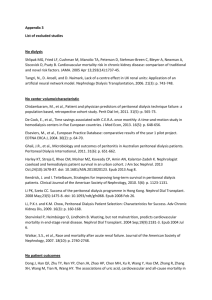
NOTES
advertisement

NOTES Chronic Renal Failure cmj Module #13: Nursing Care of the Individual with Genitourinary Disorders: Chronic Renal Failure Chronic Renal Failure & ESRD (click here) & Transplant (see Online tutorial in Module) A. Etiology/Pathophysiology (general) 1. 2. Normal physiology-( ref to ARF-A & P) Progressive renal tissue destruction and loss of function a. Progresses over years without being recognized until kidneys unable to excrete metabolic wastes and electrolytes: End-stage Renal Disease (ESRD) b. Incidence increasing- especially in older adults; higher in African Americans , Native Americans; large Hispanic population requires dialysis here in local area; 300,000 patients with ESRD, incidence increased almost 8% per year for past 5 years c. Chronic renal failure- diffuse bilateral disease of kidneys with progressive destruction and scarring; loss of function precedes lab abnormalities- renal size usually decreased d. *Diabetes-leading cause of ESRD; then HTN; also glomerulonephritis, cystic disorders, developmental disorders, infectious disease (HIV), neoplasms, obstructive disorders, autoimmune disorders such a s *lupus, *scleroderma; hepatorenal failure, drug toxicity such as recreational heroin, crack cocaine, *NSAIDs e. Stages of renal failure See Table 27.8 p. 776 (*recognize this/ have new classification-PPT slides includes) 1) Stage I: Reduced or decreased renal reserve a) Unaffected nephrons compensate for lost nephrons b) GFR about 50% normal & 50% nephron los c) BUN and creatinine essentially normal (some sources say creatinine doubled here-still without symptoms) d) *patient is asymptomatic. (Important to have baseline serum creatinine; varies for male and female; gradual decline with aging; **makes drugs more toxic due to inability to excrete drugs) 2) Stage II: Renal Insufficiency a) 75% nephron loss b) GFR falls to 20-50% of normal with decreased solute clearance c) Decreased hormone production including activated vit D; have reduced serum calcium; decreased erythropoietin with reduced RBC’s and anemia; etc d) Elevated BUN and creatinine, mild azotemia, decreased ability to concentrate urine; may have nocturia and fixed urine specific gravity e) *Require nephrologists consult at this stage RNSG 2432 257 f) 3) 4) Insult to kidneys-precipitate onset renal failure (infections, dehydration, exposure to nephrotoxins, urinary tract obstructions, certain drugs) g) Require *BP meds; erythropoietin injections, dietary control; use of phosphate binders can delay onset ESRD. (*may have polyuria with low, fixed specific gravity…wastes not cleared; azotemia, anemia, HTN) Stage III-IV: Renal Failure/ESRD a) GFR falls to less than 15-20% normal function b) Less than 5% GFR always considered ESRD: dialysis or transplant required or death occurs c) As 90% or more nephrons destroyed = ESRD, BUN, and creatinine clearance decreases, serum creatine increases, urine specific gravity fixed at 1.010 (if urine produced at all) d) Have *UREMIA; “urine in the blood”-uremic toxins (1) Loss of erythropoietin>chronic anemia (lowered H & H); fatigue (2) Fluid and sodium retention, hyperkalemia, hypermagnesemia, hyperphosphatemia and hypocalcemia; metabolic acidosis due to impaired hydrogen ion excretion *As renal function declines; and end products of protein metabolism (which are typically excreted in urine) accumulate in blood)…all body systems adversely affected B. Manifestations (all body systems affected!) See text page 777 (* review carefully; “why” each body system affected); early manifestations: nausea, apathy, weakness, fatigue; progress to frequent vomiting, increasing weakness, lethargy, confusion 1. 2. Nervous system a. Mood swings; impaired judgment, inability to concentrate and perform simple math functions; psychotic symptoms b. Tremors, twitching, convulsions c. Peripheral neuropathy; “restless legs”, foot drop, sensations crawling, prickling d. High levels of uremic (from elevated BUN) toxins may cause axonal damage; demyelization of nerve fibers; dialysis may not reverse motor neuropathy; should slow general CNS symptoms; anemia also decreases cognition; need at least 33% to function normally e. *Neurologic changes attributed to increased nitrogenous waste products, electrolyte imbalances, metabolic acidosis and axonal atrophy and demyelination of nerve fibers Skin a. Pale, grayish-bronze color due to absorption and retention or urinary pigments that normally give characteristic color to urine; color pale due to anemia b. Dry scaly; severe itching; pruritus due to dry skin plus calciumphosphate deposition in skin and sensory neuropathy 258 RNSG 2432 c. Bruises easily; platelet abnormalities d. Hair dry, brittle and may fall out. e. Uremic frost; urea crystallizes on skin; see only if BUN extremely high 3. Eyes a. Visual blurring and occasional blindness (“Uremic red eye” from irritation due to calcium-phosphate deposits in the eye) 4. Fluid and electrolyte effects a. Urine less concentrated (unable to concentrate; have “fixed urine specific gravity” (*need to understand this); proteinuria and hematuria (lost through the glomerulus) b. Sodium and water retention; if large amounts body water retained, have dilutional hyponatremia; lead to CHF, HTN, edema; may have normal or low sodium levels; *sodium intake must be individually determined, generally restricted to 2 g per 24 hours. Tent shaped “T” c. *Hyperkalemia; muscle weakness, paresthesia, *EKG changes (fatal arrhythmias at 7-8 mEg/L; need to lower when reaches 6 mMEq/L; due to decreased excretion by kidneys, breakdown of cellular protein, bleeding and metabolic acidosis and food); hyperkalemia due to decreased excretion by the kidneys, breakdown of cellular protein, bleeding and metabolic acidosis; also from food, dietary supplements, drugs and IV infusions! (Why does hyperkalemia develop; what are the dangers and how manged-see text p. 105 +*) d. *Hyperphosphatemia, hypocalcemia, hypermagnesia (*kidneys unable to eliminate Mg) Note slide-how does kidney function affect the bone and calcium balance? How is parathyroid hormone effected? See text p. 108+ RNSG 2432 259 1) 2) 3) Calcium and phosphorous> reciprocal relationship; one rises, other decreases a) Decreased kidney filtration leads to increase in serum phosphate level with reciprocal decrease in serum calcium level Renal failure, active vit D lacking; unable to absorb calcium from GI tract; low serum Ca stimulates PTH > resorption of calcium and phosphate from bone; excess phosphate binds with calcium leading to formation of insoluble metastatic calcification deposited throughout the body; develop renal osteodystrophy a) Osteomalacia: lack of mineralization of newly formed bones b) Osteitis fibrosa; calcium absorbed from bones, replaced by fibrous tissues c) Osteoporosis d) Bones fragile, break easily; bone tenderness and pain Magnesium; primarily excreted by kidneys; generally no problem unless client ingests magnesium; Avoid magnesium containing products as milk of magnesium, magnesium citrate, etc. e. Metabolic acidosis 1) 260 RNSG 2432 Impaired kidneys unable to excrete acid load (mostly from ammonia) and from defective reabsorption/regeneration of bicarbonate; Kussmaul respiration, uncommon in chronic renal, reduces severity of acidosis > increases carbon dioxide excretion. *How does Kussmaul breathing do this? (text p. 125) 5. GI effects a. All parts affected-inflammation of mucosa due to excessive urea b. Mucosal ulcerations due to inc. ammonia produced by bacterial breakdown of urea; uremic fetor c. Anorexia, nausea, vomiting, hiccups d. GI bleeding due to GI irritation, platelet defect; diarrhea from hyperkalemia 6. Hematologic a. Anemia typically normocytic, normochromic –dec. erythropoietin; nutritional deficiencies, dec. RBC lifespan b. Iron deficient c. Bleeding tendencies -impaired platelet function d. Impaired immune system 1) WBC decline-changes in leukocyte function and altered immune response; diminished inflammatory response 2) Cellular and humoral immune responses suppressed 7. Cardiovascular effects a. Systemic HTN, usually present prior to ESRD, worsens with sodium retention and inc. extracellular fluid b. Inc. risk for MI, atherosclerotic vascular disease, elevated triglyceride levels c. CHF > pulmonary edema; peripheral edema; arrhythmias from electrolyte imbalances d. Pericarditis: metabolic toxins irritate pericardial sac 8. Endocrine a. Elevated uric acid levels; risk for gout b. Resistance to insulin glucose intolerance c. High triglyceride and elevated HDL resulting in accelerated atherosclerotic process d. *Caution in dosing diabetic who are uremic; insulin is normally excreted by kidneys e. Menstrual irregularities; reduced testosterone levels f. Hypothyroidism g. Gonadal dysfunction C. Therapeutic Interventions/Collaborative Care/Diagnostic Tests (review ARF notes; Text p. 749-751 & Table 27-1) Diagnostic Test/Assessment (*know normal values) 1. Identify CRF (chronic renal failure; monitor renal function by following level or metabolic wastes and electrolytes a. Urinalysis: fixed specific gravity 1.010 (low); excess protein, blood cells, cellular casts b. Urine culture; identify infection c. BUN and serum creatinine; evaluate kidney function 1) Mild azotemia: BUN 20-50 mg/dl 2) Severe renal impairment BUN > 100 mg/dl RNSG 2432 261 3) 4) Uremic symptoms > BUN 200mg/dl *Creatinine levels >4 mg/dl = serious renal impairment (**better indicator than BUN of renal function); elevated BUN –responsible for neurological symptoms (Need to understand this!) d. **Creatinine clearance: reflects GFR and renal function (most accurate; need 24 hour urine collection (see text p. 750) e. *Serum electrolytes: monitored throughout course of CRF f. CBC: moderately severe anemia with hematocrit 20-30%; low hemoglobin; reduced RBC’s and platelets g. Renal ultrasonography: CRF; dec. renal size (see text p. 750 h. Kidney biopsy: diagnose underlying disease process; differentiate acute from chronic (review care of client with renal biopsy, p. 750) D. Management CRF and ESRD (Death if no treatment with ESRD; attempt to delay onset ESRD) See also text p. 786-787 Nursing Care Plan; client with ESRD. Following interventions apply to both (typically…and similar to ARF) Medications *(refer also to p. 750-751; 766-767; 779) 1. General effects of CRF on medication effects a. *Increased half-life and inc. plasma levels of meds excreted by kidneys; monitor carefully b. *Dosage may change when in renal failure; do not give demerol to patients on dialysis (toxic); digitalis excreted largely by kidney* c. Dec. drug absorption if phosphate-binding agents administered concurrently d. *Low plasma protein levels > lead to toxicity when protein-bound drugs are given e. *Avoid nephrotoxic drugs (Aminoglycosides, penicillin in high doses, carefully monitor vancomycin due to toxic accumulation); Amphoteracin B very nephrotoxic ; also contrast-media induced nephrotoxicity f. *If on dialysis; many drugs removed by dialysis; varies with hemodialysis and peritoneal dialysis: CHECK before giving g. Typically do NOT give antihypertensive drugs before hemodialysis (BP may drop); give after dialysis. (work closely with co-nurse & dialysis nurse on this!) 2. Diuretic (furosemide, other loop diuretics -reduce edema; dec. blood pressure, lower potassium) Antihypertensive medications: ACE inhibitors preferred Sodium bicarbonate or calcium carbonate- correct mild acidosis *Oral phosphorus binding agents (calcium carbonate, calcium acetate; Phoslo, aluminum hydroxide)- lower phosphate levels and normalize calcium levels a. Give with meal to act as binding agent b. Give between meals to act as calcium supplement (when calcium agent used) 3. 4. 5. 262 RNSG 2432 6. Aluminum hydroxide (potential for aluminum toxicity) for “acute” treatment of hyperphosphatemia; long term use of aluminum is associated with neurologic symptoms and osteomalacia ; better to use calcium based products for phosphate binding! 7. Vit D supplements-improve calcium absorption (activated vit D3) 8. Meds to correct anemia a. Erythropoietin by injection (Epogen or Procrit….stimulate production RBCs) b. Folic acid, iron supplement to combat anemia (Don’t give iron with phosphate binders, calcium); require multiple vitamin supplements 9. Antacids to treat gastric irritation a. No magnesium based- magnesium toxicity 10. Medications to combat dangerous high potassium levels (*know these…see AFR. Text p. 106 & 107 & 765!) a. Intravenous bicarbonate, insulin glucose b. Sodium polystyrene sulfonate (Kayexalate) How and why do these medications work? Dietary and fluid management (Why can these work?) 1. *Early in CRF: diet modification-slow kidney failure avoid uremic symptoms (usual guidelines) a. Restrict proteins (40gm/day) of high biologic value b. Increase carbohydrate intake (35kcal/kg/day) c. Limit fluid to 1-2 L per day; limit sodium to 2 g/day (usual guideline is 500-600 ml more than previous’ day’s 24 urine output) d. Restrict potassium to (60-70 mEg/day; no salt substitutes); avoid bananas, prunes, raisins, orange juice, tomatoes, deep green and yellow vegetables e. Restrict phosphorus food (especially milk, ice cream, cheese; also meat, eggs, dairy products) to 1000 mg/day *When renal function at approx 5-10% = ESRD…following options must be selected___________________________________________________________ Renal Replacement Therapies; used when medications and dietary modifications no longer effective 1. 2. 3. 4. Hemodialysis: establish vascular access (create AV fistula) months Peritoneal Dialysis: can be initiated when indicated; training of patient and/or family required Transplantation Death Dialysis: manages ESRD; does not cure it* Hemodialysis 1. Hemodialysis See text p. 767 fig 27-5; also text. P. 768 Nursing Care of the Client Undergoing Hemodialysis a. *Uses principles- diffusion and ultrafiltration to remove electrolytes, waste products and excess water (soluble substances and water) from the body through a semi-permeable membrane RNSG 2432 263 (*What is diffusion? What is ultrafiltration? P.767-768-know these definitions) b. Dialysis: diffusion of solute molecules across semipermealble membrane from high to low solute concentration 1) Used to remove excess fluid and metabolic wastes produced in renal failure 2) Dialysate: dialysis solution ; separated from blood by semipermeble membrane 3) Hemodialysis: blood passes through semipermealble membrane filter outside of body 4) Peritoneal dialysis: uses peritoneum surrounding abdominal cavity as dialyzing meembrane; typically used for chronic renal failure. c. Hemodialysis 1) Do 3-4 times a week; takes 3-4 hours at a time 2) Early animal experiments in 1913; first dialysis in 1940; 2 0f 17 patients survived; experimental until 1950’s due to lack of intermittent blood access (only acute renal failure only) 3) 1960-Dr. Scribner developed Schribner shunt; initially “Death Panels” to determine who could dialyze! 1970 congress under Medicare gave access to all for dialysis; 300,000 now on dialysis! d. *Continuous renal replacement therapy (CRRT): used for clients with acute (or chronic) renal failure who cannot tolerate hemodialysis and rapid fluid removal (see text p. 768, 769 and Table 27-6 (CAVH, CAVHD, CVVHD) 1) Blood continuous circulated through highly porous hemofilter from artery to vein or vein to vein; better for less stable clients 264 RNSG 2432 2. Hemodialysis process (*understand principles of operation) Diffusion takes places here a. Blood removed from patient into extracorporeal circuit (flow at about 350-500 ml/min) b. Diffusion and ultrfiltration occurs in dialyzer (long plastic cartridge containing thousands of parallel hollow tubes or fibers which are semi-permeable membrane made of cellulose-based or other synthetic materials. Blood pumped into the top of cartridgedispersed into all of the fibers) c. “Cleaned” blood returned to patient RNSG 2432 265 Locate the dialyzer! d. *Glucose, electrolytes, water can pass through but larger molecules (protein, red blood cells) are blocked from passing through the semipermeable membrane e. Substances can be added to dialysate to diffuse into the blood of the client (i.e. additional K if level is low) 3. Vascular access (the other critical component of hemodialysis!) a. Acute or temporary access gained by inserting double lumen catheter into subclavian, jugular or femoral vein (temporary) 1) Blood drawn from proximal portion of catheter and returned to circulation through distal end of catheter 2) Allow for immediate use; no needle sticks; likely to have poor blood flow; clot easily and become infected 266 RNSG 2432 b. May have “Permanent” central line catheters such as Quinton, Permacaths and newest ones as Lifesite Ports (not often used locally)- provide access into IJ, femoral, subclavian; tunneled 1) Also for immediate use; no needle sticks; good for patients without any other access 2) Lifesite Port; good blood flows, implanted under skin and tunneled into internal jugular (IJ) 3) Note: typically central line access sites -more prone to complications (infections, clotting, etc) a. Require high dosages heparin to maintain flow; risk for bleeding (heparin kept in line) b. Only dialysis nurses/tech access these sites!! c. *Arteriovenous (AV) fistula (click here for direct link)-long term access for dialysis (Text 769, Fig 27-7) 1) Surgical anastomosis of artery and vein in non-dominant arm, usually radial artery and cephalic vein preferred (also called primary AV fistula) RNSG 2432 267 Site for cannulationdialysis of AV fistuals a) b) c) d) Time needed to “mature”; may take even 3-6 months Palpable pulsation (thrill) and bruit on auscultation Less prone to clotting and infections Require “good” vessels for placement d. * Dialysis access using a “graft” (typically also called a fistula, but a synthetic material used -graft “Internal Graft: insertion of internal graft; used when an artery is surgically connected to a vein with a short piece of special tubing placed under the skin. Needles can be inserted in this graft…” 1) 268 RNSG 2432 Surgical insertion of grafting material (Gortex) to connect vein and artery a) Used in clients with poor blood flow etc b) Can use usually within 7-14 days c) More prone to complications than “primary” AV fistula (infections, clotting, poor blood flow) *Note: “primary fistula” and “fistula made with with graft” material serve same purpose…management slightly different! Need to understand difference!!l e. Assess functional fistula/graft for complications (regardless if primary AV fistula or graft) a) Thrombosis: (clotted off); check for palpable thrill, audible bruit b) Infection: check for redness, drainage; more common in AV fistula; requires removal of fistula Graft material used in this photo; listen for bruit, feel for thrill; no BP’s on this arms, no restrictive bands! 1) 4. Prevent complications with fistulas/grafts (*know this!) a) Identify presence of functional fistula/graft b) No BP’s or venipunctures done at fistula/graft site c) No constricting bands above AV fistula/graft and keep elevated especially post surgical insertion d) Recognize complication of “steal syndrome” with AV fistula/graft (decreased blood supply distal to affected site); report and MD treat. Complications of hemodialysis (*important to understand these!) a. Fluid and electrolyte related 1) Hypotension, most common- related to changes in osmolality, rapid removal from vascular department, vasodilation 2) Usual- hold Bp meds prior to dialysis b. Cardiovascular (arrhythmias) c. Bleeding- platelet function and use of heparin during dialysis; potential needle separation during dialysis 1) “Central line” catheters contain 10,000 u Heparin; NEVER for “regular” IV access without specific training/instructions d. Neurologic: seizures (*know why this happens!) 1) Disequilibrium syndrome especially with initial dialysis a) Urea, sodium and other solutes removed more rapidly from blood than from cerebrospinal fluid and brain b) Creates a high osmotic gradient in the brain; causes shift of fluid into the brain and cerebral edema; causes nausea, vomiting, confusion, headaches, twitching and seizures RNSG 2432 269 e. *Infection: local or systemic 1) Staphylococcus aureus septicemia-infected vascular access; high rates of hepatitis B and C, CMV, HIV 5. Dietary & other considerations related to hemodialysis (*understand why needed!) (p. 768; 784-788) a. Fluid restriction ( usual - 1000 cc/24 hours or 500-600 in 24 hours plus previous 24 hours urine output; weigh before and after dialysis; 1 kg = 2.2 lb; 1000 g = 1 kg = 1000 cc/l liter fluid b. **Should not gain more than 1-2 lb between dialysis. How many Kg does this =? How much fluid does this equal? c. Continued phosphorous, potassium, sodium restrictions (slightly more liberalized than prior to starting dialysis) d. Protein- to amount necessary for nitrogen balance; if too high difficult to dialyze waste products; too low, decreased albumin, increased death rate e. Calories to maintain or reach ideal weight f. **Medications: generally hold medications (especially BP) prior to hemodialysis; medications dialyze “out” during dialysis; BP medications may cause the BP to drop (already falls during dialysis!) Check before giving medications prior to dialysis. g. Invasive procedures (wound care, injections, etc, should not be done during or immediately after dialysis, have to bleeding risk due to use of hearin during dialysis. h. Assess for patency of fistula (palpable thrill and audible bruit) i. Never use these access sites or fistula for “regular IV administration of drugs….unless especially instructed to do so! Peritoneal dialysis See text p. 770 fig 27-8 270 RNSG 2432 “Manual” method of peritoneal dialysis-no “cycler” used 1. Peritoneal dialysis: peritoneal membrane used as dialyzing membrane (semi-permeable membrane) a. Warmed sterile dialysate instilled into peritoneal cavity via catheter inserted into peritoneal cavity b. Metabolic waste products and excessive electrolytes diffuse into dialysate while it remains in abdomen c. Water diffusion controlled by glucose (dextrose) concentration in the dialysate which acts as an “osmotic” agent **What is osmosis? d. Amount of solution removed determined by glucose concentration of the dialysate! **Need to understand this concept!! e. Excess fluid/solutes removed more gradually; less risk for unstable client f. Fluid drained by gravity into sterile bag at set interval-removing waste products/ excess fluid 1) “Clear” solution ‘fills” abdomen 2) “Yellow” urine appearing fluid drains out (looks like urine, should be clear) g. Terminology: 1) Dwell time: time that dialysate fluid remains in peritoneal cavity (depends upon types) 2) Fill: fluid infused into peritoneal cavity (usually takes 10-15 minutes) 3) Drain: time fluid drains from peritoneal cavity by gravity flow (usually takes 20-30 minutes) RNSG 2432 271 2. Types of Peritoneal dialysis a. CAPD: most common, continuous ambulatory peritoneal dialysis; exchanges 4-5 times a day; treatments-ongoing 24 hours a day; 7 days a week; 2 liters solution in peritoneal cavity except during drain time; independent treatment b. CCPD: continuous cycler peritoneal dialysis; uses delivery devise (cycler) during nighttime hours and continuous dwell during day The cycler — automatically fills and drains abdomen, usually at night during sleep — can be programmed to deliver specified volumes dialysis solution on specified schedule 3. Complications a. *Infection: peritonitis (dialysate return looks cloudy; abdominal tenderness), tunnel infections, catheter exit site infections; priority problem! b. Hypervolemia: hypertension, pulmonary edema c. Hypovolemia: hypotension d. Hyperglycemia: glucose concentrations high for osmosis for fluid loss; can add insulin to solution; obesity and malnutrition (early satiety due to glucose) 272 RNSG 2432 e. *Hypokalemia: loss of potassium and protein through peritoneal membrane 1) diet liberalized; can have more protein f. Ineffective clearing wastes; gradual 4. Comparison Peritoneal and Hemodialysis (Know this!) Peritoneal Hemodialysis No vascular access & heparin (except placement peritonal catheter) No rapid fluctuation of in extracellular fluid; continuous process Diet liberalized; more protein, personal adjustment of fluid intake by increasing amount of dextrose in dialysate (osmosis to cause loss of fluid) *still should control Na, Mg, Phosphorous intake & fluid… May require less insulin; add insulin to dialysate Potential increased risk for infection (peritonitis) Requires vascular access and heparin Slower process; less effective in waste elimination Increased serum triglycerides Altered body image; weight gain (increased glucose (dextrose intake) Rapid fluid/electrolyte shift; done only 3-4 times a week; 3-5 hours Diet more restrictive; only means to control fluids is by dialysis 3-4 times week and personal regulation fluid intake Onset of dialysis may allow control of diabetes to improve Still at risk for infection; blood borne due to dialysis and vascular access (Hepatitis, HIV) Rapid improvement in fluid and electrole status Improved control of serum triglycerides Minimal body image change Clotting of access site Kidney Transplant 1. 2. 3. 4. 5. 6. 7. Kidney Transplant (See text p. 783, Nursing Care of the Client Having a Kidney Transplant) *important to read & PDS on Liver Transplant Treatment choice for ESRD; limited by availability of kidneys; improves survival and quality of life for ESRD client; 90-95% 1 year survival rate (reverses many of pathophysiological changes of ESRD); may last 25 years; subject to chronic rejection a. Requires life long medications b. Multiple side effects from medications c. Increased risk of tumors d. *Increased risk of infection e. Major surgery Organ donors: majority from cadavers; transplants living donors increasing Close match between blood and tissue type desired; HLA are compared What is HLA? (text p. 233 to recall) Living donors- good physical health; nephrectomy major surgery; remaining kidney must be healthy Cadaver donors; meet criteria for brain death, age varies, free of systemic disease, malignancy or infection including HIV, hepatitis B, C (See Organ Donation PPT program) Kidney removed- preserved by hypothermia RNSG 2432 273 a. Transplant within 24-72 hours (time extended) b. Use technique: continuous hypothermic pulsatile perfusion, and transplant up to 3 days c. Donor kidney placed in lower abdominal cavity, renal artery, vein, and ureter are anastomosed; extraperitoneally in iliac fossa (right preferred); do not remove “old” kidney unless extremely large (polycystic or infection source) 8. Care of the recipient - major surgery; general anesthesia a. Pre-op: 1) 2) 3) b. Post-op 1) 2) 274 RNSG 2432 Answer questions/concerns Remain on dialyisis as ordered Administer immunosuppressive drugs before surgery Careful assessment of renal function (fluid and electrolyte balance) Maintain urinary catheter patency; hourly I&O; keep urine at 100 cc/hr; monitor for ATN (acute tubular necrosis 3) 4) 5) 6) c. *Teach 1) 2) 3) 4) Monitor for BUN, creatinine and creatinine clearance, daily weights, all labs Monitor vital signs and hemodynamic pressure Replace fluids based on urine utput of precious 30-60 minutes (like treating ARF); diuretics as ordered Monitor for complications: a) hemorrhage b) ureteral anastamosis failure (urine leak into periotoneal cavity); dec. urine output with abdominal tenderness/swelling c) renal artery thrombosis; abrupt onset HTN and d) dec. GFR e) infection due to immunosuppression Prevention infection due to immunosuppression (lead to kidney loss); major complication: handwashing, avoid crowds, kids Monitor daily weights; vital signs for inc. temperature; gain in weight (rejection, loss kidney function) Avoid crowds, ills persons, crowds, especially first 3 months Signs of rejections (know them): a) Inc. weight b) Pain and/tenderness over transplant site c) Dec. urine output d) Fever >100 degrees e) Progressive azotemia; protenuria, HTN (chronic f) Rejection > renal failure d. Monitor for rejection see text p. 246 Table 9-3 1) Hyperacute a) Pre-formed antibodies to donor antigen b) function ceases within 24 hours (no treatment; remove kidney) 2) Acute a) cell-mediated mmune response to HLA antigens b) occurs days to months after transplant c) have signs of inflammation; impaired organ function d) 50% experience- differentiate between rejection and medication (cyclosporine) toxicity e) treat with steroids, monoclonial or polyclonal antibodies such as OKT3 or HTG 3) Chronic rejection a) gradual deterioration of organ function b) starts 4 months to years after transplant c) no effective treatment; return to dialysis or retransplant d) *Involves humoral and cellular immune response 9. Responses to transplant & other facts a. Rejection of a first kidney “may not” jeopardize the second. RNSG 2432 275 b. c. d. e. f. g. h. 10. Depression occurs with rejection. The longer a person goes without rejection, the better the prognosis. Leading causes of death are infection, CVA, and MI. Living related donor survival for 1 year is 95%. Living related donor kidney survival for 3 years is 65%. Cadaveric donor survival for 1 year 78%. Cadaveric donor kidney survival for 3 years is 45%. Immunosuppressive medication See also text p. 248-9 Medication Administration & required PDS a. Prednisone (prevent infiltration of T lymphocytes) cornerstone drug: side effects: cushnoid changes; avascular necrosis, GI disturbances, diabetes, infection, risk of tumor b. Cytoxic Agents 1) Azathioprine (Imuran); prevents rapid growing lymphocytes: side effects: bone marrow toxicity, hepatotoxicity, hair loss, infection, risk of tumor 2) Cylosporin (Neoral, Sandimmune); interferes with production of interleukin 2 which is needed for growth and activation of T lymphocytes; side effects: *nephrotoxicity, HTN, heptotoxicity, gingical hyperplasia, infection 3) Cellcept (Mycophenolate); Cyclophosphamide (Cytoxan); newer drugs used instead of Imuran due to decreased toxicity. c. Monoclonal antibody (OKT3 or Orthoclone); used to treat rejection or induce immunosuppression; decreases CD3 cells within 1 hour; side effects: *anaphylaxis, fever/chills, pulmonary edema, risk of infection and tumors (treat prior to administration; reaction increases chance of success) d. Antilymphocyte Globulins: contain antilymphocyte antibodies produced by immunizing horses, etc with human lymphocytes to stimulate production of antibodies; administered to client, binds to peripheral lymphocytes and mononuclear cells, removes them from circulation (must skin test for sensitivity to horse serum prior to use) 1) Antithymocyte globulin (ATG (ATGAM) 2) Antilymphocyte globulin Nursing Care/Collaborative Care (CRF, ESRD & Transplant) 1. 2. Determine stage of renal failure; provide appropriate instruction; critical to caution about drugs, dehydration, etc that may compromise already impaired renal function Nursing diagnoses CRF/ESRD/management with dialysis a. Fluid volume excess rt inability of kidneys to excrete fluid, inadequate dialysis, and excessive fluid intake as manifested by edema, HTN, bounding pulse, weight gain, SOB, pulmonary edema b. Impaired tissue perfusion: renal* text p. 784 276 RNSG 2432 c. Impaired skin integrity rt decrease in oil and sweat gland activity, hyperphosphatemia, deposition of calcium-phosphate precipitates, capillary fragility, excess fluid and neuropathy as manifested by itching, bruising, dry skin, edema, excoriation d. Imbalanced Nutrition: less than body requirements rt restricted intake of nutrients, especially protein, nausea, vomiting, anorexia and stomatitis as manifested by loss of appetite and weight and decreased albumin levels e. Risk for Infection rt suppressed immune system, access sites, and malnutrition secondary to dialysis and uremia f. Risk for injury (fracture rt alteration in the absorption of calcium and excretion of phosphate, altered vitamin d metabolism g. Disturbed body image Kidney transplant (in addition to immediate post-op concerns) a. *Ineffective protection rt effects of medications that compromise immune system, loss of tissue integrity b. *Risk for impaired tissue integrity (graft rejection) rt presence of foreign body c. Risk for infection rt compromised immune system 3. Nursing Care of Client Undergoing Hemodialysis (see text p. 768) a. Note importance of pre-post weights b. Identify medications to be held with dialysis (medication will dialyze out; no BP medications prior to dialysis due to BP fall during dialysis; need for supplement with water soluble vitamins (give after dialysis); antibiotics typically after dialysis c. *Fluid intake restricted unless patient has urine output. d. *Assess vascular access; protect access site e. Assess for complications related to hemodialysis f. Provide for teaching (diet/fluid restrictions/cautions related to access) 4. Nursing Care of Client Undergoing Peritoneal Dialysis (see text p. 771) a. Differentiate between hemodialysis and peritoneal dialysis (food and fluid restrictions, compare advantages/disadvantages of each method b. Instruct in strict aseptic technique in managing peritoneal dialysis c. Instruct regarding signs and symptoms of infection d. Instruct how to manage problems during instillation of dialysate solution 5. Nursing Care of Client Having a Kidney Transplant (see text p. 783) a. Review pre-post-operative care (p. 256a) b. Monitor for signs symptoms of rejection c. Teaching 1) Avoid crowds; immune suppressed 2) Medication compliance; medication information! RNSG 2432 277 278 RNSG 2432