POISONING
advertisement

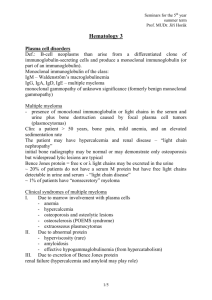
Seminars for the 5th year international students Prof. MUDr. Jiří Horák DRUG ABUSE AND POISONING Drug abuse – a maladaptive pattern in the use of any substance that persists despite adverse social, psychological, or medical consequences. Tolerance – the body‘s ability to adapt to repeated uses of the drug and thus mitigate the drug‘s pharmacologic action. As tolerance increases, higher doses and more frequent administration are required to achieve the desired effect. Physical dependence – results in a physiologic withdrawal syndrome after cessation of drug use. Psychological dependence – can result in alcohol or drug craving and associated behaviours to obtain the drug. Screening - infections (endocarditis, hepatitis B or C, tuberculosis, sexually transmitted diseases, recurrent pneumonias, skin abscesses, HIV infection) - insomnia, mood swings, chronic pain, repetitive trauma, behavioral or social problems Physical findings nedle marks, upper extremity edema, chronic sinusitis, perforated nasal septum from cocaine use Tobacco smoking - the most preventable cause of death in western countries - ~ 420,000 deaths each year in the US - causal link to lung cancer and other malignancies, cardiovascular disease, chronic obstructive pulmonary disease, pregnancy complications, gastrointestinal disorders etc. - passive smoking - implicated in lung cancer, cardiovascular disease, and chronic obstructive pulmonary disease Alcoholism ~ 100,000 deaths per year in the US Pharmacology - 90% metabolized by the liver, the remainder is excreted by the kidneys, lungs, and skin. Its elimination is independent of concentration. Once drinking ceases, blood levels fall ~ 10 to 25 mg/dl/hr. The alcohol dehydrogenase pathway metabolizes alcohol to acetaldehyde, which is then converted to acetate. In both these reactions, NAD is reduced to NADH. Excess NADH → elevated lactic acid and uric acid levels, hyperlipidemia, hypoglycemia, hypoproteinemia, and increased collagen synthesis. Acetaldehyde can promote cellular death. It can block secretion of proteins from hepatocytes → ballooning. 1/9 Seminars for the 5th year international students Prof. MUDr. Jiří Horák Long-term use of alcohol → induction of the MEOS and cytochrome P-4502E1 → development of tolerance and an increase in the metabolism of drugs (pentobarbital, propranolol, tolbutamide, warfarin, diazepam). P-4502E1 converts many foreign substances (solvents, anesthetic agents, cocaine, INH, acetaminophen) into highly toxic metabolites. It activates carcinogens and, coupled with vitamin A deficiency and the increased mutagenicity of tobacco caused by alcohol, may lead to increased incidence of cancers of GIT, lung, and breast. Alcohol-related medical disorders affected organ or system disorder nutrition deficiencies of: folate, B1, B2, B6, niacin, Mg, Zn, Ca, protein brain hepatic encephalopathy, WernickeKorsakoff syndrome, cerebral atrophy, amblyopia, central pontine myelinolysis nerve neuropathy muscle myopathy liver fatty liver, hepatitis, cirrhosis, hepatoma heart hypertension, cardiomyopathy, arrhythmia blood anemia, leukopenia, thrombocytopenia, macrocytosis gut esophagitis and gastritis pancreatitis metabolite and hypoglycemia, hyperlipidemia, hyperuricemia, electrolytes ketoacidosis, hypomagnesemia, hypophosphatemia endocrine pseudo-Cushing‘s syndrome, testicular atrophy, amenorrhea bone osteopenia Acute alcohol intoxication uptake of alcohol into the brain is rapid Blood alcohol levels and symptoms level (mg/dl) sporadic drinkers 50 congenial euphoria 75 gregarious or garrulous 100 incoordinated 125 - 150 unrestrained behaviour 200 – 250 alertness lost, lethargic 300 – 350 chronic drinkers no observable effect often no effect minimal signs pleasurable euphoria effort required to maintain emotional and motor control drowsy and slow stupor or coma 2/9 Seminars for the 5th year international students Prof. MUDr. Jiří Horák > 500 some die coma Fatalities can occur from respiratory depression, hypotension, and acidosis. DD: drowsiness and stupor – hypoglycemia, acidosis, meningitis, subdural hematoma suspected head trauma → CT Th: intubation, hemodialysis if the blood alcohol level exceeds 600 mg/dl Alcohol withdrawal syndrome minor symptoms – tremor, sweating, anxiety, tachycardia, nausea, diarrhea, and insomnia more profound symptoms – tremulousness, hyperactivity, tachycardia, insomnia, nightmares, visual hallucinations, and alcohol craving withdrawal seizures may occur 12 to 48 hours after abstinence delirium tremens – it typically occurs 72 to 120 hours after cessation after a decade or more of fairly heavy drinking: acute delirium, confusion, fear, agitation, gross tremor, insomnia, incontinence, hypertension, tachycardia, profuse sweating, and fever. Delirium tremens may last several days and is a medical emergency – mortality rate 20 to 40% for those not receiving treatment Management of alcohol withdrawal observe and normalize vital signs replace fluids and electrolytes begin sedation with benzodiazepines or barbiturates use haloperidol (1 – 2 mg orally q4h as needed) cautiously for hallucinations or agitation together with benzodiazepines replace folic acid and thiamine measure and replace calcium and phosphate give multivitamin with zinc daily begin beta-blocker or clonidine to reduce adrenergic signs Prescription drug abuse Benzodiazepines can produce both physical and psychological dependence and a potentially dangerous withdrawal syndrome withdrawal symptoms: intense anxiety, insomnia, irritability, weight loss, muscle spasms, palpitations, diarrhoea, sensitivity to light and sound, tremors, and seizures; panic attacks and disturbing nightmares Th: propranolol to reduce tachycardia, hypertension, and anxiety In acute overdose flumazenil 3/9 Seminars for the 5th year international students Prof. MUDr. Jiří Horák Barbiturates acute intoxication: sluggishness, difficult thinking, slurred speech, poor memory and judgment, nystagmus, diplopia, vertigo Th: oral charcoal, alkalinization of the urine (pH > 7.5) with forced diuresis Opioids commonly abused drugs: heroin, morphine, codeine, oxycodone, meperidine, fentanyl Commonly prescribed opioids Agonists morphine methadone meperidine oxycodone propoxyphene heroin hydromorphone fentanyl codeine Mixed agonists-antagonists pentazocine nalbuphine buprenorphine butorphanol Antagonists naloxone naltrexone Opioids act by inhibiting neurons that tonically inhibit dopaminergic neurons, resulting in the increased release of dopamine. Acute opioid overdose usually from injected heroin Clin: cyanosis, pulmonary edema, respiratory distress, coma; also: increased intracranial pressure, seizures, fever, pinpoint pupils The acute syndrome is thought to result mainly from adulterants in the mixture rather than the opiate itself Unsterile intravenous practices → skin abscesses, cellulitis, meningitis, thrombophlebitis, endocarditis, hepatitis, and HIV infection Th of acute overdose: naloxone i.v., repeat in 2 to 3-minute intervals (titrate carefully – risk of acute withdrawal symptoms in dependent patients) 4/9 Seminars for the 5th year international students Prof. MUDr. Jiří Horák Response within minutes: increases in pupil size, respiratory rate, level of alertness Withdrawal symptoms develop 6 – 10 hours after the last injection of heroin: drug craving, anxiety, restlessness, irritability, rhinorrhea, lacrimation, sweating and yawning develop early. Later: dilated pupils, piloerection, anorexia, nausea, vomiting, diarrhea, muscle spasms, abdominal cramps, bone pain, myalgias, tremor, sleep disturbance. These symptoms peak at about 36 to 48 hours and then subside over 5 - 10 days if untreated. There can be a protracted abstinence syndrome up to 6 months (mild anxiety, sleep disturbance, bradycardia, hypotension). Withdrawal can be managed with methadone (a long-acting synthetic agonist drug). Patients with repeated relapses can be maintained on methadone in doses of 60 mg or more daily. It may be used for years. Amphetamines The most frequently abused amphetamines are: dextroamphetamine, methamphetamine, methylphenidate, ephedrine, and phenmetrazine. They have been used for weight reduction, attention deficit disorder, and narcolepsy. They inhibit dopamine reuptake and release dopamine from intracellular stores. Tolerance develops rapidly to the stimulant effects. Toxic effects resemble acute paranoid schizophrenia with delusions and hallucinations. Withdrawal symptomes are similar to those seen with cocaine. Acute amphetamine toxicity: excessive sympathomimetic effects – tachycardia, tremors, hypertension, hyperthermia, arrhythmias. Chronic users may have an increased incidence of schizophrenia. Th: a quiet environment, benzodiazepines for anxiety. Urine acidification with ammonium chloride may accelerate amphetamine excretion. Illicit drug abuse Cocaine - a naturally occuring alkaloid derived from the coca plant. Its use has increased dramatically over the past decade. The „crack“ form. It is highly addictive. Cocaine can be ingested orally or by snorting, injecting i.v., or smoking crack. The blood half-life is ~ 1 hour. Its major metabolite benzoylecogonine can be detected in the urine for 2 to 3 days after a single dose. Through smoking, high brain levels are obtained within seconds. An intense, pleasurable reaction lasting about 20 to 30 minutes is followed by rebound depression, agitation, insomnia, and anorexia and later by fatigue, hypersomnolence, and hyperphagia (the „crash“). This typically lasts 9 to 12 5/9 Seminars for the 5th year international students Prof. MUDr. Jiří Horák hours. Users repeat the sequence at short intervals to recapture the euphoric state and avoid the crash. Cocaine blocks the reuptake of dopamine by binding strongly to the dopamine reuptake transporter at presynaptic nerve endings. Physiologic responses are related to catecholamine excess: tachycardia, hypertension, hyperthermia, agitation, peripheral vasoconstriction, seizures, tachypnea, pupillary dilatation, and anorexia. The most devastating medical complications relate to the cerebrovascular and cardiovascular effects of cocaine: potent vasoconstriction of the cerebral arteries may result in acute stroke, of the coronary arteries → myocardial ischemia and arrhythmias (AIM rare). Th of myocardial ischemia: benzodiazepines, nitrates, phentolamine (alphaantagonist). For cocaine-induced hypertension or tachycardia, metoprolol or labetalol is effective. Th of cocaine intoxication: obtain vascular and airway access; benzodiazepines repeatedly i.v. to control CNS agitation. Most patients suffer psychological dependence with intense craving for cocaine, along with fatigue and depression. Relapse is common and very difficult to treat. Cannabis The cannabinoid drugs include marijuana (the dried flowering tops and stems of the resin-producing hemp plant) and hashish (a resinous extract of the hemp plant). Main drug is delta-9-tetrahydrocannabinol. This drug is intensely lipophilic and is absorbed by the lung. Metabolites can be detected in the urine for 2 to 3 days following casual drug use and up to 4 weeks in chronic users. The primary mode of ingestion is smoking. Acute physiologic effects: increase in heart rate, conjunctival congestion, decreased intraocular pressure, bronchodilation, peripheral vasodilation, dry mouth, fine tremor, muscle weakness, and ataxia. Psychoactive effects: euphoria, enhanced perception of colours and sounds, drowsiness, inattentiveness. Motor vehicle driving is impaired. Tolerance and physical dependence occur. Th: supportive and reassuring. Benzodiazepines can be used in severely agitated patients. Amotivational syndrome in some chronic users. Psychedelics LSD (lysergic acid diethylamide) is the most potent psychedelic drug known. It interacts with several serotonine receptors in the brain but the actual psychoactive mechanism is not known. Within 20 minutes of oral ingestion, sympathomimetic effects occur (mydriasis, hyperthermia, tachycardia, elevated blood pressure, increased alertness, tremors, and occasional nausea and vomiting). Within 2 hours, psychoactive effects 6/9 Seminars for the 5th year international students Prof. MUDr. Jiří Horák occur with heightened perceptions, body distortions, variable mood, and possible visual hallucinations. After 12 hours the syndrome starts to clear. An acute psychotic or panic reaction may occur. Phencyclidine is now the most widely abused of the group. Prompt stimulant effect similar to that of amphetamines: feeling of euphoria, power, and invincibility. Physical examination: hypertension, tachycardia, bidirectional nystagmus, hyperthermia, hallucinations, extreme agitation, ataxia, and slurred speech. Patients can have hypertensive crises, seizures, and bizzare, often violent behaviour. Overdosing can result in death. The major problem is drug craving. Th: a quiet environment, sedation with benzodiazepines, hydration, and haloperidol for terrifying hallucinations. Inhalants Organic solvents: toluene, kerosene, gasoline, acrylic paint spray, carbon tetrachloride, degreasors. Solvents are inhaled by children or young adolescents and can produce dizziness and intoxication within minutes. Prolonged exposure can cause bone marrow depression, cardiac arrhythmias, cerebral degeneration, and damage to the liver, kidney, and the peripheral nervous system. Amyl nitrite is a volatile liquid that dilates smooth muscle and is used as a sexual enhancer. It is usually sprayed into the nose and can produce flushing, dizziness, and a feeling of a rush. No chronic toxicity has been reported. Acute poisoning General approach to the poisoned patient 1. Emergency management 2. Clinical evaluation 3. Elimination of the poison from the GIT etc. 7/9 Seminars for the 5th year international students Prof. MUDr. Jiří Horák 4. 5. 6. 7. Administration of an antidote Elimination of any absoberd substance Supportive therapy Observation and disposition Emergency antidotes Poison Acetaminophene Atropine Benzodiazepines Beta-blockers Calcium channel blockers Carbon monoxide Cyanide Digitalis Hydrofluoric acid Iron Lead Mercury Arsenic Gold Methyl alcohol Ethylene glycol Nitrites Opiates Organophosphates Tricyclic antidepressants antidote N-acetylcysteine physostigmine flumazenil glucagon calcium oxygen amylnitrate sodium thiosulfate sodium nitrate Digibind FAB antibodies calcium deferoxamine dimercaptosuccinic acid dimercaprol ethyl alcohol methylene blue naloxone atropine pralidoxime sodium bicarbonate Methods for elimination of absorbed substance Alkaline diuresis Phenobarbital Salicylate Hemodialysis Ethylene glycol Lithium Methanol Salicylates Theophylline Hemoperfusion Barbiturates 8/9 Seminars for the 5th year international students Prof. MUDr. Jiří Horák Theophylline -------------------- 9/9