emotion in an appropriate manner in the session (and vice-versa)
2. Ability to elicit emotions that facilitate change by helping the client access, differentiate and experience their emotions
14
3. Ability to reflect on the meaning and communicative intent of the behaviour/emotional expression and its relation to the current and past context
C. Ability to manage endings and service transitions
1. Knowledge of national and local guidance on the assessment of any risks relating to clients ending contact with a service (including guidance that relates to risk assessment and management, or consent, confidentiality and information sharing)
2. Ability to work collaboratively with the client in order to plan and to manage termination and set in place any future support
3. Ability to work with planned endings by:
clearly signalling the ending to the client throughout the intervention
helping clients to express their feelings about termination
exploring client’s feelings about the ending (especially where these have implications for their capacity to manage the ending)
reviewing/ reflecting on the therapy and developing a relapse prevention plan
preparing the client for any transition to another service
4. Ability to work with premature or unplanned terminations, by:
(where possible), exploring with the client and (where working with families/carers) the family/carer(s) their reasons for terminating contact earlier than planned
exploring whether concerns about the intervention or service can be addressed
assessing any risk to the client and their family/carer(s) from early termination
reviewing contact with the client (verbally or through a discharge letter)
D. Ability to select and use, appropriate outcome measurement
1. Knowledge of commonly used assessment measures for people with psychosis and bipolar disorder and their specific focus and purpose (including measures assessing risk and client experience and use of services)
2. Knowledge of the importance of assessing outcomes for family members/ carers as well as the service user
3. Knowledge relevant to the application of a measure (e.g. psychometric properties, scoring and interpretation procedures, characteristics of the test that may influence its use (e.g. brevity, ‘user-friendliness’ etc)
4. Ability to identify when clients have difficulty completing measures (e.g. due to literacy problems or not speaking English as a first language) and to know when and
5. An ability to integrate outcome measurement into the intervention or treatment programme how to assist them
15
6. Ability to use systematic diary recordings to help identify the function of a specific behaviours (by analysing its antecedents and consequences) and to integrate these into assessment and intervention
E. Ability to make use of supervision and training
1. Ability to recognise when operating beyond current level of competence, training or capacity, and to respond to this by seeking supervision and/or further training
2. Ability to work collaboratively with the supervisor:
to generate an explicit agreement about the parameters of supervision
to present an honest and open account of clinical work undertaken
to discuss clinical work as an active and engaged participant (i.e. without becoming passive or avoidant, or defensive or aggressive)
to present clinical material to the supervisor in a focussed manner, selecting the most important and relevant material
3.
Ability to reflect on the supervisor’s feedback and to apply these reflections in future work
4. Ability to reflect on beliefs about clients and to identify and work on any beliefs that may be unhelpful to the progress of an intervention
5. Ability to act on suggestions regarding relevant reading made by the supervisor, and to incorporate this material into clinical practice
6. Ability to use supervision to discuss the personal impact of the work, especially where this reflection is relevant to maintaining the likely effectiveness of clinical work
7. Ability to reflect on the quality of supervision as a whole, and (in accordance with national and professional guidelines) to seek advice from others where there is concern that supervision is below an acceptable standard where the supervisor’s recommendations or behaviour deviate from acceptable practice
F. Ability to deliver group-based interventions
1. Ability to recruit clients to the group by discussing the appropriateness of the group and possible barriers to participation
2. Ability to negotiate individualised goals with each group member
3. Ability to implement components of the group therapy model (and adhering to the manual where groups are manualised)
4. Ability to establish a physically and emotionally safe group environment and manage emotional or physical risk to group leaders and participants
5. Ability to engage group members (e.g. matching content and pacing to group member characteristics, building a positive rapport with individuals, ensuring participation of all members, using social reinforcement to encourage participation)
16
6. Ability to manage potential challenges to group engagement (e.g. disruptive behaviour, persistent non-engagement, dominating group members or high distress or expressed emotion)
7. Ability to help clients prepare for the ending of a group intervention (e.g. by signalling endings, aiding expression of feelings about group ending, reviewing themes covered in the group or reflecting on group progress)
8. Ability to evaluate the group (e.g. by employing appropriate strategies and tools, reviewing client goals, and feeding back evaluation sensitively and meaningfully)
17
UNIT 4
ASSESSMENT AND FORMULATION
The content of this curriculum is based on the competence framework for work with people with psychosis and bipolar disorder (Roth & Pilling (2013), published at: www.ucl.ac.uk/CORE/
The framework contains more detailed information regarding the knowledge and skills outlined in this curriculum, and should be cross-referenced when developing programmes
Introduction
Assessment and formulation represent a core (though often complex) areas of activity.
People with psychosis or bipolar disorder often present to services in ways that do not map neatly to single diagnostic groupings, have problems in a number of different areas of functioning, and may well function very differently in differing contexts. Gaining a clear understanding of their needs is critical; even more so is the ability to use assessment information to derive a formulation that can be used to guide decisions about which interventions should be offered, by whom, and by which agencies. The capacity to direct service users and their families and carers to the care that is most likely to be effective (and that they themselves feel is the right approach) should be seen as a central aspect of the care they receive.
Assessment and formulation can vary considerably in their scope and level of detail, and it is important to hold in mind the function to which assessment and formulation is being put - it is this that should determine the level of detail and depth that is required in order to progress to an intervention.
Overview of unit content
A. Ability to undertake a comprehensive assessment
B Ability to undertake a risk assessment and to manage risk
C. Abi lity to assess the child/young person’s functioning across systems
D. Ability to develop a formulation
E. Ability to feedback the results of an assessment to children/young people and their family/carers, and to agree a treatment plan
F. Ability to co-ordinate casework or interventions across different agencies
General learning outcomes from the units
At the end of the unit participants will be able to demonstrate the set of competences that define the assessment process:
18
1. The knowledge and skills required to undertake a comprehensive assessment of the problems and needs, as well as the strengths and resources, of people with psychosis and bipolar disorder and their families/carers
2. The knowledge and skills required to undertake an assessment of any risks to the service user or to others, and to respond to any risks that are identified
3. The knowledge and skills required to assess the ways the service user’s functioning across the “systems” in which they live
4. An ability to integrate assessment information to derive a formulation of the presenting problems, and identify appropriate and effective intervention strategies
5. An ability to feedback the results of the assessment process, and of the formulation that emerges, to the service user and their families/carers
6. An ability to coordinate casework within and across agencies
Specific learning outcomes from the unit
A. Ability to undertake a comprehensive assessment
1. Ability to adopt a basic stance throughout assessment that is collaborative and which:
takes into account the client’s history and social/cultural context
prioritises the client’s understanding of their experiences and issues they identify as most salient and distressing
recognises the adverse impacts of stigma across various domains and sense of self
considers the client’s strength and resources when planning intervention
2. Knowledge of recovery models and their guiding principles
3. Ability to move flexibly between assessment and engagement in response to shifting client states and to adapt the pace, structure and content of assessment to meet the client’s needs and priorities
4. Ability to engage the client in the assessment process by:
explaining the purpose of assessment and therapist’s role
discussing any concerns the client has about the assessment
normalising and validating the client’s experiences
5. Ability to apply knowledge of ethical and legal issues relating to confidentiality, consent and capacity
6. Ability to maintain professional boundaries while also maintaining appropriate levels of personal contact
7. Ability to attend to (and where appropriate to adopt) the language used by the client to describe their experience
19
8. Ability to distinguish between what the client experiences and their inferences regarding these experiences
9. Ability to appraise referral and background information with regard to its relevance and its reliability
10. Ability to assess the client’s history and current circumstances, including their:
developmental and family history
relationship history and interpersonal functioning
stability and appropriateness of the client’s home and living circumstances
financial circumstances
history of support (including changes over time)
physical health
11. Knowledge of anomalous experiences and ability to enquire about them
12. Knowledge of delusional beliefs and ability to enquire about them, including:
their specific content, meaning and level of conviction, preoccupation and the distress associated with the beliefs
antecedent and maintaining factors, including “safety behaviours”, and consequences of “activating” the belief
13. Ability to enquire about voices and the factors that trigger them, their form and content, beliefs about, and relationship with the voice, and their emotional and functional impact
14. Ability to draw on knowledge of negative symptoms in order to observe and enquire about them
15. Ability to draw on knowledge of perceptual disturbances in order to observe and enquire about depersonalisation, derealisation, changes in perception
16. Ability to draw on knowledge of motor and behavioural disturbances in order to
17. Ability to assess coexisting emotional or mental health difficulties, and to consider how these interact with, and impact on, psychotic symptoms observe and enquire about them (e.g. reduced or increased motor activity, reduced non-verbal expression, unusual mannerisms, appearance or behaviours)
18. Ability to assess current and past physical health issues and sleep problems, and to identify any conditions for which treatment is not being offered
19. Ability to assess the client’s history of, and current contact with, services (including forensic services) and discuss their experience and attitudes towards specific
20. Ability to draw on knowledge of relevant interview-based and self-report assessment measures interventions
20
21. Ability to involve all relevant significant others, carers, and other service providers in the assessment process
22. Ability to communicate the outcome of assessment (including formulations and intervention plans) to service users, their carers and families and non-professional colleagues clearly, comprehensibly and appropriately
B. Ability to undertake a risk assessment and to manage risk
1. Ability to conduct a structured risk assessment (including risk of self-harm, selfneglect or harm to others), drawing on information from all relevant sources of information (e.g. clinical interviews, measures, observations and other agencies)
2. Ability to conduct a risk assessment that gauges the likelihood, type and severity and of a harmful/negative event
3. Ability to monitor and assess risk in clients whose presentation and mental state may vary markedly from day to day and/or be extreme and challenging
4. Ability to consider whether any assumptions or stereotypes about particular demographic groups (rather than knowledge of researched risk factors) lead to underestimation or over-estimation of actual risk
5. Ability to develop a risk formulation which identifies factors which are likely to increase or decrease risk , and to create a risk management plan based on this formulation
6. Ability to communicate the risk management plan to clients, relevant others and relevant agencies, including information on the potential benefits and risks of a decision, and the reasons for a particular plan
C. Ability to assess the person’s functioning across systems
1. Knowledge of the multiple contexts that need to be considered in any assessment, and the ways these are likely to interact with each other and may be relevant to the client’s presentation, for example,:
their significant relationships (e.g., partner, family, close friends, peers)
the professional network(s) involved with the client
their cultural setting
2. Ability to gather information relevant to the client from significant members of the system (e.g., client’s partner and family, carers, other professionals), to collectively identify:
perceived problem areas and the beliefs concerning them
potential strengths of the client (and the wider system) which may support therapeutic change
solutions that have been tried or have been considered
21
D. Ability to develop a formulation
1. Knowledge of the usual content of formulations (i.e. a set of hypotheses or plausible explanations which draw on theory and research to explain the details of the clinical presentation obtained through an assessment)
2. Knowledge of “generic” formulations (drawing on biological, psychological and social theory and research, and including consideration of risk factors, precipitating factors, maintaining factors, and protective factors) and of “model-specific” formulations
3. Ability to develop an intervention plan that is based on the formulation
4. Ability to construct a formulation by evaluating and integrating assessment information obtained from multiple sources and methods, and identifying factors which significantly influence the development of the presenting problem(s)
5. Ability to appraise and resolve contradictory reports of a problem (e.g., where informants differ in focus or problem representation, or where client behaviour is context-dependent)
E. Ability to feedback the results of an assessment and formulation and to agree a treatment plan
1. Ability to communicate the outcomes of assessment and the formulation to service users
2. Ability to adapt the way that information is conveyed to the client’s level of understanding and emotional readiness to accept it (and to adapt written information for people with a sensory disability)
3. Ability to check that the client (and where relevant significant others) understand information conveyed, and to structure sessions to allow them to indicate whether they agree and to feel able to ask any questions
4. Ability to openly explore reasons for any significant differences between the clinician’s view of the diagnosis or formulation and that of the client (and where relevant, that of significant others)
5. Ability to plan an intervention that draws on the agreed formulation, is congruent with current research knowledge, and with the resources available to the service
6. Ability to promote informed choice by providing information on any alternative intervention options, their likely efficacy, and to seek the clien t’s views and preferences
7. Ability to help the client to identify goals for the intervention(s) that are explicitly defined, realistic and prioritised by areas of functioning most amenable to change
22
8. Ability to choose appropriate measures to evaluate and monitor progress
F. Ability to collaboratively engage the client with the treatment model
1. Ability to engage the client in a collaborative discussion of the treatment options open to them, informed by assessment, formulation and the client’s aims and goals
2. Ability to ensure that clients understand the models or approaches being offered to them (i.e. the broad content of each intervention and the way an intervention usually progresses)
3. Ability to maintain a positive stance whilst conveying a realistic sense of the effectiveness, scope and challenges associated with each intervention
4. Ability to use clinical judgment to determine whether the client’s agreement to pursue an intervention is based on a collaborative choice (rather than a passive agreement, or an agreement they experience as imposed on them)
G. Ability to co-ordinate casework or intervention across agencies and/or individuals
1. Ability to effectively communicate with, and refer to, professionals within and across agencies and, where differences in perspectives are evident, to act on implications for effective intervention delivery
2. Ability to establish cross-agency casework by agreeing the roles/responsibilities of other agencies involved, gathering and sharing information, and identifying the service co-ordinating the overall plan
3. Ability to share information on a “need to know” basis to support partner agencies in understanding and recognising areas of risk and the implications for their work
4. Ability to develop a shared understanding of the ways in which agencies employing different language, definitions, customs and practise will respond to events (e.g. procedures for following-up concerns, or for escalating response in response to evidence of risk) and manage problems arising as a result of difference
5. Ability to ensure that the service user and/or their family are informed of outcomes from interagency discussions (and included in discussions where appropriate) and supported in decisions regarding engagement with partner agencies
6. Ability to update other agencies on changes to the current formulation and intervention plan, acting as a conduit for information exchange where appropriate
7. Ability to proactively monitor the activity of other agencies and to challenge them if they do not meet agreed responsibilities
23
8. Ability to recognise when the service user’s needs (across the domains of health, , physical, emotional, social functioning) are not being met by the current intervention, and where the involvement of other agencies would be beneficial to their welfare
9. Ability to inform all relevant agencies where there is an intention to discharge the service user, ensure that partner agencies are aware of current risk levels and have appropriate plans and monitoring in place
24
UNIT 5
COGNITIVE BEHAVIOURAL THERAPY FOR PSYCHOSIS (CBTp)
The content of this curriculum is based on the competence framework for work with people with psychosis and bipolar disorder (Roth & Pilling (2013), published at: www.ucl.ac.uk/CORE/
The framework contains more detailed information regarding the knowledge and skills outlined in this curriculum, and should be cross-referenced when developing programmes
Introduction
This unit outlines the knowledge and skills required to carry out CBT for people with psychosis (CBTp).
Effective delivery of CBTp rests on knowledge of (and experience in applying) the techniques of cognitive behaviour therapy. This is because CBTp requires practitioners to be fluent in these skills. Further, CBTp often focuses on common coexisting presentations (such mood disorders, anxiety, worry or sleep dysregulation) that are thought to promote psychotic symptoms. As such the learning outcomes described below build on (and assume) the knowledge and skills set out in the CBT competence framework (accessed at www.ucl.ac.uk/CORE/ ).
General learning outcomes
At the end of this unit participants will be able to demonstrate knowledge and skills relating to the following areas:
A. Knowledge of CBTp and its implementation
B. Engagement in CBPp
C. Assessment for CBTp
D. Formulation and treatment planning
E. CBTp intervention strategies
F. Affect regulation
G. Activity monitoring, scheduling and working with withdrawal
H. Working with safety behaviours/coping strategies
I. Planning and conducting behavioural experiments
J. Working with beliefs: a. working with core and metacognitive beliefs b. specific interventions for delusional and paranoid beliefs, and beliefs about voices
K. Working with thought disorder
L. Problems in social functioning (negative symptoms)
M. Trauma
N. Staying or keeping well (relapse prevention)
25
Specific learning outcomes
A. Knowledge of CBTp and its implementation
1. Knowledge that CBTp and all associated activities take place within the context of a collaborative working relationship
2. Knowledge that the central focus of CBTp is to identify a maintenance model explaining the factors driving and maintaining an individual client’s distress and dysfunction
3. Knowledge tha t assessment and formulation of a client’s difficulties determines the degree to which the maintenance model focuses on proximal and/or distal
(developmental) maintaining factors
4. Knowledge of the usual sequence in which the components of CBTp are delivered, along with an awareness that this varies depending on the formulation for each individual client e.g: a) engagement (e.g. focusing on coping skills, normalisation/validation, affect regulation, collaborative identification of goals and disadvantages and advantages associated with change, instilling hope and optimism) b) graded work on symptoms (e.g. verbal evaluation followed by the introduction of behavioural experiments) c) identification and evaluation of core beliefs regarding the self and others d) focusing on ending (e.g. relapse prevention, supporting client selfunderstanding and sense of empowerment, social functioning, social support and relationships)
5. Knowledge that the phases of CBTp (engagement, assessment, formulation and intervention) are ‘iterative’ and so need to be delivered flexibly (rather than linearly)
6. Knowledge that the content of CBTp should differ for clients who are in, or close to, an acute episode and individuals between episodes (e.g. where “meaningmaking” may be more appropriate and relevant)
7. Knowledge that the length of time devoted to an initial assessment/ formulation will vary markedly (for example, in relation to progress in building therapeutic alliance, or the client’s needs, capacities and concerns)
8. Knowledge of ways in which difficulties in cognitive functioning (e.g., in memory or attention) and/or intellectual functioning can influence the client’s presentation and capacities, and an ability to make appropriate adjustments to accommodate these
9. Knowledge of information processing biases and distortions commonly observed in cognitive therapy and relevant to the formation of delusional belief
B. Engagement in CBTp
B.1 Building a collaborative approach
1. Ability to orient the client to the content of assessment (e.g. that this will focus on the past as well as the present, will consider their experiences in some detail) and to check that this conforms to their needs and expectations
26
2. Ability to convey the reasons for undertaking a careful assessment before trying to initiate change
3. Ability to judge whether/when to introduce discrete CBT change techniques if this is likely to promote engagement through early gains
4. Ability to foster a positive alliance with the client (e.g. by encouraging discussion of their experiences, maintaining an empathic position, showing that their comments are taken seriously regardless of content, validating their experience)
B.2 Responding when the client is suspicious or hostile to the practitioner
1. Knowledge of factors like ly to influence the client’s receptiveness to assessment and continued therapy (e.g., mental state, past experience of and attitude towards services, expectation of clinician beliefs)
2. Ability to counter negative beliefs or suspicions the client may have about the therapist (e.g., understanding (rather than reacting to) hostility, judicious use of selfdisclosure, patience/persistence where the client presents as paranoid or reticent )
3. Ability to maintain awareness of the impact of nonverbal communications when a client presents as paranoid and/or aggressive (e.g., taking care not to mirror a client’s body language)
4. Ability to anticipate that voices may be commenting negatively on the therapist (e.g. through explicit discussion of this possibility, collaboratively developing management strategies where voices make it hard to proceed)
5. With clients for whom normalisation is appropriate, an ability to help clients
“normalise” psychotic experiences and beliefs (e.g., by discussing the prevalence of hear ing voices in the general population and the concept of a “continuum” of experience)
B.3 Adapting content to the individual client
1. Ability to personalise and adapt session content and the way that information is conveyed (i.e. in a way that is responsive to the client’s state of mind and capacities)
2. Ability to ‘check-in’ regularly with the client to determine the helpfulness of session content, (e.g. checking their readiness to discuss new areas or strategies, or their capacity to manage emotional discomfort), and to change tack as required
3. Ability to help the client retain a sense of shared control over sessions (e.g. by being willing to stay with neutral topics of discussion, being flexible around session setting, finding a shared language or using a recovery oriented stance)
B.4 Managing emotions
1. Ability to help the client ‘regulate’ affect in session (e.g. by collaboratively deciding when to explore sensitive areas and when to redirect discussion, making it clear that the client has control over whether to stop or continue)
2. Ability to help the client access, differentiate and experience their emotions in a way that is likely to facilitate change (e.g. by acknowledging and containing emotional
27
levels that are too high (e.g. anger, fear, despair) or too low (e.g. apathy, low motivation)
3. Ability to work with emotional issues that interfere with effective change (e.g. hostility, anxiety, excessive anger, avoidance of strong affect)
C. Assessment for CBTp
C.1 Knowledge of the scope of an assessment
1. Knowledge of the scope of assessment (usually covering the client’s experiences of psychosis, ‘anomalous experiences’, co-occurring affective and cognitive difficulties and associated metacognitive beliefs)
2. Knowledge of the broad domains usually included in an assessment – for example:
cognitive, affective, behavioural and physiological components of any difficulties
an open exploration of beliefs and attitudes about medication
use of drugs and other risky behaviours
level of functioning (e.g. coping strategies, activities of daily living, engagement in pleasurable activities)
interpersonal functioning (e.g. social and family functioning, degree of social support)
‘external’ stressors (e.g. financial problems, or abusive others)
an appraisal of strengths and the resources available to the client
3. Knowledge of likely inter-relationships between different components of the client’s presentation (e.g. managing distress associated with auditory hallucinations by taking street drugs; social isolation leading to more frequent auditory hallucinations)
C.2 Flexibility
1. Ability to adopt the order in which information is collected in response to cues from the client, and undertaking assessment in a manner congruent with the client’s
‘recovery style’
C.3 Assessin g the client’s history and circumstances
1. Ability to undertake a detailed assessment of the client’s first episode of psychosis to clarify the origins of their past and present beliefs (potentially drawing on any relevant records and informants (such as family members))
2. Ability to set up and make use of behavioural experiments to clarify areas of assessment that may be hard for the client to articulate (e.g. carrying out an activity that makes the client anxious in order to help them determine their responses)
3. Ability to work with the client to undertake a ‘recent incident analysis’ that identifies links between events, thoughts, feelings and subsequent behaviours
4. Ability to conduct a functional analysis (e.g. of functional relationships between a specified set of target behaviours or experiences, such as delusional beliefs))
28
5. Ability to assess core beliefs (e.g. by exploring events within the therapeutic relationship, or undertaking a thematic analysis of automatic thought records)
6. Ability to unde rtake “thought chaining” (e.g. working on the basis that the client’s inferences are true and to consider the implications of this, ‘chaining’ thoughts so as to progress from surface inferences through to a deeper evaluation)
7. Ability to help the client translate vague or abstract complaints into concrete and discrete problems and to prioritise target problems (usually those most distressing/amenable to change)
8. Ability to assess and act on any indicators of risk that emerge during the assessment
C.4 Dete cting and responding to the client’s cognitive and emotional capacities
1.
Ability to identify potential cognitive deficits (e.g. poor ‘processing speed’, or low levels of intellectual functioning) and to appraise their likely impact on day-to-day functioning and on any intervention
2.
Ability to gauge the client’s capacity to think about themselves psychologically and their ‘stress tolerance’, and to respond to emotional and cognitive capacities by adapting session pacing, order and content
C.5 Coping behaviours and safety behaviours
1. Knowledge of the positive and negative consequences of coping strategies that clients develop to manage their symptoms (e.g. avoidance of social settings helping to reduce symptoms, but also leading to social isolation)
2. Ability to distinguish coping behaviours (which have a sustained positive benefit) from overt and covert ‘safety-behaviours’ (which can be unhelpful in the longer term), usually by appraising their functional impact
C.6 Using measures and diaries
1. Ability to help the client keep (and have a sense of ownership over) a diary/log of specified difficulties, and to develop a shared understanding of the relevance of diary completion to personal goal achievement
2. Ability to select and use standardised and personalised measures appropriate to the client’s difficulties and capacities (e.g. reading ability and concentration), establishing a baseline and re-administering measures at appropriate intervals
D. Formulation and treatment planning
1. Ability to take into account the nature and scope of the intervention that is planned in order to decide (in collaboration with the client) the degree to which the formulation needs to consider both distal and proximal events, and the level of detail that is required
29
2. Ability to draw on knowledge of evidence-based cognitive models to create a clientspecific conceptualisation that:
accounts for the development and maintenance of symptoms and problems
links the client’s presentation with core beliefs and the attributional biases that underpin them
identifies events or experiences (including affects) that activate unhelpful beliefs
3. Ability to include consideration of the client’s long-standing beliefs about themselves and others (including the therapist) and the impact of current unusual experiences and beliefs upon such beliefs
D.1 Sharing the formulation
1. Ability to discuss the formulation with the client with the aim of helping them to begin:
considering alternative ways of understanding delusional beliefs
gaining an appreciation of the history, triggers and maintaining features of their problems and how this might be relevant to achieving their goals
identify and discuss any predictable difficulties in implementing therapy
2. Ability to monitor and manage any strong positive or negative reactions clients have to the formulation
3. Ability to agree a shared understanding of the development of the client’s psychotic symptoms, using the cognitive model to explain links between problems, interpretations and emotional and behavioural responses
4. Ability recognise when working within a delusional system or set of cultural beliefs may be necessary initially
5.
Ability to develop the client’s understanding of the cognitive model by “socializing” them to it using examples based on their own material
6. Ability to gauge whether the client understands the rationale for intervention, has questions or (for example) is sceptical about it, responding to concerns openly and non-defensively
D.2 Using the formulation to plan treatment
1. Ability to collaboratively develop a treatment plan that:
identifies the goals of the intervention
is directly linked to the hypotheses contained in the formulation
identifies likely obstacles to implementation and helps to guide the therapist’s response to their emergence
aims to promote an experience of success (e.g. by focusing initially on less distressing and/or more malleable problems, thoughts and beliefs)
2. Ability to select cognitive and/or behavioural change strategies, based on their acceptability to the client, and (based on the formulation) their likelihood of success
30
3. Ability to formulate a therapy plan for each session (e.g. that helps the client to identify and modify unhelpful or dysfunctional thinking, ideation and behaviour)
4. Ability to address factors that the formulation identifies as a threat to efficacy, (e.g. referring the client for family work or for neuropsychological testing)
5.
Ability to revise and update the formulation (and hence the treatment plan) in the light of newly emerging clinical information
6.
Ability to use the formulation to identify when CBT may not be appropriate or the best option, and to discuss this with the client (e.g., where the client’s difficulties are not primarily psychological or they indicate preference for an alternative approach)
E. CBTp intervention strategies
E.1 General CBT strategies – maintaining engagement
1. Ability to be alert (and responsive to) the risk that the intensity of affect may challenge the client’s capacity to stay in therapy
2. Ability to respond where clients are hypervigilant for signs that the therapist does not believe them or is part of their mistreatment/ persecution (e.g. by eliciting feedback from the client and responding openly and non-defensively)
3. Ability to maintain a consistently collaborative stance, working at the client’s pace and in line with their readiness to change
4. Ability to ensure that clients are ready for (and willing to engage in) an intervention strategy by checking their agreement to proceed throughout the intervention
E.2 General CBT strategies – homework
1. Ability to integrate practice assignments (homework) into therapy (by offering the client a clear rationale for their use and by ensuring they can feedback their understanding of and attitude towards homework
2. Ability to tailor homework to the individual client, ensuring it is appropriate to the stage of therapy and in line with the case conceptualisation
3. Ability to work with the client to agree appropriate and manageable homework tasks, identifying clear and specific goals that are linked to the content of sessions
4. Ability to work with the client to identify strategies which make it more likely that homework tasks are completed and to identify any reasons for non-completion
5. Ability consistently to review homework in subsequent sessions, helping the client appraise outcomes against their prior expectations, and building on this learning to identify further homework assignments
31
F. Enhancing coping skills, psychoeducation and normalisation
F.1 Enhancing coping skills
1. Ability to help the client use coping strategies to manage specific symptoms (e.g. using behavioural strategies (such as increasing their activity levels) or cognitive strategies (such as attention switching or practising positive self-talk)
2. Ability to help the client to practise coping strategies in sessions and through homework, and to adapt these strategies based on their experience of applying them
3. Ability to ensure that both therapist and client remain alert to the risk that coping strategies are adopted as safety behaviours
F.2 Psychoeducation
1. Knowledge that because psychoeducation is not usually effective as a standalone intervention in people with psychosis it should be delivered as part of a CBT intervention
2.
Ability to tailor psychoeducation to the client’s need (e.g. relating it to the difficulties they are experiencing, to the explanatory models to which they subscribe, and the extent to which these models are flexible or fixed)
3. Ability to monitor any distress arising from psychoeducation and to help decrease this (e.g. by linking explanatory models (such as the stress-vulnerability model) to their experiences)
F.3 Normalisation
1. Knowledge that while normalisation may reduce distress in clients who hold beliefs about their experiences being abnormal, it is inappropriate and unhelpful for clients who hold beliefs that they are unique and special
2. Ability to ‘decatastrophise’ the client’s experiences by discussing the ways in which similar psychological processes or experiences occur (or could be triggered) in the general population (aiming (for example) to promote their understanding of symptoms, or improve self-esteem)
3. Ability to ensure that a normalising stance does not ignore or minimise the degree of distress experienced by the client
G. Affect regulation
1. Ability to observe and enquire about affective issues and concerns impacting on the client (e.g., depression, anxiety and worry, affective issues linked to past psychotic experience, anger) and to work collaboratively to manage distress by drawing on appropriate cognitive behavioural techniques
32
H. Activity monitoring, scheduling and working with withdrawal
H.1 Activity monitoring and scheduling
1. Ability to help the client complete and review activity charts (to identify activity patterns, over- or under-represented activities and activities associated with high or low levels of pleasure and mastery)
2. Ability to work with the client to identify and plan specific changes to activities, identifying thoughts (assumptions or beliefs) which may make implementation difficult
3. Ability to use activity charts to help clients schedule activities (e.g. pleasurable activities or previously avoided activities) and to record their predicted and actual levels of pleasure and mastery
H.2 Addressing social withdrawal
1. Ability to help the client use diaries, behavioural experiments and activity scheduling to identify any links between inactivity, low mood, and unusual beliefs
(and hallucinations)
2. Ability to help the client reflect upon the function that social withdrawal plays in their lives, and its pros and cons (e.g. withdrawal may help to decrease paranoid thoughts but may increase depression)
3. Ability to work with the client to identify areas where focusing on or adapting their social skills might be helpful (e.g. to facilitate social contact)
4. Ability to help clients who completely avoid social situations to consider how they could engage in more ‘strategic’ avoidance (e.g. balancing attempts to reduce symptoms against improving their quality of life)
5. Ability to collaboratively identify individuals within the client’s social network who could provide support or act as a confidant (including helping to reinitiate contact with estranged individuals)
I. Working with safety behaviours/coping strategies
1. Ability to work collaboratively to differentiate safety behaviours from coping strategies (guided by their function and consequences) and identify how safety behaviours maintain distress/impaired functioning
2. Ability to work with the client to consider more functional alternatives to safety behaviours, ensuring their sense of risk and distress remain manageable during the process
3. Ability to help clients to be aware of the potential role of residual safety-seeking behaviours in relapse
33
J. Planning and conducting behavioural experiments
J.1 Planning conducting and reviewing behavioural experiments
1. Ability to devise behavioural experiments and to ensure that their form, timing and content are congruent with their intended aim
2. Ability to plan experiments collaboratively so as to make sure that any concerns/reservations held by the client are fully accounted for
3. Ability to check the client’s understanding of the cognitions being targeted, and to help them anticipate possible problems
4. Ability to help the client anticipate their likely reactions should the experiment confirm their fears, and ways of overcoming these
5. Ability to help the client appraise their reactions to the experiment (.e.g by recording the outcome (whether positive or negative) and identify its impact on their thinking or behaviour)
Working with beliefs
K. Working with core and metacognitive beliefs
1. Knowledge that (because core beliefs can underpin psychotic symptoms) direct core-belief work can reduce distress/dysfunction
2. Knowledge that core belief work can focus on challenging negative self-schema and on creating positive, self-schema, and/or helping clients to accept that both are valid parts of their sense of self
3. Ability to identify metacognitive beliefs (such as worry, rumination or paranoia) and their contribution to the maintenance of the client’s difficulties
4. Ability to work collaboratively to consider the utility of metacognitive beliefs (e.g. by weighing up their advantages and disadvantages, challenging beliefs (e.g. through behavioural experiments))
L. Specific interventions for delusional and paranoid beliefs and beliefs about voices
L.1 Knowledge of delusional beliefs
1. Knowledge of the characteristics of delusional beliefs
2. Knowledge that querying the basis of delusional beliefs should only take place once the therapist has a thorough understanding of their content and
34
consequences (and therefore a sound basis for commencing Socratic dialogue about the belief)
3. Knowledge that beliefs may be shaped by difficulties in social understanding, which may arise as a result of limited learning opportunities
4. Knowledge that the client’s conviction regarding the validity of a delusional belief, and their interpretations of events, will often fluctuate over time
L.2 Knowledge of paranoid beliefs
1. Ability to determine the nature and content of paranoid ideation
2. Knowledge of reasoning biases thought to be associated with paranoia (e.g., external attribution bias, interpretation bias, jumping to conclusions)
L.3 Knowledge of beliefs about voices
1. Knowledge of factors that determine the client’s emotional and behavioural reactions to hearing voices (e.g. their beliefs about the voice(s)’ power, identity, malevolence or benevolence, omnipotence or omniscience, the consequences of compliance/non-compliance)
2. Knowledge that clients experience an intimate and inescapable ‘interpersonal’ relationship with their voice(s)
3. Knowledge that malevolent voices are usually associated with negative affect and resisted, and benevolent voices with positive affect, and that voices of all forms may be appeased by “safety-behaviours”
4. Knowledge that individuals may have multiple voices with different characteristics
(e.g. some benign and some malign), for which intervention must be tailored
5. Knowledge that voice hearers are often moderately depressed, and that low mood (along with other affects such as anxiety and shame) can trigger voices
L.4 Assessing the content of delusional beliefs
1. Ability to focus on the beliefs causing the most distress/dysfunction and/or those closely linked to the client’s goals
2. Ability to distinguish the actual content of voices from the client’s beliefs about them
3.
Ability to identify the client’s delusional beliefs regarding compliance with voices
(especially if such behaviour transgresses social rules)
4.
An ability, where there are multiple delusional beliefs, to prioritise the order in which to address them with the client, usually (if appropriate) starting with the
35
least threatening and firmly held
5. Ability to determine the extent to which the content of beliefs are shared by other members of the cultural and faith groups to which the client belongs
6. Ability to help the client to keep a diary/log in order to track when psychotic symptoms occur, and the internal/ external triggers that influence symptoms
7. Ability to help the client use appropriate coping strategies if they become distressed within sessions as a consequence of experiencing voice(s) (e.g. validating efforts to deal with voices, or drawing on prior discussions of triggers)
L.5 Orienting the client to working with the content of delusional beliefs
1. Ability to help the client consider that the extent to which a belief is considered true or false is changeable (e.g. by starting with a previously held belief that the client now views differently or a current belief which they hold with less than
100% conviction)
2. Ability to help the client identify ways in which distress is mediated by their beliefs (rather than a direct relationship between a triggering event and distress)
3. Ability to collaborative ly explore the “pros and cons” of delusions (e.g. while vigilance is a good strategy for avoiding danger it can lead to isolation and loneliness)
4. Ability to openly discuss delusional beliefs held about the therapist, reflecting on the likely feeling or meaning conveyed by delusional content (rather than the content itself)
5. Ability to help the client utilise their own critical evaluation of their belief(s) and reflect on possible anomalies (rather than directly challenging them)
L.6 Working with delusions and beliefs about voices
1. Knowledge that the intervention does not require beliefs to be fully rejected to be effective, and that working to modify part of a belief system can reduce distress
2. Knowledge that cognitive techniques target both the client’s preoccupation with psychotic symptoms and the behaviours associated with experiencing them
3. Knowledge that where discussion seems to result in an adverse impact (e.g. reinforcing rather than diminishing belief strength, or generating upset or anger) discussion should be refocused to more neutral ground
4. Ability to collaboratively reflect on the advantages and disadvantages of holding a delusional belief or experiencing a symptom (and hence reassure the client that the aim is to reduce distress rather than force a change of belief)
36
5. Ability to help client generate alternative explanations for their beliefs
6. Where clients have identifiable and potentially malleable triggers to psychotic symptoms, an ability to help them explore the controllability of symptoms (e.g. by spending more or less time in triggering situations/settings and observing the frequency of symptoms)
7. Ability to link the client’s negative evaluations of self, others and others’ view of self (if accessible) to the psychotic symptom
8. Ability to work collaboratively to help clients understand the ways in which a delusional explanation of their anomalous experiences might have emerged
L7 Working with worry
1. Ability to help reduce levels of worry in patients with persecutory delusions (e.g. using psychoeducation about the role of worry in escalating a sense of threat, reviewing positive and negative beliefs about worry, identifying triggers to worry, using worry periods, planning activity at times of worry and learning to let go of worry)
M. Working with Thought Disorder
1. Knowledge that thought disorder can be conceptualised as a problem of disordered communication between the client and others and that it can increase when emotionally salient topics are discussed
2. Ability to remain open-minded as to whether the client presents with thought disorder or whether the therapist needs to orient to the client’s style of communication, phraseology and concerns
3. Ability to use a non-probing style of questioning and information from the assessment to try to und erstand the client’s concerns and to make suggestions about meaning and content to help structure their communication
4. Ability, when the client sometimes presents with thought disorder, to collaboratively investigate what triggers communication change
5. Ability to address thought disorder and support more effective communication by the client (e.g., by shortening therapist statements to make intent clear, asking clarifying questions, taking breaks throughout the session)
N. Problems in social functioning (negative symptoms)
1. Knowledge that the development and manifestation of negative symptoms can be formulated psychologically (e.g. reflecting hopelessness/depression, or the client’s attempts to avoid anxiety provoking situations)
2. Knowledge of mechanisms that may account for negative symptoms (e.g.
“defeatist” beliefs about the value of pursuing an action, perceiving resources to be limited (e.g., energy, motivation, attention capacity)
37
3. Knowledge that negative symptoms can be formulated as “primary” or as secondary to positive symptoms, and that this informs the form and sequence of intervention
4. Ability to assess negative symptoms (e.g. factors that may account for their presence (e.g. depression, medication side-effects), past and present levels of functioning, relevant cognitive appraisals and beliefs, rate and flow of speech)
5. Where the client finds it difficult to articulate their understanding, an ability to use techniques such as behavioural activation to test-out factors associated with negative symptoms
6. Ability to collaboratively formulate the relationships between negative symptoms and precipitating and maintaining factors, and to discuss areas to target and in what order
7. Ability to address skill deficits that contribute towards the presence of negative symptoms (e.g. building on literacy skills, helping with social skills)
8. Ability to employ strategies that promote motivation and engagement in therapy, (e.g. spending part of the session doing something that the client finds enjoyable, or complementing the client for changes in behaviour, however small)
9. Ability to help the client set meaningful and realistic goals, taking into account current and previous functioning (ensuring that they (and significant others) have appropriate expectations of change)
10.
Ability to establish the role of negative expectancies about performance, pleasure, personal resources or social acceptability, and to conduct cognitive and behavioural work that addresses beliefs interfering with goal achievement
O. Trauma
1. Ability to validate (normalise) the difficulty that clients may have in expressing and exploring difficult traumatic experiences
2. Ability (where appropriate and helpful) to work with the client to develop a narrative of their traumatic experience and relate this to the development of psychosis
3. Ability to establish with the client how they try to manage symptoms of trauma in order to draw links between their traumatic experience and their subsequent reactions
4. Ability to apply standard CBT techniques to help the client manage cognitions associated with experiences characteristic of trauma (e.g. avoidance (both active and passive) re-experiencing, over-arousal and sleep difficulties)
38
5. Ability to help the client achieve their goals even where some trauma symptoms are still present (e.g. by addressing beliefs about being unable to change because of persistent symptoms)
P. Staying or keeping well (relapse prevention)
1. Knowledge that client will display particular early warning signs and idiosyncratic triggers, including changes in mood, behaviour and thoughts
2. Ability to develop a timeline with clients who have recovered to identify problematic events (and their meanings) that have led to previous deteriorations in mental health, and to evaluate any previous relapse prevention strategies
3. Ability to enhance client’s coping strategies by encouraging them to apply skills that foster a sense of control and instil hope
4. Ability to identify and discuss the client’s appraisals regarding the re-emergence of symptoms (e.g. aiming to de-catastrophise reactions to changes in mood, behaviour and thoughts), and to support a sense of the repertoire of strategies they can employ
5. Ability to recognise that for some clients symptoms will persist in spite of intervention, and to understand and discuss recovery and maintenance of gains from this standpoint
39
UNIT 5
FAMILY INTERVENTIONS FOR PEOPLE WITH
PSYCHOSIS AND BIPOLAR DISORDER
The content of this curriculum is based on the competence framework for work with people with psychosis and bipolar disorder (Roth & Pilling (2013), published at: www.ucl.ac.uk/CORE/
The framework contains more detailed information regarding the knowledge and skills outlined in this curriculum, and should be cross-referenced when developing programmes
Introduction
Psychosocial family support and family interventions (FI) are evidence-based interventions which usually (but not invariably) include both the service user/client and their family members. In this context “family” is defined as those people of significance within the service user’s social/support network, not just those with a biological/marital relationship. For some clients, the term “family” might include friends, health, social or care workers, residential services staff, and others with whom they have significant contact.
This curriculum describes a set of principles that are applicable to work with family members with psychosis or bipolar disorder.
Family support and Family interventions
This curriculum contains competences that can be employed by all professionals in order to support families, as well as more specialist skills associated with family interventions
(shaded in grey).
Overview of unit content
At the end of this unit participants would have developed knowledge and skills in the following areas:
C. Knowledge of the rationale for family interventions
D. Knowledge of the core components of a family intervention
E. Ability to engage the family during assessment and formulation
F. Specific components of family interventions
G. Multi-family interventions
Specific learning outcomes from the unit
A. Knowledge of the rationale for family interventions (FI)
10. Knowledge that the aim of FI to empower the family to manage their situation more effectively
40
11. Knowledge of the evidencebase supporting FI’s use as an intervention integrated with wider service provision (e.g. medication, individual psychological and social interventions, care co-ordination)
12. Knowledge of the breadth of issues/circumstances for which FI may be suitable (e.g., helping the partner of a service user with bipolar disorder who becomes sexually disinhibited or parents to differentiate between developmentally normal adolescent behaviour and ‘psychosis’)
13. Knowledge of the ways in which the social/family environment may influence the course of psychosis and bipolar disorder (both positively and negatively)
14. Knowledge of the impact of psychosis and fluctuating mood on family functioning, and hence ability to recognise family member reactions and attitudes as an understandable responses to difficult circumstances
15. Knowledge of the impact of service user and family mental health problems and/or alcohol and drug misuse on daily family functioning, and to address these issues sensitively and directly
16. Knowledge of risk and resilience factors both the family and in the service user
(e.g., family, social and environmental factors)
17. Knowledge of the importance of focussing on improving outcomes for both service users and family members.
18. Ability to identify opportunities and/or barriers presented by the local service context to the routine implementation of FI, and to identify effective solutions or adaptations of the intervention
B. Knowledge of the core components of a family intervention (FI)
1. Knowledge of the usual core components of FI, including:
listening to family members’ experiences
sharing information (psycho-education, including normalisation)
‘staying well’ or relapse prevention strategies
communication and problem-solving skills
helping family members develop empathy and respect for each other’s position
stress management and crisis management techniques
“coping strategy enhancement”
motivational interviewing
signposting to information and peer support services available both locally and nationally
2. Knowledge that the core components of FI are not fixed but are based on an assessment of family needs and on a collaborative formulation
3. Knowledge of the importance of homework or “between session practice” in effecting and reinforcing change
41
4. Knowledge of links between family members’ appraisals and beliefs and their emotional reactions and behavioural responses
C. Ability to engage the family during assessment and formulation
C.1 Ability to engage the family in assessment
1. Ability to identify and overcome barriers to initial contact (for example, by being flexible (e.g. with regard to timing of meetings or whether contact is face-to-face or by phone) or responsive to factors that may dispose families to decline contact (e.g. because they feel blamed, or service users do not want them to be involved))
2. Ability to set up an initial meeting with the family aimed at promoting engagement
(e.g. by explaining the rationale for FI, and describing its key components and potential benefits)
3. Ability to establish trust and respect between family workers and family members
(e.g. by showing empathy for, and respect towards, their experiences)
4. Ability to promote engagement and maintain a working alliance with the family (e.g. by taking a positive non-blaming stance, establishing a connection with every family member, maintaining a consistently collaborative stance, modelling and promoting positive communication)
5. Ability to convey enthusiasm and confidence, and a belief in the value of the approach for the family
6. Ability to work with and manage difficulties in engagement, by employing a variety of strategies, such as:
identifying goals of each family member
focusing on issues that the family see as a priority
acknowledging concerns regarding previous experience of services
discussing evidence and reflection (based on experience) of how FI has helped other families
being flexible about where and when sessions are held
allowing families time to reflect and ask for further clarification
using supervision
7.
Ability to decide whether to co-work with another therapist (e.g. taking into account the FI model employed, the coworker’s skills and experience, any risks posed by individual working and session location)
C.2 Knowledge of confidentiality and consent
1. Knowledge of both the constraints and the permitted actions contained in legal and professional guidance relating to confidentiality and consent
2. Knowledge of, and ability to work with, confidentiality issues that arise in the delivery of FI (e.g. maintaining the right of each family member to confidentiality, managing disclosures of risk)
42
3. Ability to manage issues of confidentiality (e.g. by maintaining an empathic and reflective manner, clarifying reasons for sharing (or not sharing) information, enabling discussion of concerns)
4. Ability to recognise and work with changes in consent from any family member during the process of FI
C.3 Ability to undertake assessment and develop formulation specific to FI
1. Ability to explain the rationale for the assessment process to the family and to ensure that the process is supportive (i.e. non-critical) and not overpowering
2. Ability to conduct a comprehensive assessment that identifies the ways the family communicates and resolves issues, their capacity to act as a ‘problem-solving unit’ and goals at both an individual and family level
3. Ability to conduct an individual assessment with each family member which includes: a. general background information (family demographics and health etc) b. knowledge and key appraisals/beliefs of the service users’ experiences c. family communication skills d. effects of the problems faced by the family and their coping strategies e. daily life pattern f.
personal goals (SMART 1 goals, individualised and achievable within the timeframe of the intervention)
4. Ability to work with the whole family to consider family communication skills, problemsolving skills and patterns of beliefs and behaviour
5. Knowledge of, and ability to employ, structured interview schedules and standardised measures to support clinical assessment
6. Ability to develop a collaborative formulation based on assessment that includes an intervention plan setting out the components to be delivered, in order of priority
D. Specific components of family interventions (FI)
D.1 Therapeutic ground rules and information sharing
1. Ability to collaboratively establish and to document ground rules that identify the basic structure of sessions (e.g. only one person talking at a time, allowing everyone to take a turn)
2. Ability to undertake family psychoeducation, adapting the timing and level of detail to factors such as the course of the individual’s presentation and the family’s capacity to assimilate information
3. Ability to share information in a manner that acknowledges service-users and families as e xperts in their own experience and enables them to share their own “lay model” of the problems they face and discuss beliefs and appraisals that may influence their own and the service users’ recovery
1 * SMART = Specific, Measurable, Attainable, Realistic and Timely
43
4. Ability to tailor information so that it is readily understood by the family (e.g. avoiding jargon, using a variety of media, adapting content to the family’s literacy and language skills)
5.
Ability to be aware of the potential emotional impact of information being shared and to respond appropriately to help families manage this (e.g. not moving on if family members become distressed, showing an understanding of reactions such as anger and denial, allowing time for exploration of sensitive issues
D.2 Early warning signs, relapse prevention and “Staying Well” work
1. Ability to adopt a positive, recovery orientated stance to ‘staying well’ planning (i.e. recognising and promoting wellbeing)
2. Ability to work with the family to identify factors that maintain wellbeing ( e.g. “what I am like/what I am doing wh en I am well?”)
3. Knowledge of the importance of responding appropriately and promptly to early warning signs in reducing the risk of relapse or hospital admission
4. Ability to discuss and promote the rationale for early warning signs work within a family context (i.e. that individuals usually display both common and idiosyncratic signs with a similar pattern or ‘signature’ ahead of relapse) and to discuss the service user and family’s previous experience of relapse
5. Ability to help the family develop techniques to help them identify, monitor and respond to the early signs of relapse (e.g. by developing checklists of common prodromal signs, identifying triggers/“flash points” to relapse identifying and agreeing appropriate responses to signs, documenting decisions about these responses in a way that is meaningful to the family)
6.
Ability to manage difficult emotions that might be triggered by discussions of relapse, and to reinforce the rationale for engaging in the process
7.
Ability to help the family to be mindful of the risk of over-vigilance to warning signs, and to discuss balancing appropriate observance with unhelpful sensitivity
8.
Ability to liaise with any services included in the agreed relapse strategy in order to communicate their expected roles, and to review this at appropriate intervals to take account of any changes in circumstances
D.3 Ability to work with children/ young people of parents with mental health issues
1.
Ability to work with children/young people of parents with mental health issues, for example by:
taking into account their cognitive/developmental stage
discussing their observations of signs of relapse while ensuring that they are not made to feel respo nsible for their parent’s welfare
discussing feelings that may arise if they feel responsible for actions taken to protect their parent
acknowledging the specific issues facing children of lone parents
acknowledging the reasons they may be reluctant to engage
44
recognising that because they may be a young carer they will have individual support needs, and providing appropriate signposts for support
D.4 Enhancing family communication
1. Ability to ensure that the communication skills component of FI is mapped to the formulation (i.e. focuses only on those skills in which the family is least proficient)
2. Ability to use a wide range of materials to demonstrate examples of effective communication (e.g. video, role play, YouTube)
3. Ability to help the family develop positive communication skills (characterised by constructiveness and behavioural specificity), for example by practising active listening, making clear and positive requests of each other, expressing difficult feelings (such as anger or disappointment)
4. Ability to adopt a staged approach to skills development, (e.g. typically beginning with skills with a positive emphasis before moving on to more complex skills or skills with a more challenging focus
5. Ability to elicit from the family, and subsequently summarise/provide, a rationale for the development of each specific skill (e.g. by identifying how the skill might be helpful to them as a family)
6. Ability to help the family practice skills within sessions and to generalise these skills outside of sessions
7. Ability to provide constructive feedback to the family and to ensure that feedback from family members remains constructive
8. Ability to identify “homework” (between session practice) aimed at reinforcing
D.5 Problem solving change, ensuring that this is relevant, clearly understood, and ensuring that this is reviewed in subsequent sessions
1. Ability to elicit from the family, and subsequently summarise/provide a rationale for structured problem solving (e.g. building on their existing strengths to improve family functioning/ reduce family stress, encourage family participation and help achieve individual and family goals)
2. Ability to help the family develop and use problem-solving and crisis management skills (e.g. by helping them to see the problem-solving approach as relevant and applicable, or by modelling each element of the model to help manage in crisis situations)
3. Ability to introduce a structured problem-solving model and clearly define each component that includes:
agreeing a clear, specific definition of the problem/goal
listing all possible solutions
evaluating the advantages and disadvantages of each
negotiating the “best” solution and planning implementation
45
reviewing the results
4. Ability to ensure that solutions usually involve all members of the family making changes, and (as far as is possible and practical) employing strategies that enable all family members to have a voice in the process
5. Ability to adopt a staged approach to problem solving, starting with circumscribed, behaviourally-specific problems through to more complex or emotionally challenging issues
6. Ability to promote proficiency and independence in problem solving by shifting from active involvement, modelling and demonstration towards encouraging its use outside sessions
D.6 Managing a planned disengagement
1. Ability (throughout the intervention) to help the family act independently (e.g. by taking the role of “coach” rather than “team captain, eliciting rationales for skill development and not directly doing anything that the family are capable of doing themselves)
2. Ability to work actively towards disengagement (e.g. by signalling from an early stage that the intervention is circumscribed and time-limited, ensuring that homework is being carried out (so as to support generalisation of skills))
3. Ability to review progress frequently and to adapt the intervention accordingly, and discuss progress with the family so that disengagement is seen as positive and to be expected
4. Ability to help the family to acknowledge progress and skill development
5. Ability to discuss the possibility of “top-up” sessions and ongoing support with the family where appropriate
D.7 Evaluation
1. Ability to write a collaborative report of the intervention (e.g. where this helps to summarise key points of learning, or to give feedback to others involved in care of the service user)
2. Ability to explain the rationale for evaluation and engage the family in completing an appropriate range of outcome measures
3. Ability to interpret and apply measures/data (e.g. in relation to service evaluation, or as a way of indicating areas for professional skills development
D.8 Supervision
1. Ability to engage in clinical supervision with appropriately trained supervisors (e.g., familiar with FI or through peer supervision)
46
E. Multi-family interventions
This section of the curriculum primarily relates to multi-family groups where a number of families and service users are seen together. However, it also relates to groups for family members (held in the absence of the service user) which run in parallel with single-family interventions, and groups that include service users and peer supporters as co-facilitators..
1. Ability to manage the practicalities of group working (e.g. agreeing roles with a cotherapist, identifying an optimal group size in relation to whether the group is interactive or more didactic, planning for dropout over time)
2. Ability to select appropriate participants if the group has a particular focus (e.g. on early intervention, or is intended for BME clients and their families)
3. Ability to decide whether the group will be open to new participants over time, or will be “closed” (based on knowledge of the advantages/disadvantages to each)
4. Ability to maintain engagement and attendance (e.g., by addressing the issue explicitly, identifying and addressing potential barriers to attendance with individuals, using reminder strategies)
5.
Ability to promote a safe ‘social’ environment by establishing clear agenda and objectives and maintaining ground rules (e.g. regarding communication, confidentiality and attendance during crises or elevated mood, setting limits on expectations of ‘performance’ within the group)
6.
Anility to balance intra- and inter-family boundaries and to provide the opportunity for families to test out more adaptive, empathic relational styles with other families before trying it in their own
7. Ability to apply both individual and family therapy techniques in a flexible and responsive manner in order to establish a social structure for the group (e.g. focusing on specific individuals or on one family, inhibiting unhelpful interactions, intervening when ground rules are broken)
8.
Ability to encourage and validate families’ contributions to the group and to each other by using group therapy skills (e.g. identifying group processes, validating themes through normalisation, inviting responses from individuals or subgroups, using praise and positive reinforcement)
9.
Ability (in more mature groups) to promote relationships across family boundaries
(e.g. by working with social bonds that have developed, positively reinforcing families’ ability to support one another, expanding conversation to include others)
10.
Ability to appropriately evaluate the group/intervention
47
UNIT 5
COGNITIVE BEHAVIOURAL THERAPY (CBT) FOR BIPOLAR DISORDER
The content of this curriculum is based on the competence framework for work with people with psychosis and bipolar disorder (Roth & Pilling (2013), published at: www.ucl.ac.uk/CORE/
The framework contains more detailed information regarding the knowledge and skills outlined in this curriculum, and should be cross-referenced when developing programmes
Introduction
This unit outlines the knowledge and skills required to carry out CBT for people with bipolar disorder (BD).
Effective delivery of CBT for bipolar disorder rests on knowledge of (and experience in applying) the techniques of cognitive behaviour therapy. This is because CBT for BD requires practitioners to be fluent in these skills. Further, CBT for BD often focuses on common coexisting presentations (such mood disorders, anxiety, worry or sleep, dysregulation, substance use and suicidality). As such the learning outcomes described below build on (and assume) the knowledge and skills set out in the CBT competence framework (accessed www.ucl.ac.uk/CORE/).
General learning outcomes
At the end of this unit participants will be able to demonstrate knowledge and skills relating to the following areas:
O. Knowledge of assumptions and structure of a CBT intervention for BD
P. Engagement in CBT for BD
Q. Assessment in CBT for BD
R. Formulation
S. Cognitive interventions
T. Behavioural interventions focused on enhancing self-regulation
U. Stigma, guilt and loss
V. Managing impact on close relationships
W. Early warning signs and coping
X. Relapse prevention
Y. Ending therapy
48
Specific learning outcomes
A. Knowledge of basic assumptions and structure of a CBT intervention for BD
1. Knowledge of vulnerability stress models of BD, including factors such as: a. circadian rhythm instabilities (including sleep/wake cycle or activity levels) b. unhelpful appraisals of success or failure (e.g. unrealistic appraisals of achievement, or underestimating achievement and gaining little sense of pleasure or reward) c. very reactive responses to success or failure (e.g. success leading to a marked elevation of mood and driven behaviour, failure leading to dysphoria or depression)
2. Knowledge that CBT aims to help individuals develop coping strategies that allow them to benefit from their appraisal styles and drive but also reduce their vulnerability
3. Knowledge of the usual components in a CBT interventions for BD e.g.: a. discussing evidence-based information about BD (including vulnerabilitystress models and their implications for psychological intervention) b. developing skills to enhance coping with prodromes of mood episodes c. maintaining regular routines and identifying the ways in which these can be regulated d. managing potential vulnerabilities (e.g. impulsivity, or interpersonal disputes)
B. Engagement
B.1 Ability to engage in a collaborative and flexible manner
1. Ability to use and maintain a collaborative, recovery oriented stance that consistently focuses on the client’s goals, motivations and strengths
2. Ability to engage family members or other carers in therapy sessions and provide family members/carers with assessment information (where relevant and as agreed with the client)
3. Ability to amend session length flexibly (e.g.in relation to client mood, activity level and capacity to focus on therapeutic work)
4. Ability to recognise if and when a client’s pattern of alliance and motivation is fluctuating in tandem with their mood state and to adapt session focus/duration accordingly
5. Ability to respond to variations in the client ’s capacity to engage, and knowledge of factors that may influence this (e.g. complexity of presentation, level/pattern of disability, significant instability in mood)
B2. Ability to engage the client in discussion of Bipolar Disorder
1. Ability to take a normalising approach to symptom onset (e.g. introducing the idea of BD as an understandable reaction to abnormal stressors/life events)
49
2. Ability to engage the client in discussion of BD (e.g., factors thought to contribute to its development and maintenance, influence of common coexisting presentations
(e.g. anxiety or substance misuse)
3. Ability to provide psychoeducational information in a non-didactic, discursive and collegial manner that explicitly fosters challenge/debate and encourages information-seeking
4. Ability to discuss patterns of medication use in an open, collaborative and nonjudgemental way (e.g. considering the relative merits and costs of medication/adherence for the individual client)
5. Ability to normalise experience of mood fluctuations and instil hope that mood management is possible (e.g. by discussing the continuum model of mood fluctuations and potential psychosocial coping strategies)
6. Ability to hold in mind that for some clients their primary goals relate to functional/personal recovery outcomes rather than mood management
B.4 Ability to deal with emotional content of a session
1. Ability respond to the expression of strong affect by maintaining a flexible approach, adapting session content, duration and timing appropriately
2. Ability to manage interactions if emerging mania threatens to create ruptures in the therapeutic relationship (e.g., by “stepping back” from a confrontation)
3. Ability to acknowledge and help the client manage mood states or activity level changes that are:
too high (e.g. euphoria, overactivity or irritability), for example by using collaborative problem solving approaches
too low (e.g. apathy, low motivation) for example by working collaboratively to implement activation strategies
4. Ability to engage with emotional issues that may present a challenge to goal achievement (e.g. high levels of hostility, anxiety, anger or avoidance of strong affect) through appropriate application of CBT techniques
5. Ability to collaboratively help the client access, differentiate and experience their emotions in a way that both facilitates change and is congruent with their goals
C. Assessment
C.1 Knowledge of the scope and collaborative nature of assessment
1. Ability to work collaboratively with the client and to: a. elicit a detailed history of mood experiences and their association with life events (including trauma) b. develop a detailed timeline of milestones, achievements and life events in relation to the development and experience of BD and to specific bipolar episodes c. elicit the client’s understanding of any family history of mood problems and how this informs beliefs about their own mood experiences
50
d. discuss the impact of BD on the client’s life and life goals, and their sense of positive and negative aspects of the disorder
2. Ability to relate the experience of BD to the client’s wider societal values and goals
3. Ability to discuss the personal relevance/ significance and meaning of a diagnosis of
BD with the client
4. Ability to discuss the client’s pathway to diagnosis (including previous diagnoses and any concerns about the accuracy of their current diagnosis)
5. Ability to explore the client’s sense of the relevance of a psychological therapy
6. Ability to identify, common co-existing problems in BD (particularly anxiety and substance misuse)
7. Ability to discuss issues related to medication with the client (including side effects, relationship to medication and “messages” regarding medication received from other professionals
8. Ability to identify aspects of BD that clients value (such as hypomania) and any ambivalence about intervention (based on concerns that this will limit access to aspects of BD that they experience positively)
9. Ability to explore the psychological impacts of past episodes/behaviour (e.g., impact of extreme behaviours, interpersonal and socio-occupational disruption and impact on sense of self-worth)
10. Ability to discuss the impact of stigma and self-stigmatisation
11. Ability to identify the social network and support available to the client (including informal, family and professional support)
12. Ability to identify and discuss issues relating to pregnancy and parenthood (e.g., relationship between medication and pregnancy, concerns about intergenerational transmission)
C.2 Ability to assess resilience and risk factors and the client’s current mood state
1. Ability to identify and discuss periods when the client has coped well in life (including with problematic mood swings) and how this was achieved
2. Ability to identify protective factors in the client’s social network
3. Ability to identify the client’s characteristic responses to mood change (e.g., rumination or risk-taking, adaptive approaches) and to identify and explore risk in relation to depressed mood (e.g., suicide/self-harm) and elevated mood (e.g., impulsivity/disinhibition and risk taking)
4. Ability to detect personalit y styles which may influence the client’s responses to therapy tasks and goal-setting (e.g, perfectionism, need for autonomy, impulsivity)
5. Ability to assess the client’s pattern of shifts between different mood states, and how these states are manifested (e.g. using observational measures, self-report and third-
51
party information (including clinical information and information from family and friends))
6.
Ability to reach a co llaborative understanding of the client’s mood experiences and their impact on other aspects of their life
C.2 Ability to use measures and self-monitoring to guide therapy and monitor outcome
1. Ability to select and employ validated measures relevant to the client’s presentation
(e.g., assessing mood and symptoms, specific BD features, personal recovery, appraisal style, social functioning or quality of life)
2. Ability to help the client self-monitor and (over the course of the intervention) to build on this skill as part of self-management
D.3 Ability to discuss the CBT model
1. Ability to discuss the CBT model with the client (e.g. that clinical episodes derive from interactions between proximal factors (such as stressors), distal factors (such as experiences of loss), the client’s explanatory styles, and circadian vulnerability) and to help the client consider the role of these interactions in their own experience
2. Knowledge that acceptance of BD as a diagnosis is not required for the client to engage with CBT
3. Ability to work with the client to identify whether CBT is not appropriate for their needs (e.g., where the client has a purely biological view, is currently in an acute manic episode or does not identify issues to work on psychologically)
E. Formulation
E.1 Ability to construct a formulation
1. Ability to develop a collaborative formulation that is personally meaningful to the client and presented in a way that is comprehensible, normalising and instilling of hope
2. Ability to construct a formulation that recognises that some ‘problem behaviours’ may also be associated with real achievements, and that changing them may be associated with understandable ambivalence
3. Ability to develop a formulation that: a. reflects the client’s success in dealing with presenting problems as well as any difficulties b. formulates how each problem is maintained c. makes a link between the formulation and the personal goals identified by the client
E.2 Ability to identify goals for the intervention
1. Ability to work with the client to set goals that they personally value and that incorporate concepts of recovery consistent with the collaborative formulation
52
2. Ability to regularly review goals with the client to reflect shifting priorities as therapy progresses
3. Ability to include goals that relate to: a) symptom reduction b) medication use/adherence c) valued activities d) self-management of cognitive, behavioural and/or emotional instability e) appropriate and planned use of services to optimise self-management f) concepts of recovery and well-being
4. Ability to work with the client to strike a balance between immediate and longer-term goals
5. Ability to identify and operationalise achievable steps towards agreed goals and collaboratively identify and problem-solve impediments to goal achievement
F. Cognitive interventions
1. Ability to engage the client in self-monitoring of mood, activity patterns, thoughts and belief patterns and medication use
F.1 Monitoring links between variations in mood and patterns of daily activity levels
1. Knowledge that mood monitoring can be an effective way to help clients understand their mood experiences (by identifying their own pattern of normal and abnormal mood variation) and consequently can aid self-management
2. Ability to help the client use mood and activity diaries to rate their mood, and to identify personalised anchor points for their ratings (so as to individualise scales)
3. Ability to use the mood diary to help the client discriminate normal mood states from those requiring attention (e.g. by reflecting on patterns of mood and behaviour and identifying patterns that may contribute to mood dysregulation)
4. Ability to help the client understand that many mood fluctuations are normal
(especially in the absence of abnormal sleep or activation levels) and do not necessarily signify the onset of a manic or depressive episode
5. Ability to help the client explore whether they are unhelpfully restricting activities due to fluctuations in mood and worry about relapse
6. Ability to help the client work towards as much or as little mood fluctuation as they wish, bearing in mind that costs and benefits of fluctuations differ for each client
7.
Ability to address any increases in client anxiety due to mood monitoring (e.g. using mood records to illustrate the self-correcting nature of the majority of mood fluctuations)
53
F.2 Identifying cognitive changes associated with different mood states
1. Knowledge of cognitions commonly associated with extreme mood states (e.g., over optimistic predictions of success and reduced risk awareness when manic, selfblame and hopelessness when low)
2. Knowledge that positive and negative automatic thoughts occurring in the context of elevated and/or depressed mood can be inaccurate and biased, and so significantly influence the client’s feelings and actions and subsequent mood changes
3. Knowledge that potentially problematic appraisal and thought patterns often persist at lower levels of intensity outside of mood episodes
4. Ability to work with the client to identify the specific changes in cognition associated with high or low mood states (e.g., by eliciting global thoughts and images, using structured questioning to refine global thoughts into specific thoughts or using thought and thought challenge records)
5. Ability to use Socratic questioning to help the client consider evidence that supports or challenges problematic thoughts, based on review of thought records and other relevant information (e.g., diary records)
6. Ability to help the client consider alternative explanations and perspectives on their thoughts (e.g. through in-session reflection, by generating alternatives, and through homework tasks)
7. Ability to help client gain external feedback on their problematic thoughts (e.g. th rough “polling exercises” with trusted others, or through anonymous surveys supported by the therapist)
8. Ability to help the client identify particularly positive automatic thoughts (e.g., by reflection on recent hypomanic episodes), to identify those that are problematic , and to assess their belief in these thoughts when in and out of a mood episode
9. Ability to work with the client to challenge problematic positive automatic thoughts
(e.g., starting with beliefs that are not strongly held when euthymic, progressing to beliefs that are strongly held when hypomanic or depressed and which may increase
10. Ability to help the client to detect suicidal thoughts and to help identify alternatives to suicidality using problem-solving approaches the risk of future mood episodes)
F.3 Ability to identify key cognitive factors and attributional styles
1. Ability to identify cognitive vulnerability factors and specific areas of vulnerability associated with BD in order to inform treatment goals (e.g. perfectionism, problemsolving deficits, decision-making biases (e.g. a bias to engage in high risk and impulsive decision making))
54
F.4 Ability to identify positive and negative self-appraisals of internal states
1. Knowledge that a tendency to explain changes in mood with reference to internal (as opposed to external) factors is associated with a higher risk of mania and depression
2. Ability to explore the extent to which the client explains changes in mood and behaviour as being driven by internal (self/personality) versus external (day to day events and relationships) factors
3. Ability to help the client recognise and evaluate the self-appraisal of their internal states and to identify positive and negative bias and problematic appraisals
4. Ability to help the client repeatedly identify and strengthen their awareness of connections between external events and mood state/activation levels changes, as an alternative to internal self-appraisal
5. Ability to help the client learn to modify cognitive biases occurring during extreme mood states and to attribute these to external events
F.5 Ability to identify and modify assumptions and beliefs driving impaired functioning and relapse
1. Ability to work with the client to identify assumptions, attitudes and rules that drive impaired functioning and relapse, ensuring this process is client-led
2. Ability to use the ‘downward arrow’ technique to help the client identify and elaborate possible assumptions and their meaning, and to identify those assumptions that are central, and those which are more peripheral
3. Ability to challenge assumptions (while taking care not to make these challenges didactically)
4.
Ability to help the client to consider how assumptions can become self-fulfilling and to consider changing /discarding self-defeating assumptions by identifying the advantages and disadvantages of retaining them
5.
Ability to help the client act against their assumptions (e.g. through behavioural experiments)
6.
Ability to help clients examine the long-term (rather than short-term) effectiveness of their assumptions
7.
Ability to begin developing hypotheses about likely core beliefs and to tentatively present these to the client
8.
Ability to help the client reconstrue core beliefs as ideas whose validity can be tested and to use standard cognitive techniques to help them modify existing and strengthen new beliefs
F.6 Ability to employ cognitive and behavioural strategies for hypomania/ mania
1.
Ability to help clients evaluate and reframe unrealistically positive ideas using
“reframing” to consider an alternative view grounded in available evidence
55
2.
Ability to help the client to identify unrealistically positive ideas associated with recent experiences of mania/hypomamia, to explore links between these ideas and mood elevation, and to reframe them as possible indicators of an impending mood episode
3.
Ability to help the client consider how best to respond to thoughts which they themselves agree are early warning signs
4. Ability to introduce daily thought records identifying hyperpositive thinking
5. Ability to help the client appraise mania-related behaviours and elevated risk taking using “risk ratings” of their productive or destructive consequences
6. Ability to challenge overvalued ideas (e.g. through role playing, foreseeing negative consequences through imagery, and anticipatory problem solving)
7.
Ability to target scattered and unfocused thinking associated with manic mood states (e.g. through intensive structuring of session, or modelling of measured speech and response patterns)
8. Ability to help clients manage unrealistically positive ideas by discussing strategies for delaying acting on them (e.g. by not acting for an agreed period of time and using cognitive strategies to evaluate ideas during the delay period)
F.7 Appraising positive and negative aspects of hypomania
1. Knowledge that (because of their enjoyment of hypomanic states, or because they see these as part of their personality) some clients may be reluctant to take actions to prevent hypomania or curtail elevated mood
2.
Ability to explore with clients all aspects of their hypomania and agree how, when and if signs of an elevated mood may be managed
3.
Ability to help the client weigh up the positive and negative consequences of hypomania using a costs/benefit analysis
G. Behavioural interventions focused on enhancing self-regulation
G.1 Ability to understand the relationship between mood and activity
1. Knowledge that because the circadian rhythms of people with BD may be particularly sensitive to disruption, risk of relapse may be reduced through maintenance of regular routines and sleep patterns (while also being aware of the risks of an overly restrictive approach)
2. Knowledge that self-regulation of mood and activity levels is essential for coping with BD
56
G.2 Activity monitoring and scheduling
1. Ability to help clients monitor their activities by completing an activity chart and rating degrees of pleasure and mastery associated with activities
2. Ability to review activity charts with the client to identify activities that are over- or under-represented, and those associated with high or low levels of pleasure and mastery
3. Ability to work with the client to identify and plan specific changes to activities, identifying any thoughts which might make it difficult to implement these changes
G.3 Regulating activity levels
1. Ability to help the client understand the potential mood-stabilising benefits of balancing constructive, task-focused activity with pleasurable non-task activity/recreation (e.g. by using mood and activity charts to assess the current balance of activities, collaboratively evaluating this balance and discussing the introduction of new activities)
2. Ability to use the activity chart to help clients schedule activities and agree specific targets (e.g. to help regulate the timing and duration of sleep and frequency of meals, or the balance of social contact and time spent alone) identifying and problem solving potential barriers to achieving these aims
3. Ability to help clients record predicted and actual levels of pleasure and mastery associated with scheduled activities, and to reflect on the implications of any disparities (especially where these arise when the client is depressed)
4. Ability to discuss automatic thoughts or beliefs that emerge prior to, or during activities (in particular, comparing their predictions of the outcome of an activity with actual outcomes to help amend unhelpfully positive or negative thoughts)
G.4 Applied relaxation, breathing and mindfulness exercises
1. Knowledge that various forms of relaxation training may be helpful for clients who find it hard to ‘wind down’ or switch off during escalating mood and reducing anxiety associated with extreme mood fluctuations
2. Ability to explain the rationale for, and application of, applied relaxation to the client
3. Ability to teach clients progressive relaxation techniques and help them to apply and maintain these in anxiety-provoking situations
4. Ability to describe and explain the rationale for mindfulness exercises, and to teach these to clients (e.g., mindful walking/eating, taking an observer role in relation to thoughts, using breathing exercises to help experience thoughts/feelings without reacting to them)
G.5 Managing over-activity
1. An ability to resist the impulse to overactivity at the early stages of a manic episode and to identify strategies that can assist them in achieving this
57
G6 Stimulus control
1. Knowledge that significant mood shifts can be triggered by specific stimuli/events (e.g., changes to routine, work stress, alcohol/excessive caffeine or illegal drug use)
2. Ability to help the client to develop awareness of stimuli/ events which trigger a distinctive mood shift (e.g., using guided discovery) and develop and identify pre-defined strategies that can be used to moderate their impact
3.
Ability to work with the client to agree targets for exposure to, and avoidance of, trigger stimuli, and to problem solve issues that might make behavioural change challenging
4.
Ability to work with the client to identify whether the experience of challenging or exciting activities is personally important, and if so to plan activities that balance excitement against risk of triggering a mood episode
G.7 Life chart mapping
1. Knowledge of the use of life charts to help clients gain insight into the relationships between cognitive/behavioural responses to events and to their mood experiences
2. Ability to alert the client to the fact that constructing a life chart can be emotionally challenging, and so help them make an informed decision about proceeding
3. Ability to work with the client to decide which episodes to include and at what level of detail
4. Ability to work with the client to consider whether episodes of mood instability were precipitated by identifiable events and use the life chart to identify potential patterns of vulnerability to specific types of stress
G.8 Sleep routines
1. Ability to work with the client to identify patterns of sleep disturbances associated with changes in mood and to develop a sleep routine (e.g. identifying sleep restriction targets for excessive sleep, or extension targets where sleep is too brief)
2. Ability (when mood changes make it difficult for the client to adopt behavioural sleep techniques) to discuss the use of adjunctive time-limited sleep medication
H. Stigma, guilt and loss
1. Ability to work with the client to identify their experience of stigma and to consider its impact (e.g., on their capacity to meet therapy goals)
2.
Ability to work with the client to identify self-stigmatising thoughts and beliefs and to employ CBT techniques (such as behavioural experiment) to address these
3.
Ability to reduce self-stigma by revisiting the vulnerability stress model with the client
(e.g. drawing attention to their capacity to exercise control in relation to mood experiences)
58
4.
Ability to detect and moderate excessive guilt associated with behaviours engaged in during manic episodes (e,g, by exploring their impact on the client and others, identifying their own responsibilities and that of others)
5.
Ability to explore the client’s experience of losses directly associated with BD
(e.g., family and social relationships, lack/loss of employment or higher status employment)
6.
Ability to employ problem-solving techniques where losses can be mitigated
7.
Ability to use emotional processing approaches where losses cannot be mitigated
8.
Ability to assess and manage high levels of hopelessness and suicidality by contracting for safety, identifying and challenging of suicidogenic beliefs, maximising social support and formulating crisis plans
I. Managing the impact of BD on close relationships
1. Ability to identify anger and irritability arising in the context of mood episodes and address their effect on existing relationships and coping resources (e.g. identifying triggers and identifying alternative responses and management strategies)
2. Ability to identify sources of support for family members where their distress is impacting negatively on client outcomes
3. Ability to identify and work with family communication patterns that impact adversely on coping with mood states (e.g. by enhancing communication skills and empathic problem solving)
I.1 Couples therapy
1. Ability to offer couple sessions, where this is likely to enhance therapeutic outcomes
(e.g. where knowing more about BD would help partners understand the client’s behaviour, where the carer could help the client identify early warning signs, or where focusing on communication skills may be especially important (e.g., in the early phases of mania))
I.2 Child care issues
1. Where relevant, an ability to discuss child care issues with the client (e.g: identifying possible risks associated with depressive or manic mood states, and agreeing action plans to address these, or where contact with children is limited, considering constructive approaches to optimise relationships)
J. Early warning signs and coping
J.1 Identifying early warning signs and ways of coping
1. Ability to introduce a focus on early warning signs for mania, depression and mixed episodes as soon as sufficient information is available to inform early warning signs and coping lists
59
2. Ability to discuss with the client the rationale for detecting and coping with prodromal signs (i.e. its relevance in self-management)
3.
Ability to ensure that clients do not become overly anxious about, or sensitive to, mood changes (e.g. by highlighting the importance of choice in moving towards or away from an episode)
4.
Ability to help the client reflect on past experiences to identify changes in thoughts, behaviour or mood associated with moving into a manic or depressive phase
5.
Ability to work with the client to produce a list of prodromes for mania and depression that is specific enough for them to identify when they occur
6.
Ability to identify behavioural and cognitive coping strategies that may help to manage prodromes (e.g., thought challenging, increase/reduction in activity, increasing support from family/friends or input from clinical care team)
7.
Ability to develop an agreed early warning signs plan for mania, depression and
(where appropriate) mixed episodes which summarises prodromes and coping strategies
8.
Ability to work with the client to construct a personal mania profile that identifies personal triggers, coping responses and ways in which appraisals of responses to mania vary in relation to mood state (e.g. using a cost benefit analysis)
9.
Ability to work with the client to construct a personal depression profile that identifies personal triggers, coping responses and ways in which appraisals of responses to depression vary in relation to mood state (e.g. using a cost benefit analysis)
J.2 Staying Well plans
1. Ability to agree with the client a ‘staying well’ plan based on key elements and strategies that have emerged from therapy
2. Ability to identify and incorporate any relevant changes that the client plans to make after therapy
3. Ability to work with the client to ensure the plan is written in their own words, has an appropriately constructive tone, and identifies key elements they wish to maintain after therapy
K Relapse prevention
1. Ability to discuss with the client how they might use the staying well and coping plans to troubleshoot potential challenges after therapy has ended
2. Ability to consider with the client whether a small number booster sessions may optimise clinical outcomes over the longer term
60
L Ending therapy
1. Ability to collaboratively work towards a planned ending in therapy, based on completion of work on shared therapy goals
2. Ability to summarise the progress made in therapy
3. Ability to collaboratively decide whether to share staying well and coping plans with family members/clinical professionals, and where this is agreed, to negotiate how and with whom to share this information
61
UNIT 5
PSYCHOEDUCATION FOR BIPOLAR DISORDER
The content of this curriculum is based on the competence framework for work with people with psychosis and bipolar disorder (Roth & Pilling (2013), published at: www.ucl.ac.uk/CORE/
The framework contains more detailed information regarding the knowledge and skills outlined in this curriculum, and should be cross-referenced when developing programmes
Introduction
This unit outlines the knowledge and skills required to carry out group psychoeducation for people with Bipolar Disorder.
General learning outcomes
At the end of this unit participants will be able to demonstrate knowledge and skills relating to the following areas:
A. Knowledge of psychoeducation and an ability to set up a psychoeducational group
B. Ability to deliver a systematic programme of psychoeducation
Specific learning outcomes
H. Knowledge of psychoeducation and ability to set up a psychoeducational group
A.1 Knowledge of psychoeducation for Bipolar Disorder
1. Knowledge that psychoeducation should adopt a psycho-bio-social model to address all aspects of the client’s treatment interventions, deliver ‘user-friendly’ specific information about bipolar disorder and its management, and teach and encourage practice of effective coping skills
2. Knowledge of the usual aims of psychoeducation (e.g. to increase awareness of bipolar disorder, help clients reconsider related attitudes and behaviours and detect warning signs of new episodes, encourage treatment adherence)
3. Knowledge of evidence of the efficacy of psychoeducation delivered in a group format, and the contribution to efficacy of opportunities for modelling and mutual support
62
4. Knowledge that psychoeducation should be introduced when clients are s euthymic
5. Knowledge that dropout in the first few sessions is predictable and should be taken into account to ensure group size remains viable
6. Knowledge of the advantages of co-facilitation of groups by at least two therapists experienced in running groups and working with people with bipolar disorder
7. Ability to adapt session content so that it maps to group members’ experiences and needs
I. Delivering a systematic programme of psychoeducation
B.1 Establishing the group
5. Ability to explain the rationale for the group and outline content, explain the group schedule and establish ground rules (e.g. confidentiality, expectations around attendance and practice assignments, etc.)
B.2 Increasing awareness of bipolar disorder
1. Ability to convey comprehensive information about bipolar disorder in an open and collaborative manner that encourages dialogue (e.g. to establish client’s pre-existing client knowledge and stance)
2. Ability to help clients learn about the evolution of bipolar disorder evolution and its prognosis (e.g. helping clients draw a personal chart illustrating episodes, triggers, consequences and treatments)
3. Ability to ensure that, over time, all members of the group can present and discuss their life charts
B.3 Improving adherence
1. Ability to discuss factors that commonly influence treatment adherence
2. Ability to discuss medication commonly prescribed for people with bipolar disorder and the factors that may influence medication adherence
3. Ability to discuss risks associated with unplanned withdrawal from medication
B.4 Substance abuse
1. Ability to discuss the potential dysregulating impact of substance use and abuse and engage the group in open discussion of the impacts of legal and illicit substances and stimulants
2. Ability to maintain a focus on a medical, rather than a moral, rationale for controlling substance use
63
B.5 Detection of new episodes
1. Ability to present common indicators of relapse and use group discussion to help clients identify and act on indicators for hypomania, mania and depression
2. Ability to help clients nominate a trusted individual to work with outside the group to help identify reliable early warning signs of relapse
3. Ability to help clients identify changes preceding the onset of warning signs (e.g., changes in symptoms and perceptual experience)
4. Ability to help clients develop an individualised list of specific early indicators and develop an action plan for responding to these indicators (e.g. contacting clinicians, adjusting medication dose, adjusting social regulators)
B.6 Regulation and stress management
1. Ability to discuss the importance of maintaining a regular schedule (e.g. of activity, social contact sleep) and help clients consider how to achieve a schedule that balances their needs/interests with the need for stability
2. Ability to help clients discuss their reactions to stress and consider strategies for managing more effectively (e.g., using relaxation or problem-solving)
B.7 Ending the group
1. Ability to review content covered in the group and help clients review their experience of the group
64
UNIT 6
METACOMPETENCES
The content of this curriculum is based on the competence framework for work with people with psychosis and bipolar disorder (Roth & Pilling (2013), published at: www.ucl.ac.uk/CORE/
The framework contains more detailed information regarding the knowledge and skills outlined in this curriculum, and should be cross-referenced when developing programmes
Introduction
There is a clear professional consensus that the effectiveness of work with people with psychosis and bipolar disorder is strongly influenced by the ability to use clinical judgment in order to balance the maintenance of a task-focused approach with the ability to be flexible and focused on the needs, wishes, aspirations and capacities of individual clients and their families/carers. The competences in this section are not abstract ideas, but form an underpinning to the way in which interventions are delivered. As such the content needs to be embodied in (and exemplified within) teaching of more concrete clinical skills described in other units of this curriculum (an observation that also applies to the unit setting out therapist stance, values and style).
General learning outcomes from the unit
At the end of this unit participants will be able to demonstrate knowledge and skills relating to the application of clinical judgment in the delivery of interventions with people with psychosis or bipolar disorder.
Specific learning outcomes from the unit
In what follows the term ‘client’ is used to denote both individuals, families and carers
Therapist stance and style
1. Ability to vary style in relation to session content or type of intervention (e.g. balancing an empathic with a directive style, as appropriate)
2. An ability to practice in a manner that is congruent with the current evidence base, and to use clinical judgment to decide when and how to integrate emerging evidence with current practice, and whether, when and how to work beyond the evidence base
Engagement
1. Ability to balance the instillation of hope that change is possible and that interventions will be helpful against the need to convey a sense of realism regarding the likely challenges of therapy
65
2. Ability to judge whether and how to persevere when engagement is threatened by factors characteristic of psychosis or bipolar disorder (e.g. struggling to maintain a conversational thread, confusional states or rapidly changeable states reflecting a worsening of symptoms)
Assessment
1. Ability to balance the benefits of a thorough assessment against the benefits of initiating interventions (e.g. judging when assessment has been optimal and sufficient, even if incomplete in some areas, or where more assessment information is required before an intervention can be carried out safely)
2. Ability to adopt a flexible and responsive approach to assessment that balances the need to obtain information against the client’s readiness and willingness to share this with the therapist
Case conceptualisation and formulation
1. Ability to judge the level of complexity and detail required of a formulation, holding in mind the intervention being planned
2. When constructing a formulation and planning treatment, an ability to reflect the interplay of biological, psychological and social factors in the development and maintenance of clients’ difficulties
3. Ability to draw on a formulation to identify the most appropriate focus and sequence of interventions most likely achieve change, and to ensure that this sequence is congruent with th e client’s perceptions of what would be most useful to them
4. Ability to hold in mind both the client’s perspectives on events as well as those of the professionals with whom they are contact, identifying how best to manage any differences of viewpoint and their potential impact on the therapeutic relationship
Validation
1. Ability to achieve a balance between explicitly validating the client’s experience and distress while helping them to consider the possibility of alternative perspectives
Implementing interventions
2. Ability to maintain a task-focused approach while being sensitive to (and being directed by) the client’s needs and capacities and maintaining a consistent sense of collaboration with the client
3. Ability to use clinical judgment to manage and respond to rapid changes in thinking, perception and presentation that are characteristic of psychosis or bipolar disorder in order to maintain the alliance and the ‘thread’ of therapy
Information sharing
1. Ability to judge what and how much information should be shared and with whom in the light of the specific situation of the client, the stage of their illness, and the interests of each party and the protection of the public
Working with coexisting disorders
1. Ability to use clinical judgment in order to adapt and titrate standard interventions for common co-existing disorders and integrate them into the treatment
66
Supervision
1. Ability to manage and tolerate personal feelings elicited by challenging behaviours
(such as hostility, suspiciousness, amotivation) and to recognise when support or supervision is necessary in order to continue working effectively
67