MENOPAUSE AND HRT
advertisement
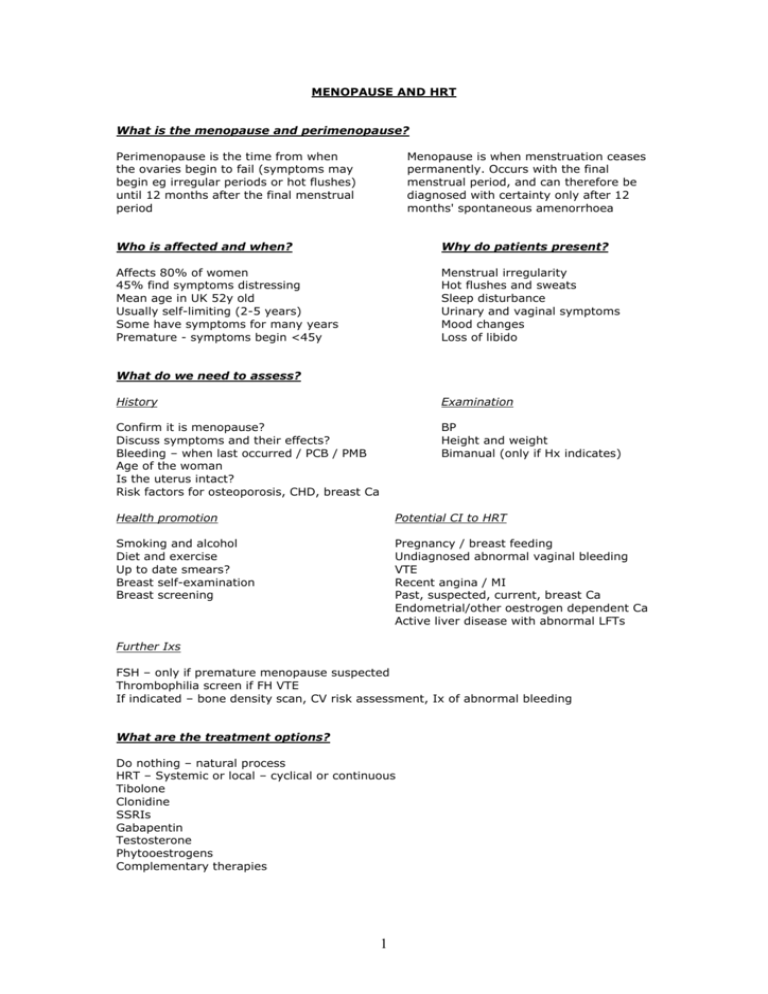
MENOPAUSE AND HRT What is the menopause and perimenopause? Perimenopause is the time from when the ovaries begin to fail (symptoms may begin eg irregular periods or hot flushes) until 12 months after the final menstrual period Menopause is when menstruation ceases permanently. Occurs with the final menstrual period, and can therefore be diagnosed with certainty only after 12 months' spontaneous amenorrhoea Who is affected and when? Why do patients present? Affects 80% of women 45% find symptoms distressing Mean age in UK 52y old Usually self-limiting (2-5 years) Some have symptoms for many years Premature - symptoms begin <45y Menstrual irregularity Hot flushes and sweats Sleep disturbance Urinary and vaginal symptoms Mood changes Loss of libido What do we need to assess? History Examination Confirm it is menopause? Discuss symptoms and their effects? Bleeding – when last occurred / PCB / PMB Age of the woman Is the uterus intact? Risk factors for osteoporosis, CHD, breast Ca BP Height and weight Bimanual (only if Hx indicates) Health promotion Potential CI to HRT Smoking and alcohol Diet and exercise Up to date smears? Breast self-examination Breast screening Pregnancy / breast feeding Undiagnosed abnormal vaginal bleeding VTE Recent angina / MI Past, suspected, current, breast Ca Endometrial/other oestrogen dependent Ca Active liver disease with abnormal LFTs Further Ixs FSH – only if premature menopause suspected Thrombophilia screen if FH VTE If indicated – bone density scan, CV risk assessment, Ix of abnormal bleeding What are the treatment options? Do nothing – natural process HRT – Systemic or local – cyclical or continuous Tibolone Clonidine SSRIs Gabapentin Testosterone Phytooestrogens Complementary therapies 1 Understanding HRT No uterus No need for progestogen protection Either tablet, patch or gels or implants eg Elleste solo (low dose tablet) or Premarin (medium dose tablet) eg Evorel patch (low dose or medium dose version) Periods still happening (Perimenopausal) cyclical combined HRT Either monthly or three monthly Take oestrogen everyday and then progestogen added for 14 days of 28 day cycle therefore regular bleed every 28 days OR oestrogen everyday then progestogen for 14 days every 13 weeks giving a bleed every 3 months eg Elleste duet 1mg (low dose) or Prempak-C 0.625 (medium dose) eg Femapak 40 transdermal patch (2x weekly medium dose) Periods stopped > 1 year ago (Postmenopausal) continuous combined HRT Usually do not have a monthly bleed eg Premique low dose tablets. eg Evorel conti transdermal patch (2x weekly) If sub total hysterectomy then because unsure if any endometrial tissue left usually start with cyclical combined HRT if no bleeding after a 3 months then can stop progestogen and continue oestrogen only HRT Explaining indications for HRT Short term Relief of vasomotor symptoms Long term Prevention / Rx of CVD and osteoporosis (where premature menopause until aged 50y) Explaining benefits of HRT Helps vasomotor symptoms Help urogenital symptoms Prevents osteoporosis (use HRT in premature menopause for this indication) Reduced colorectal Ca risk Explaining potential side effects Oestrogen Breast tenderness Leg cramps Bloating Nausea Headaches Progestogen PMS like symptoms Breast tenderness Backache Depression Pelvic pain Explaining risks to patients Main controversy surrounding HRT is as a result of the Women’s Health Initiative, a US based study, and the Million Women Study based in the UK published between 20022004. Increased risks of: Breast cancer - Risk lower with oestrogen only HRT, risk increases with use Endometrial cancer - Adding cyclical progestogen effectively eliminates risk 2 Ovarian cancer – Risk increases with use VTE - Risk higher with combined HRT CHD - If starting combined HRT >10y after menopause Stroke *IMPORTANT* DO NOT USE HRT if history of above cancers, VTE, CVD, abnormal vaginal bleeding, pregnancy or severe liver disease. Important to explain these risks carefully as generally all women as they get older have increased risks of the above and when you compare groups of women on HRT and a group of women not on HRT the increased risk is very slight. For example for breast cancer In a group of 1000 women aged 50-59 in a 5 year period -10 will get breast cancer -12 will get breast cancer if on oestrogen only HRT (therefore 2 extra cases) -16 will get breast cancer if on combined HRT (therefore 6 extra cases) Generally the risks are greater the longer you take HRT Is contraception required? HRT does not suppress ovulation In those with intact uterus use contraception For 1y after LMP if >50y For 2y after LMP if <50y How to start treatment - Aim to start on lowest dose that controls symptoms After 1-3 years think about HRT break to see if symptoms have settled Vaginal symptoms vaginal cream or pessary Think about whether perimenopausal, post menopausal and whether they have a uterus as this will decide what sort of HRT they will have Then need to decide how to give each hormone as there are various options o Oestrogen options Tablets (remember to start at low dose) Transdermal patch or gel, gel useful if skin irritation occurs with patches Oestrogen implants (usually last resort) If just using local oestrogens initial dose is nightly for 2/52 followed by twice weekly for maintenance o Progestogen options In combined tablets Progestogen tablets separately (provera or utrogestan) Mirena coil: particularly useful if contraception is needed, persistent progestogenic s/e from systemic HRT or when withdrawal bleeds are heavy on sequential HRT and serious causes have been excluded. What about tibolone? Selective oestrogen receptor modulator (SERM) Has oestrogen, progestogenic and androgenic properties Improves sexual function and vasomotor symptoms 3 Increases stroke risk in older women Generally risks outweight benefits if >60y Increases risk of breast Ca recurrence in those with a previous Hx Alternatives Lots of options available with varying levels of evidence: -Evidence for reducing hot flushes Clonidine, SSRI’s (venlafaxine, fluoxetine and paroxetine), Gabapentin, High dose progestogens (MPA- usually only hospital prescribed due to strict criteria) - Lots of herbal remedies on offer. Have to be careful as many of them have oestrogenic properties so wary in people who shouldn’t have oestrogen. Most evidence is for red clover and acupuncture. -Others to consider black cohosh, evening primrose oil, dong quai, ginkgo biloba or ginseng. *Note: Current CKS guidelines does not recommend complementary therapies. 4