Head and Neck Cancer
advertisement
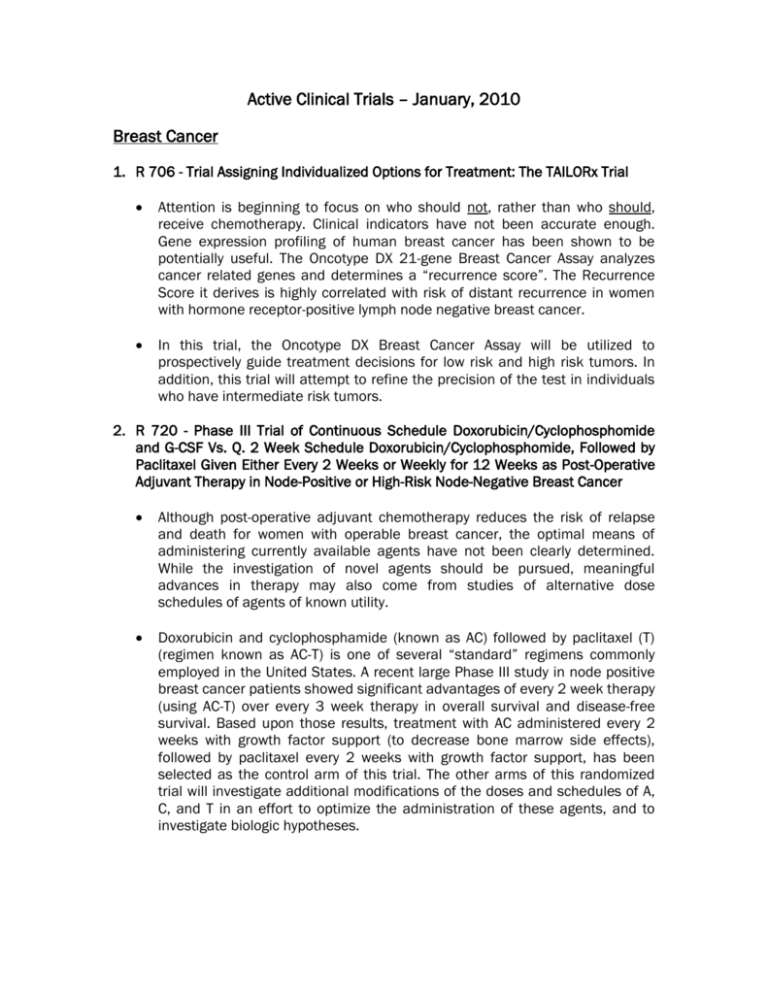
Active Clinical Trials – January, 2010
Breast Cancer
1. R 706 - Trial Assigning Individualized Options for Treatment: The TAILORx Trial
Attention is beginning to focus on who should not, rather than who should,
receive chemotherapy. Clinical indicators have not been accurate enough.
Gene expression profiling of human breast cancer has been shown to be
potentially useful. The Oncotype DX 21-gene Breast Cancer Assay analyzes
cancer related genes and determines a “recurrence score”. The Recurrence
Score it derives is highly correlated with risk of distant recurrence in women
with hormone receptor-positive lymph node negative breast cancer.
In this trial, the Oncotype DX Breast Cancer Assay will be utilized to
prospectively guide treatment decisions for low risk and high risk tumors. In
addition, this trial will attempt to refine the precision of the test in individuals
who have intermediate risk tumors.
2. R 720 - Phase III Trial of Continuous Schedule Doxorubicin/Cyclophosphomide
and G-CSF Vs. Q. 2 Week Schedule Doxorubicin/Cyclophosphomide, Followed by
Paclitaxel Given Either Every 2 Weeks or Weekly for 12 Weeks as Post-Operative
Adjuvant Therapy in Node-Positive or High-Risk Node-Negative Breast Cancer
Although post-operative adjuvant chemotherapy reduces the risk of relapse
and death for women with operable breast cancer, the optimal means of
administering currently available agents have not been clearly determined.
While the investigation of novel agents should be pursued, meaningful
advances in therapy may also come from studies of alternative dose
schedules of agents of known utility.
Doxorubicin and cyclophosphamide (known as AC) followed by paclitaxel (T)
(regimen known as AC-T) is one of several “standard” regimens commonly
employed in the United States. A recent large Phase III study in node positive
breast cancer patients showed significant advantages of every 2 week therapy
(using AC-T) over every 3 week therapy in overall survival and disease-free
survival. Based upon those results, treatment with AC administered every 2
weeks with growth factor support (to decrease bone marrow side effects),
followed by paclitaxel every 2 weeks with growth factor support, has been
selected as the control arm of this trial. The other arms of this randomized
trial will investigate additional modifications of the doses and schedules of A,
C, and T in an effort to optimize the administration of these agents, and to
investigate biologic hypotheses.
3.
R 745 - A Phase 1/2 Study of HKI-272 in Combination with Vinorelbine in
Subjects with Solid Tumors and Metastatic Breast Cancer
This study will investigate the combination of HKI-272 with vinorelbine in
subjects with metastatic breast cancer (MBC) for several reasons. Both drugs
have been shown to be active as single-agent treatment in the MBC
population. In addition, in the preclinical setting, synergy between ErbB-2targeting agent and various chemotherapy agents has been reported, notably,
in a study with trastuzumab
combined with vinorelbine in ErbB-2-overexpressing breast cancer celllines.
HKI-272, by targeting the intracellular ErbB-2 kinase rather than the
extracellular domain, may have different mechanisms of sensitivity and
resistance to trastuzumab, and then may present an advantage in
combination with vinorelbine over the combination oftrastuzumab and
vinorelbine.
Indeed, preliminary phase I and 2 data show that HKI-272 as monotherapy is
associated with a clinical benefit in pretreated subjects, demonstrating some
preliminary efficacy in subjects for whom trastuzumab therapy failed.
Additionally, no significant cardiotoxicity has been reported so far with HKI272 used as a single agent, and no overlapped toxicity is foreseen by
combining HKI-272 with vinorelbine.
Finally, HKI-272 could be a more effective compound than other pan-ErbB
inhibitors to combine with vinorelbine because of its tyrosine kinase inhibition
activity
through an irreversible binding at a targeted cysteine residue in the ATP
binding pocket of the receptor.
3. R 746 – An Open-Label Study of AMG 386 in Combination with Either Paclitaxel
and Trastuzumab or Capecitabine and Lapatinib in Subjects with HER2-postive
Locally Recurrent or Metastatic Breast Cancer
Research has shown that Ang2 overexpression is highly prevalent in the
tumors of subjects with invasive breast cancer and that there is a correlation
between Ang2 expression and worse clinical outcome. In addition, activation
of the HER2 receptor has been shown to lead to downstream up regulation of
VEGF and Ang2, and this increased VEGF and Ang-2 production may be
responsible for the aggressive course of HER2-positive breast cancer.
Together, these data suggest that AMG may have efficacy in combination with
standard of care treatment in subjects with metastatic or locally recurrent
HER2-positive breast cancer.
4. R 752 – A Phase 2, Double-Blind, Randomized, Placebo-Controlled Study of ACE011 for the Treatment of Chemotherapy Induced Anemia in Patients with
Metastatic Breast Cancer
This study is designed to evaluate the efficacy, safety, and tolerability of ACE0II for the treatment of chemotherapy induced anemia in patients with
metastatic breast cancer.
Treatment of patients with metastatic breast cancer with myelosuppressive
chemotherapy is frequently associated with anemia. Chemotherapy induced
anemia (CIA) is a significant problem for patients with cancer, causing fatigue
and reduced quality of life. Patients with CIA are currently treated with blood
transfusion and/or erythropoiesis-stimulating agents. However, with these
treatment options CIA is still an area of unmet medical need.
Erythropoiesis stimulating agents (ESAs) can successfully mitigate
transfusion need in a proportion of these patients, but concerns have
emerged regarding apparent negative effects on survival and/or tumor
progression in certain patient populations. The murine surrogate to ACE-0II,
RAP-0II, has been tested as a single agent in breast cancer cell lines MDA-MB231 and MCF-7 and no effect on enhanced proliferation of these cell lines
has been observed in vitro. Therefore, treatment with ACE-0II may provide a
distinct benefit/risk profile to patients with chemotherapy induced
anemIa.
In both a Phase I single dose and multiple dose study of ACE-0II in
postmenopausal women, increases in hemoglobin and hematocrit were
observed following ACE-0Il treatment and remained elevated over the course
of study. The observed hemoglobin and hematocrit effects of ACE-0II were
dose and time dependent.
Based on the effect of ACE-0lI on hematopoiesis and consistent biological
phenomena observed in both non clinical and clinical studies, it is
hypothesized that the blockade of ActRIIA receptor signaling impedes the
terminal differentiation step in erythropoiesis to allow additional rounds of cell
replication before cells enter the final differentiation phase. The result is a
substantial increase in mature erythrocytes released into the circulation.
Since this proposed mechanism is different to that of known ESAs, ACE-0II
may provide a different clinical profile in the treatment of CIA.
This study will provide information on the pharmacodynamics (PD) properties
regarding the ability of ACE-0II to increase hemoglobin in patients with CIA.
5. R 755 – A Randomized Double-Blind, Placebo-Controlled Study of Everolimus in
Combination with Exemestane in the Treatment of Postmenopausal Women with
Estrogen Receptor Positive, Locally Advanced or Metastatic Breast Cancer Who
are Refractory to Letrozole or Anastrozole
There are currently no treatments specifically approved for postmenopausal
women with ER positive breast cancer after recurrence or progression on a
non steroidal aromatase inhibitor (letrozole or anastrozole). To date
treatment of these patients remains an area of unmet medical need.
Exemestane is an irreversible steroidal aromatase inactivator that has
demonstrated efficacy in the treatment of postmenopausal patients with
advanced breast cancer.
It is indicated for adjuvant treatment of
postmenopausal women with estrogen receptor positive early breast cancer
who have received two to three years of tamoxifen and are swithched to
exemestane for completion of a total of five consecutive years of adjuvant
hormonal therapy.
Everolimus acts as a signal transduction inhibitor. An import aspect of the
anti-tumor effect of everolimus is its potential to act both on tumor cells
directly to inhibit growth and indirectly by inhibiting angiogenesis and
displaying anti-vascular properties. Everolimus and letrozole synergistically
inhibit proliferation in breast cancer cells.
Colorectal Cancer
1. R 709 - A Randomized Phase III Study Comparing 5-FU, Leucovorin, and
Oxaliplatin versus 5-FU, Leucovorin, Oxaliplatin and Bevacizumab in Patients with
Stage II Colon Cancer at High Risk for Recurrence to Determine Prospectively the
Prognostic Value of Molecular Markers
Patients with Stage II colon cancer carry a 20-25% risk of recurrence. There is
a need to identify the subset of patients with stage II colon cancer who are at
greatest risk to develop disease recurrence. Data collected by ECOG and
others suggest that two groups of patients can be defined, high-risk versus
low-risk, based on molecular markers. If these retrospective molecular
observations hold true for patients with stage II colon cancer, it will be
possible to more clearly define a low-risk group that would not require
postoperative therapy. (Low-risk stage II patients would have a 5-year survival
rate of 90%, high-risk 60%.)
In this study, patients determined to be high-risk by the molecular analysis will
receive chemotherapy +/- bevacizumab. Bevacizumab, an anti-VEGF
monoclonal antibody, blocks the growth of cancer cells. Its antitumor effect is
enhanced when combined with chemotherapy, even over that of
chemotherapy alone. A phase II study of bevacizumab plus 5-FU/leucovorin in
patients with metastatic colorectal cancer led to a 40% tumor response rate.
Recently, 5-FU/leucovorin/oxaliplatin (FOLFOX) has been proven to provide
greater disease-free survival than 5-FU/leucovorin alone as adjuvant therapy
for patients with colon cancer. In this study, the investigators propose that
adding bevacizumab to FOLFOX will maximize its effects for the high-risk stage
II patient.
2. R 730 - A Clinical Trial Comparing Preoperative Radiation Therapy and
Capecitabine With or Without Oxaliplatin With Preoperative Radiation Therapy and
Continuous Intravenous Infusion of 5-Fluorouracil With or Without Oxaliplatin in
the Treatment of Patients With Operable Carcinoma of the Rectum
Rectal cancer is a significant problem, with approximately 34,700 new cases
diagnosed each year with an expected overall 5-year survival of 50%. Surgical
resection is the primary therapy, which unfortunately often requires creation
of a permanent colostomy. Due to a high recurrence rate (20 – 40%) with
surgical treatment alone, adjuvant chemoradiation has become standard
practice for the treatment of advanced rectal cancer. However, the optimal
treatment schedule remains unknown.
During the last decade, there has been an increasing interest in the use of
preoperative RT in patients with rectal cancer. The advantage in using it prior
to surgery is the potential to downsize the tumor and possibly change the type
of surgery required from one where a permanent colostomy is necessary to
ananal-sphincter-sparing procedure.
One trial using preoperative RT has shown an overall survival advantage.
Adjuvant radiation therapy alone decreases the local/regional recurrence rate
but not overall survival. Adjuvant chemotherapy alone increases the diseasefree survival and overall survival, but does not affect local/regional
recurrence. NSABP R-02 showed that the addition of RT to adjuvant therapy
significantly decreased the local/regional recurrence rate over chemotherapy
alone. The chemotherapy regimen of %-FU and leucovorin was deemed in this
same study to be the most effective thus far.
Capecitabine is an oral drug which is converted into 5-FU in the body. Because
of its ease of use, potential improvement in the quality of life over continuous
infusion 5-FU, selective concentration in tumor tissue rather than healthy
tissue, more favorable sideeffect profile, and superior effectiveness in
advanced colorectal trials, capecitabine will be investigated in this current
study. Also, the combination of capecitabine and RT yielded highly enhanced
activity in comparison to 5-FU plus RT in a preclinical study.
Oxaliplatin, a platinum derivative, has been shown to be effective in
combination with 5-FU and leucovorin in several trials and has been approved
by the FDA for treatment of advanced colorectal cancer. Various combinations
of oxaliplatin with 5-FU and leucovorin regimens have been studied in the
adjuvant setting. In pilot studies, adding oxaliplatin to pelvic irradiation and
preoperative 5-FU showed significant activity (complete clinical and pathologic
tumor response rates). Additional pilot studies have shown the tolerability of
preoperative pelvic irradiation and oxaliplatin with 5-FU or capecitabine, with
25% or 19% respective complete pathologic tumor responses. It seems
reasonable to attempt to increase the tumor response rates from
preoperative rectal therapy by adding this promising agent to 5-FU or
capecitabine.
3. R 760
A Phase 3, Randomized, Double-blind, Placebo-Controlled Study of
Pegfilgrastim Administered to Subjects with Newly Diagnosed, Locally-Advanced
or Metastatic Colorectal Cancer Treated with Bevacizumab and Either 5Fluororacil, Oxaplatin, Leucovorin (FOLFOX) or 5-fluorouracil, Irinotecan,
Leucovorin (FOLFIRI)
Vascular endothelial growth factor (VEGF) is a critical mediator of tumor
angiogenesis and VEGF has become an important target for anticancer
therapeutics. Bevacizumab (Avastin), a recombinant humanized monoclonal
antibody with a high-binding specificity for VEGF, prevents the interaction of
VEGF with its receptors on vascular endothelial cells and thereby disrupts
angiogenesis.
Pegfilgrastim is a granulocyte colony stimulating factor indicated to decrease
the incidence of infection, as manifested by febrile neutropenia, in patients
with non-myeloid malignancies receiving myelosupresive anti-cancer drugs
associated with a clinically significant incidence of febrile neutropenia,
The addition of bevacizumab to chemotherapy results in increased rates of
neutropenia in each of the tumor types for which bevacizumab has an
indication.
This study will evaluate te efficacy of pegfilgrastim versus placebo in reducing
the incidence of grade 3/4 febrile neutropenia for subjects receiving
bevacizumab and chemotherapy.
Head and Neck Cancer
1. R 705 - A Randomized, Open-Label, Controlled, Phase II Trial of Combination
Chemotherapy With or Without Panitumumab as First-Line Treatment of Subjects
With Metastatic or Recurrent Head and Neck Cancer, and Cross-over-Second-Line
Panitumumab Monotherapy of Subjects Who Fail the Combination Chemotherapy
Only Arm
The goal of treating patients with recurrent Head and Neck Cancer (HNC) is to
relieve symptoms and to extend survival. Metastatic HNC is usually treated
with systemic chemotherapy, which may consist of either single drugs or
combinations. Historically, the most frequently used combination was
cisplatin and 5-FU.
Several newer chemotherapy agents have demonstrated response rates in
metastatic throat cancer that are similar to or higher than those obtained with
the standard cisplatin-5FU combination, i.e. docetaxel combined with
cisplatin.
Over-expression of Epidermal Growth Factor (EGFr) is associated with
malignant transformation in a number of solid tumor types such as prostate,
breast, colon, lung, ovary, kidney, and head and neck. Over-expression of
EGFr in squamous cell carcinoma of the head and neck has been associated
with increased risk of treatment failure.
Panitumumab is a high affinity human monoclonal antibody directed against
human EGFr. In vivo studies have demonstrated that panitumumab prevents
tumor formation and can induce eradication of established tumors in an
orthotopic xenograft model of squamous cell carcinoma of the head and neck.
This study is designed to estimate the effect of adding panitumumab, to
docetaxel and cisplatin combination chemotherapy, on median progressionfree-survival.
Lymphoma
R 739 - A Phase III Multicenter, Open-Label Study of Rituximab Faster Infusion Time
in Patients With Previously Untreated Diffuse Large B-Cell or Follicular Non-Hodgkin's
Lymphoma.
Data from investigator-sponsored, single-center studies, have
demonstrated that faster infusions of rituximab appear to be generally well
tolerated and feasible in patients with NHL.
The primary endpoint of this study is the development of grade 3 or 4
infusion related toxicities in patients who receive rituximab by faster
infusion in Cycle 2 and who did not experience a grade 3 or 4 infusion
related adverse eventr during the rituximab infusion given at the standard
rate in Cycle 1.
Lung Cancer
1. R 719 - A Phase III Randomized Trial of Adjuvant Chemotherapy With or
Without Bevacizumab for Patients With Completely Resected Stage IB-IIIA NonSmall Cell Lung Cancer (NSCLC)
Lung cancer remains the leading cause of cancer death in the United States
and worldwide. Surgical resection is the cornerstone of therapy for early
stage disease, but 30-60% of patients with resected non-small cell lung
cancer (NSCLC) still die of their disease. Between 2003 and 2005, four
randomized controlled trials validated the role of adjuvant chemotherapy for
completely resected NSCLC with survival advantages at 5 years ranging
from 4% to 15%. Adjuvant chemotherapy is now standard care for
completely resected stage IB-IIIA NSCLC.
The next logical step is to attempt to improve upon the survival advantage
found with adjuvant chemotherapy. A promising approach may be the
addition of targeted therapy via bevacizumab. In a randomized Phase III trial
of patients with advanced NSCLC (excluding squamous cell pathology),
standard chemotherapy plus bevacizumab produced increased tumor
response rate, tumor progression-free survival, and overall survival over
chemotherapy alone. Toxicity will be of concern, however, as new data
shows an increase in the rate of low white blood cell count and possible
infection when bevacizumab is given with chemotherapy, as opposed to
chemotherapy alone.
2.
R 700 - A Multi-Center Phase III Randomized, Double-Blind Placebo-Controlled
Study of the Cancer Vaccine Stimuvax (L-BLP25 or BLP25 Liposome Vaccine
in Non-Small Cell Lung Cancer (NSCLC) Subjects With Unresectable Stage III
Disease
Chemotherapy and radical radiotherapy are the standard of care for
unresectable stage III NSCLC even though median survival is often less
than two years with only 15% surviving five years. Given the considerable
toxicity and modest benefit of chemotherapy it is apparent that additional
therapies are required to improve the quality of life and survival duration in
these patients.
There is a growing body of literature describing the potential of
immunotherapy. Much of the focus on cancer immunotherapy has been in
the area of cancer vaccine development, particularly with the identification
of specific antigens associated with cancer.
Recent studies have identified the MUC1 antigen as being associated with
cellular transformation as demonstrated by tumorigenicity and an ability to
confer resistance to genotoxic agents.
MUC1’s ability to protect and
promote tumor cell growth and survival make it an attractive target for
cancer immunotherapy.
L-BLP25 is designed to induce principally a cellular immune response that
may lead to immune rejection of tumor tissues that express MUC1 antigen.
3. R 712 - A Phase 3, Multicenter, Randomized, Placebo-Controlled, Double-Blind
Trial of AMG 706 in Combination With Paclitaxel and Carboplatin for Advanced
Non-Small Cell Lung Cancer
Approximately 60-70% of patients with NSCLC present with advanced
disease that is not amenable to potentially curative surgical resection or
combined modality therapy. For these patients systemic chemotherapy is
the preferred treatment. However, with currently available combination
regimens the 5 year survival rate for patients with stage IIIB disease is 3%
to 7%, and it is <1% for those with stage IV disease.
A carboplatin and paclitaxel combination is frequently used in cancer
patients because of its favorable toxicity profile.
Angiogenesis, the formation of new blood vessels from the existing
vasculature is essential for continued tumor growth and metastasis. One
of the most potent proangiogenic substances is the VEGF family of
cytokines.
VEGF appears to be the single most potent molecule regulating tumor
blood vessel formation.
AMG 706 is a small organic molecule that has been shown in preclinical
pharmacology studies to be a potent, oral, multi-kinase inhibitor with an
anti-angiogenic and anti-tumor activity achieved by selectively inhibiting all
known VEGF receptors, platelet derived growth factor (PDGF) receptor, and
Kit. AMG 706 has an acceptable safety profile in both non-clinical and
clinical studies.
4. R 750 - A Randomized, Double-blind, Placebo-controlled Study to Evaluate the
Long-term Safety and Efficacy of Darbepoetin Alfa Administered at 500 ug Once
Every 3 Weeks in Anemic Subjects With Advanced Stage Non-small Cell Lung
Cancer Receiving Multi-cycle Chemotherapy
Anemia frequently develops in patients with neoplastic disease. The
severity of cancer associated anemia depends in part on the extent of the
underlying neoplastic disease as well as the regimen of cytotoxic
treatments administered.
Symptoms of anemia may include fatigue, dyspnea on exertion, shortness
of breath, decreased motivation, and impaired cognition and depression,
with fatigue affecting greater than 65% of patients during their
chemotherapy treatments.
In situations where rapid reversal of anemia is required RBC transfusion is
indicated, although allogeneic blood product transfusion carries potential
undesirable risks. As an alternative to blood product transfusion,
erythropoiesis stimulating agents (ESAs) have been employed as a
pharmacological measure to palliate and/or reverse the anemia
associated with chemotherapy in non-emergent settings.
Darbepoetin Alfa, manufactured by recombinant DNA technology, has
been reported to have a longer mean residence time and a 3-fold longer
serum half-life than recombinant human erythropoietin in both dialysis and
cancer patients.
5. R 743 - Multicenter, Randomized, Double-blind, Phase III Trial to Investigate the
Efficacy and Safety of Oral BIBF 1120 plus Standard Pemetrexed Therapy
Compared to Placebo plus Standard Pemetrexed Therapy in Patients with Stage
IIIB/IV or Recurrent Non Small Cell Lung Cancer After Failure of First Line
Chemotherapy
Almost all patients with locally advanced and/or metastatic NSCLC relapse
despite the availability of several drugs for second-line monotherapy after
failure of first line therapy.
For these patients, addition of BIBF 1120 could offer a new treatment
option when administered in combination with standard chemotherapy for
second line therapy.
Angiogenesis is involved in tumor growth and development of metastases.
Vascular endothelial growth factor and platelet-derived growth factor
contribute substantially to tumor angiogenesis. BIBY 1120 is a potent
inhibitor of both.
Renal Cancer
R 731 ASSURE: Adjuvant Sorafenib or Sunitinib for Unfavorable Renal Carcinoma
Renal cell cancer (kidney cancer) affects over 33,000 people per year.
Patients with locally advanced renal cell cancer, including Stage II, III, and
IVa, have 5-year survival rates of 65-80, 40-60, and 0-20 percent,
respectively. Those who relapse usually succumb to distant metastases as
a consequence of the lack of useful agents against this cancer (including
biologic agents such as IL-2 and Interferon), both as treatment and as
adjuvant (after surgery) therapy. Adjuvant vaccine trials are ongoing.
Two promising oral targeted therapies have recently been described in
patients with advanced disease. Sorafenib (BAY 43-9006), in a Phase III
trial in advanced pre-treated renal cell cancer, produced a median
disease-progression-free survival of 24 weeks, compared to 12 weeks with
placebo. Sunitinib (SU011248), in two Phase II trials in metastatic renal
cell cancer, has produced a 40-44% tumor response rate, and median
duration of response of 8.1-8.7 months. The great need for safe and
effective adjuvant therapy of renal cell cancer prompts testing of these
new agents, sunitinib and sorafenib, in this setting.
Chemotherapy Induced Nausea and Vomiting
R 761 - A Multicenter, Open-Label, Single-Arm Evaluation of Palonosetron for the
Prevention of Chemotherapy-Induced Nausea and Vomiting (CINV) in Subjects
Who Have Experienced CINV During the Previous Cycle of Low Emetogenic
Chemotherapy (LEC).
Patients receiving LEC agents have a 10% to 30% probability of developing
CINV without prophylaxis/ Current guidelines recommend one antiemetic
agent for patients receiving LEC; however, there is a lack of evidence in
the literature to support a selection of antiemtic therapy in this patient
population.
Palonosetron has demonstrated to be a safe and effective antiemetic in
patients receiving moderate or high emetogenic chemotherapy, but has
not been evaluated in patients receiving LEC.
This study is designed to evaluate palonosetron in the prevention of CI{NV
for subjects receiving a LEC agent.