The role of bronchoscopy in childhood tuberculosis
advertisement

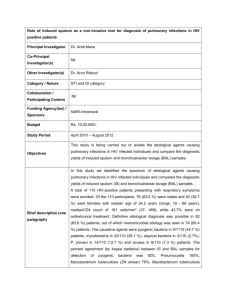
The role of bronchoscopy in childhood tuberculosis Lionel Donato – Clément Ammouche Hôpitaux Universitaires de Strasbourg (France) In children, primary tuberculosis clearly differs from the forms found in adults. Diagnosis and management guidelines should not be extrapolated. Although a key element in the diagnosis, mycobacteriological identification is seldom achieved in children. The younger the patients, the more significant the mediastinal involvement. Substantial airway obstruction sometimes requires specific therapeutic procedures. The flexible bronchoscope (FB) is usually employed for bacteriological sampling purposes and for the assessment and follow-up of endobronchial tuberculosis (ETB). The rigid tube is more suitable for endobronchial debulking maneuvers. Current indications for bronchoscopy in childhood TB remain controversial. They obviously depend on the skills and habits of the endoscopist but also on the institutional environment, available modalities of sedation, paediatric anesthesiologists, dedicated bronchoscopy suite and equipment. Technological advancements in the imaging techniques also tend to balance the indications. FB is useful too when the diagnosis is unclear, as TB can mimic other conditions such as asthma, pneumonia, inhaled foreign bodies, and congenital malformations. More specifically, ETB is an endoscopic differential diagnosis of foreign body inhalation when substantial granuloma formation is generated. Mycobacteriological studies: Mycobacteria detection and isolation can be challenging in children with pulmonary TB. Whatever the specimen collection methods the overall identification rate is poor, partly due to the low density of bacilli but also in relation to the fact that toddlers and preschools have no spontaneous ability to expectorate. Patients with latent forms are usually culture negative. Bacterial sampling is systematically performed in children 1 with a more patent disease (i.e. with clinical or radiological manifestations) in order to: - apply rapid diagnostic tests: i) in patients with confusing symptoms; ii) when resistant strains are suspected in the contamination source - evaluate the patient’s infectivity (presence of acid-fast bacilli on smears; bacterial density semi-quantitative estimation) - obtain cultures to identify the strains and to establish an antibiogram (drug resistance ?) Unfortunately, these goals are difficult to achieve. Repeated gastric aspirates have been described as the gold standard for specimen collection since children swallow rather than expectorate sputum. The yield of this method has been demonstrated superior to the one of bronchoalveolar lavage (BAL) [1]. Sputum induction, stimulated by hypertonic saline nebulization, is proposed as an efficient and low-cost alternative to include the youngest patients. Yet some authors counterbalance its advantages with the increased risk of transmission due to induced coughing and the spreading of droplets, requiring respiratory protection measures that may not be available in many resource-limited regions. Other methods include bronchial brushing and transbronchial needle aspiration biopsy (TBNA), but there is quite no data in the pediatric literature. Several studies have compared the performances of selected collection methods but no global analysis is available regarding the advantages vs drawbacks in the whole set. Choosing the most appropriate one depends on various factors including the geographical burden of the disease and economical constraints. Compared to gastric aspirates and induced sputum, the yield of BAL has been shown to be very low when performed in unselected cases [2]. This is not surprising in paucibacillary latent TB with minimal parenchymal involvement and intact mucosa. Moreover the BAL procedure is usually performed only once and the specimen collection involves a very limited area of the lungs. The sensitivity of BAL is higher in the active forms of the disease and is manifold increased when DNA amplification methods are applied [3]. Although never demonstrated it is clear that BAL sensitivity is maximal when directly performed on visible mucosal changes (ulcerations, caseating lesions) or into large parenchymal infiltrates guided by chest CT-scan. Finally, combining different sampling methods increases the overall detection rate. For instance, gastric aspirates obtain an advantage by being scheduled on the days 2 immediately following bronchoscopy, as the procedure itself improves the bacteriological yield of gastric specimens [4]. In our experience, BAL can demonstrate co-infection with usual microorganisms such as Haemophilus influenzae particularly when ETB lesions are observed. This could explain the fact of why some children with primary TB temporarily improved with nonspecific antibiotics, have delayed diagnosis. Although traditionally considered dangerous in toddlers, TBNA is in fact feasible provided it is guided by careful CT study of the mediastinum (fig.1). The place of the procedure remains to be specified; it could be an option to a surgical approach when facing mediastinal lymphadenopathy of an unknown nature; or when central necrosis is seen on a chest CT-scan but where cultures are negative. Indications are still very few but probably underestimated. Endobronchial tuberculosis assessment: In untreated toddlers, tuberculous mediastinal lymph nodes behave like locally spreading malignant tumors. Dissemination follows the lymphatic ways; the nodes have the potential of invading any adjacent structure with preferential tropism to the central airway. ETB bronchoscopic findings can be classified as follows: - extrinsic compression: mild < 50%; severe > 50%. - bronchial wall invasion with mucosal inflammatory changes and edema; granuloma formation; mucosal ulceration and perforation (caseating matter emission). - long-term after-effects: scar fistula orifice, single or complex; bronchomalacia due to cartilage destruction; circumferential stenosis; and ultimate bronchiectasis development. There is an unresolved debate on the respective place of radiology vs endoscopy in detecting endobronchial involvement. Several semi-recent publications focus on underestimation by X-ray – including chest CT-scan – compared to flexible bronchoscopy [2]. Nevertheless these studies provide little information about the usefulness of detecting minor lesions, as this does not modify the treatment regimen. More recent radiological techniques using 3D-rendering methods allow accurate detection of ETB, thus potentially restricting the need for FB examination [5]. However there is a serious limitation regarding dosimetry when serial studies are needed in children with active disease. 3 The following principles are still widely admitted: 1. in children with no symptoms and normal chest X-ray there is no need for additional investigation if the diagnosis is made clear. 2. CT-scan is indicated first when the chest X-ray demonstrates hilar enlargement or mild parenchymal involvement; FB is next discussed if bronchial wall abnormalities or airway patency impairment are suspected. 3. CT-scan and bronchoscopy are both performed in the case of huge lymphadenomegaly, atelectasis or emphysema, and extended parenchymal infiltrates. 4. FB is indicated whatever the radiological status when bacteriological studies are positive. There is a large agreement for early detection of ETB in order to prevent late sequelae. Antituberculosis drugs show variable effect on lymph node volume; significant enlargement remains sometimes visible for several years irrespective of the antibacterial efficacy. Systemic corticosteroids are added to the 3 or 4 drugs regimen at the early phase of the process when severe extrinsic compression or endobronchial granulation are observed. Serial FB examinations are carried out in order to assess the response - ranging from one to several weeks - and to keep an eye on the occurrence of fistulization that can be promoted by steroids. Failure or worsening lead us to consider interventional procedures in order to restore the airway patency. Interventional bronchoscopy: Intractable airway obstruction can produce definitive pulmonary destruction. Surgical adenotomy has been proposed in order to relieve compression but carries the risk of severe postoperative complications. Tuberculous-infected tissues are weak in nature, bleed easily and show a strong tendency to break in the adjacent connective structures (including vessels) with no clear cleavage plane. Impairment of nutritional status often acts as a pejorative factor. Therefore, endoscopic debulking should always be attempted first. FB is not the most appropriate tool for this purpose except for suctioning mucus or caseum plugs. The rigid bronchoscope can be used by itself as a mechanical drill, by rotating and guiding the bevel through the narrowing structure. Various working 4 instruments can be passed through the tube including endoscopic forceps and scissors, suction tubes, balloon-catheters, electrocautery probes, and laserconducting optical fibres. Purely mechanical disobstruction maneuvers have the drawback of poor visualization due to induced bleeding and carry the risk of imprecise tissue resection (wall laceration, perforation, vascular injury). Interestingly, some laser beams exhibit specific properties that fit these constraints. The CO2 laser is one of them but it is cumbersome for use into the lower pediatric airway. In our experience the KTP laser is more suitable as the beam is carried on by optical fibres, the contact of which causes soft tissue coagulation and necrosis with shallow penetration and very precise cutting action (fig.2). Moreover the KTP wavelength interacts specifically with hemoglobin and thus provides perfect hemostasis. It is therefore a choice piece in the endoscopic armamentarium, allowing accurate photoresection of obstructive granulomas including tuberculous ones [6]. Cicatricial stenoses can be dilated using long-shape balloon catheters. Tracheobronchial stenting for post-tuberculous bronchomalacia has already been described but only in adult patients. References: 1. Abadco DL, Steiner P. Gastric lavage is better than bronchoalveolar lavage for isolation of Mycobacterieum tuberculosis in childhood pulmonary tuberculosis. Pediatr Infect Dis 19992;11:735-8. 2. Bibi H, Mosheyev A, Shoseyov D et al. Should bronchoscopy be performed in the evaluation of suspected pediatric pulmonary tuberculosis ? Chest 2002;122:1604-8. 3. Gomes-Pastrana D, Torronteras R, Caro P et al. Diagnosis of tuberculosis in children using a polymerase chain reaction. Pediatr Pulmonol 1999;28:34451. 4. Singh M, Ashan Moosa NV, Kumar L et al. Role of gastric lavage and broncho-alveolar lavage in the bacteriological diagnosis of childhood pulmonary tuberculosis. Indian Pediatr 2000;37:947-51. 5. Arlaud K, Gorincour G, Bouvenot J et al. Could CT scan avoid unnecessary flexible bronchoscopy in children with active pulmonary tuberculosis ? A retrospective study. Arch Dis Child 2010;95:125-9. 5 6. Donato L, Tran TMH, Mihailidou E. Interventional bronchoscopy. In Priftis KN, Anthracopoulos MB, Eber E, et al (eds). Paediatric bronchoscopy. Prog Respir Res. Basel, Karger 2010, vol.38 pp 64-74. Legend of figures: Figure 1: Intermediate bronchus obstruction in an 18-month-old child with primary tuberculosis a. subcarinal enlargement with no contrast enhancement; note the central necrosis into the lymph nodes and the close relationship with the right pulmonary artery (anterior). b. fine needle puncture through a rigid tube; the child is supine and the right mainstem is right-sided on the picture; the needle is carefully kept away from the anterior wall. Figure 2: endoscopic laser photoresection of tuberculous lymphadenopathy a. complete bronchus obstruction with right middle and lower lobes atelectasis b. bronchus recanalization leading to right lung reventilation; the KTP fibre can be seen at the bottom of the endoscopic picture (green light). 6