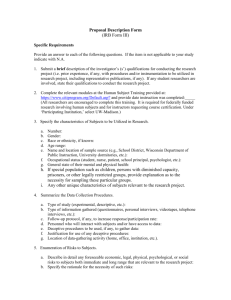
iii. study documentation - Research Conduct and Compliance Office
advertisement

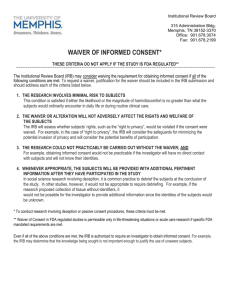
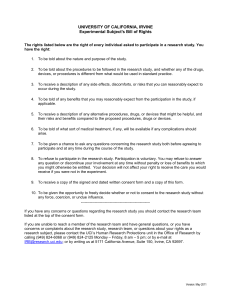
INTRODUCTION In the conduct of research, attention to detail is of utmost importance to help ensure the integrity of the study data and adherence to the regulations and guidelines that govern human subject research. Throughout their years of conducting audits, the Education and Compliance Office for Human Subject Research (ECO-HSR) at the University of Pittsburgh has identified practices that facilitate compliance with research regulations and improve the conduct of research with human subjects. The attached document provides a reasonable summary of good clinical research practices. This summary is not meant to be all-inclusive but highlights practices that we hope will assist you in the conduct of your research study. Please note that only those investigators who are conducting FDA-regulated human subjects research are obligated to follow Good Clinical Practices, as discussed at length in “The International Conference of Harmonization - Good Clinical Practices,” referenced below. Nevertheless, good clinical research practices, as summarized in our attached document, are a standard to which all researchers should aspire, and this is the set of standards used by the ECOHSR staff in conducting their audits of research studies. For investigators not conducting FDAregulated research studies, we understand that certain of our recommended procedures may be modified to reflect the nature of the research study and the likely risks to human subjects. The summary includes information gathered from: Observed practices in the research community The Reference Manual for Use of Human Subjects in Research http://www.irb.pitt.edu The Federal Policy Regulations (CFR 45 Part 46) http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm The FDA Regulations (CFR 21 Parts 50, 56 and 312 ) http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/cfrsearch.cfm and The International Conference of Harmonization - Good Clinical Practices http://www.fda.gov/cder/guidance/959fnl.pdf . If you have any questions or comments about this material, please contact The Education & Compliance Office for Human Subject Research at staff member of the Education and Compliance Office. HIGHLIGHTS OF GOOD RESEARCH PRACTICE FOR PSYCHOSOCIAL/DESCRIPTIVE STUDIES I. PROTOCOL ADHERENCE AND OVERSIGHT A. Prior to initiation of the study: 1. Ensure that all study staff have completed the designated Responsible Conduct in Research computer based training modules and other applicable training (e.g., universal precautions, shipping of biological specimens). Training requirements can be found by going to http://cme.hs.pitt.edu and clicking on the “What is Required?” link. 2. Ensure that the study and consent form(s) have received IRB approval and that the approval is current. The IRB Website is located at: http://www.irb.pitt.edu/ 3. Ensure availability of facilities, equipment, and all supplies to enable the performance of all procedures per protocol. 4. Ensure preparation of case report forms/data collection tools to document eligibility criteria and the performance of all study procedures per the IRB approved protocol. 5. Ensure that the IRB protocol includes a comprehensive list of all study surveys/assessment tools (using the title listed on the tool itself) and that all acronyms are spelled out in full. 6. Identify components/members of the DSMP/DSMB and outline responsibilities of each member; provide a schedule for regular meetings, based on study needs/complexity. Data and safety monitoring plans are addressed in Appendix L of the Reference Manual for Use of Human Subjects in Research, (The IRB Reference Manual). 7. Review study procedures and documentation with study staff: Provide a copy of the complete current version of the research protocol and consent form to all members of the research team, i.e., all coinvestigators and other personnel assisting with the conduct of the study Delegate/assign responsibilities (ensure that assignment of personnel delegated to obtain signed consent is consistent with IRB requirements and the IRB approved protocol) Review case report forms, when and how used, and how to make corrections Review randomization plan Review use of any special equipment Review methods for subject record identification and protection of confidentiality 8. B. Review storage of study records/computer data to maintain confidentiality Address who has access to the records. If blood/tissue samples will be stored, ensure availability of proper storage site and adequate oversight of the facility. If samples will be shipped to an outside site, ensure proper shipping containers/procedures are available. Also ensure that staff responsible for shipping have received appropriate training and/or certification. If samples are to be shipped to another site, a material transfer agreement may need to be executed. Details about material transfer agreements can be found on the Office of Research website at: http://www.pitt.edu/~offres/mta.html. Throughout the course of the study: 1. Maintain current IRB approval of the protocol and informed consent document(s). 2. Ensure that any modifications to the protocol/consent form are submitted to the IRB for review and approval prior to their implementation. 3. Ensure that informed consent is obtained from all subjects and the original signed consent document is retained in the study records. 4. Ensure that all study procedures are conducted per the IRB approved protocol. 5. Report unanticipated problems and adverse events per IRB requirements. Unanticipated problem and adverse event reporting is addressed in Chapter 3 of the Reference Manual for Use of Human Subjects in Research. Reporting forms are located online at: http://www.irb.pitt.edu/irbforms/irbforms.htm. 6. Ensure that adequate, current and accurate records of research data, outcomes, and adverse events are maintained to permit an ongoing assessment of the risks and benefits of study participation. 7. Review subject files for notes to file explaining any protocol variations or deviations. Notify the sponsor and the IRB of deviations and corrective actions to prevent recurrence. 8. If blood/tissue samples are being collected and stored, ensure proper storage (e.g., temperature of refrigerator, secure location). 9. Maintain ongoing communication with study staff to address problems/concerns in a timely manner. Maintain minutes of staff meetings. 10. Ensure conduct of DSMP/DSMB meetings as indicated in the IRB approved protocol. Maintain minutes of meetings. C. 11. Perform interim analysis, as required per protocol. 12. When the research is sponsored by an external agency (e.g., NIH; NSF), maintain records of communications with the sponsor (i.e., e-mails, letters, monitor visits, and a log of telephone conversations). Upon completion of study: 1. Ensure that all documentation is complete (or provide notes to file explaining omissions). 2. Prepare and submit final report to sponsor, if applicable. Notify IRB that the study is terminated and submit the necessary summary report. 3. Retain and store subject records per requirements of IRB (UP IRB is five years after termination of the study) and/or sponsor. Note: Retain records for the longer time period, if differing dates. II. CONSENT PROCESS A. Conducting the Informed Consent Process 1. Ensure that the IRB has granted approval and that the consent document is the most current version. Information on each page of the consent should list: University of Pittsburgh IRB # Current Approval Date Most Recent Modification Approval Date (if applicable) Renewal Date 2. For studies with risk of emotional distress that may lead to physical harm (i.e., suicide), assure that emergency contact information is provided on the first page of the consent document. The subject must be able to reach a "member of the research team" within two phone calls at all times. 3. Ensure that the individual conducting the consent process is authorized to do so as outlined in the protocol. If someone other than an investigator is delegated to conduct the process, it must be explained in the protocol and approved by the IRB. 4. The subject or legally authorized representative must provide written consent prior to ANY research activities unless certain activities have received a waiver of the requirement to obtain signed informed consent from the IRB (e.g., phone screening). Informed consent is addressed in Chapter 8 of the IRB Reference Manual. B. Documenting the Process 1. Ensure that the consent document is properly signed and dated. All signatures must be obtained at the time the subject provides consent. The subject or legally authorized representative must sign and date the consent document. The investigator or authorized delegate must sign and date the consent document. All signatories must date their own signature. If there are any discrepancies (i.e., dates), a narrative note must be included in the research record explaining the circumstances. 2. It is recommended but not required that in addition to the signed consent document, a narrative note of the informed consent "process" should also be included in the research records. This is most likely to be the case when studies include an intervention or where risks to participants are more than minimal. The note should include reference to: who was present during the discussion, that all risks were presented, that all questions were answered, and that the subject appears to understand and provides consent to participate by signing the consent document prior to any research procedures. This narrative note should be signed, dated and the time recorded by the individual writing the narrative note. Recording the time the consent was signed is most important when research procedures are to be performed on the same day that consent is obtained. 3. The principal investigator must retain the original signed consent document. A copy must be given to the subject. A copy should be placed in the clinic/hospital record. 4. If any problems are identified, i.e., lost or missing consent forms and/or use of an incorrect/outdated consent form, document the findings and contact the IRB for guidance and instructions. III. STUDY DOCUMENTATION A. Source Documents Source documents are the original documents containing the first recording of information used as research data. If these documents are generated in the course of routine care, copies of the documents should be maintained in the subjects research file. 1. Data collection tools should be developed and completed to address all study activities. This includes: Eligibility criteria Screening Study procedures Follow-up procedures 2. Supportive documentation should also be included in the research subject’s file, e.g., Psychological assessment tools Bloodwork results Results of other tests/procedures 3. Narrative notes should also be generated to document: how the subject tolerated the study procedures, any telephone calls or contacts with the subjects, missed visits or protocol deviations, and adverse events. 4. All subject-specific source documents should be labeled with subject ID and the date and should be signed and dated by the person completing the document. 5. Separate research records should be maintained. Investigators should not rely on clinical records to maintain research documentation. 6. If corrections need to be made to source documents or case report forms: draw a single line through the error note the correct information beside the error initial and date the correction place a note to file explaining the reason for the correction and if applicable describe the corrective actions that will be taken to avoid a future reoccurrence of the error. Note that white-out should never be used to correct research documentation. B. Regulatory Binder/Files All investigators must maintain regulatory binders/files that contain all vital study documentation. The files should be organized in such a manner that they can be easily retrieved and documents located. The regulatory file should contain the following items. Protocol Informed consent Investigators’ CV’s Copies of professional licenses Training certificates IRB approval/correspondence Sponsor/granting agency correspondence Signature list of research staff Monitoring log/reports Adverse event reports Minutes from staff meetings DSMP/DSMB meeting minutes Final study report Note: It is acceptable to establish a “central departmental file” for documentation that pertains to all studies conducted within that department. A cross-reference note should be placed in the specific study regulatory binder noting where these documents are located. For example, the central file may contain: Investigator/staff CVs / licenses / certificates Staff training records HIGHLIGHTS OF GOOD RESEARCH PRACTICE FOR MEDICAL/INTERVENTIONAL STUDIES I. PROTOCOL ADHERENCE AND OVERSIGHT A. Prior to initiation of the study: 1. Ensure that all study staff have completed the designated Responsible Conduct in Research computer based training modules (and applicable training (e.g., universal precautions, shipping of biological specimens). Training requirements can be found by going to http://cme.hs.pitt.edu and clicking on the “What is Required?” link. 2. Ensure that the study and consent form(s) have received IRB approval and that the approval is current. The IRB Website is located at: http://www.irb.pitt.edu/ . 3. Ensure availability of facilities, equipment, drugs, and all supplies to enable the performance of all procedures per protocol. 4. Ensure preparation of case report forms/data collection tools to document eligibility criteria and the performance of all study procedures per the IRB approved protocol. 5. Ensure that the IRB protocol includes a comprehensive list of all study surveys/assessment tools (using the title listed on the tool itself) and that all acronyms are spelled out in full. 6. Identify components/members of the DSMP/DSMB and outline responsibilities of each member; provide a schedule for regular meetings, based on study needs/complexity. Data and safety monitoring plans are addressed in Appendix L of the Reference Manual for Use of Human Subjects in Research, (The IRB Reference Manual). 7. Review study procedures and documentation with study staff: Provide a copy of the complete current version of the research protocol and consent form to all members of the research team, i.e., all co-investigators and other personnel assisting with the conduct of the study Delegate/assign responsibilities (ensure that assignment of personnel delegated to obtain signed consent is consistent with IRB requirements and the IRB approved protocol) Review case report forms, when and how used, and how to make corrections Review randomization plan; drug/device accountability and storage Review use of any special equipment Review methods for subject record identification and protection of confidentiality Review storage of study records/computer data to maintain confidentiality. Address who has access to the records. 8. If blood/tissue samples will be stored, ensure availability of proper storage site and adequate oversight of the facility. If samples will be shipped to an outside site, ensure proper shipping containers/procedures are available. Also ensure that staff responsible for shipping have received appropriate training and/or certification. If samples are to be shipped to another site, a material transfer agreement may need to be executed. Details about material transfer agreements can be found on the Office of Research website at: http://www.pitt.edu/~offres/mta.html. B. Throughout the course of the study: 1. Maintain current IRB approval of the protocol and informed consent document(s). 2. Ensure that any modifications to the protocol/consent form are submitted to the IRB for review and approval prior to their implementation. 3. Ensure that informed consent is obtained from all subjects and the original signed consent document is retained in the study records. 4. Ensure that all study procedures are conducted per the IRB approved protocol. 5. Report unanticipated changes and adverse events per IRB, sponsor, and hospital requirements. Unanticipated changes and adverse event reporting is addressed in Chapter 3 of the Reference Manual for Use of Human Subjects in Research. Reporting forms are located online at: http://www.irb.pitt.edu/irbforms/irbforms.htm. 6. Ensure that adequate, current and accurate records of research data, outcomes, and adverse events are maintained to permit an ongoing assessment of the risks and benefits of study participation. 7. Review subject files for notes to file explaining any protocol variations or deviations. Notify sponsor and IRB of deviations and corrective actions to prevent recurrence. 8. Review investigational product accountability on a regular basis. 9. If blood/tissue samples are being collected and stored, ensure proper storage (e.g., temperature of refrigerator, secure location). 10. Maintain ongoing communication with study staff to address problems/concerns in a timely manner. Maintain minutes of staff meetings. 11. Ensure conduct of DSMP/DSMB meetings as indicated in the IRB approved protocol. Maintain minutes of meetings. 12. Perform interim analysis, as required per protocol. 13. Maintain record of communications with the sponsor (i.e., e-mails, letters, monitor visits, and a log of telephone conversations). C. Upon completion of the study: 1. Ensure that all documentation is complete (or provide notes to file explaining omissions). 2. Return or destroy investigational product per sponsor’s requirements. 3. Prepare and submit final report to sponsor. Notify IRB that the study is terminated and submit the necessary summary report. 4. Retain and store subject records per requirements of IRB (UP IRB is five years after termination of the study) and/or sponsor. Note: Retain records for the longer time period, if differing dates. II. CONSENT PROCESS A. Conducting the Informed Consent Process 1. Ensure that IRB has granted approval and that the consent document is the most current version. Information on each page of the consent should include: University of Pittsburgh IRB # Current Approval Date Most Recent Modification Approval Date (if applicable) Renewal Date 2. For studies with risk of physical harm, assure that emergency contact information is provided on the first page of the consent document. The subject must be able to reach a "member of the research team" within two phone calls at all times. 3. Ensure that the individual conducting the consent process is authorized to do so as outlined in the protocol. If someone other than an investigator is delegated to conduct the process, it must be explained in the protocol and approved by the IRB. 4. The subject or legally authorized representative must provide written consent prior to ANY research activities unless certain activities have received a waiver of the requirement to obtain signed informed consent from the IRB (e.g., phone screening). Informed consent is addressed in Chapter 8 of the IRB Reference Manual. B. Documenting the Process 1. Ensure that the consent document is properly signed and dated. All signatures must be obtained at the time the subject provides consent. The subject or legally authorized representative must sign and date the consent form. The investigator or authorized delegate must sign and date the consent form. All signatories must date their own signature. If there are any discrepancies (i.e., dates), a narrative note must be included in the research record explaining the circumstances. 2. If the study involves a drug, device or surgical procedure, an investigator who is listed on the first page of the consent form and who is an MD, must participate in the informed consent process. This investigator MUST sign and date the informed consent document. 3. In addition to the signed consent document, a narrative note of the informed consent "process" should also be included in the research records. The note should include reference to: who was present during the discussion, that all risks were presented, that all questions were answered, and that the subject appears to understand and provides consent to participate by signing the consent document prior to any research procedures. This narrative note should be signed, dated and the time recorded by the individual writing the narrative note. Recording the time the consent was signed is most important when research procedures are to be performed on the same day that consent is obtained. 4. The principal investigator must retain the original signed consent document. A copy must be given to the subject. A copy should be placed in the clinic/hospital record. 5. If any problems are identified, i.e., lost or missing consent forms and/or use of an incorrect/outdated consent form, document the findings and contact the IRB for guidance and instructions. III. STUDY DOCUMENTATION A. Source Documents Source documents are the original documents containing the first recording of information used as research data. If these documents are generated in the course of routine medical care, copies of the documents should be maintained in the subjects research file. 1. Data collection tools should be developed and completed to address all study activities. This includes: Eligibility criteria Screening Study procedures Drug dispensing Follow-up procedures 2. Supportive documentation should also be included in the research subject’s file, e.g., Psychological assessment tools Bloodwork results X-ray reports Electrocardiograms 3. Narrative notes should also be generated to document: how the subject tolerated the study procedures, any telephone calls or contacts with the subjects, missed visits or protocol deviations, and adverse events. 4. All subject-specific source documents should be labeled with subject ID and the date and should be signed and dated by the person completing the document. 5. Separate research records should be maintained. Investigators should not rely on medical records to maintain research documentation. 6. If corrections need to be made to source documents or case report forms: draw a single line through the error, note the correct information beside the error, and initial and date the correction, and place a note to file explaining the reason for the correction and if applicable describe the corrective actions that will be taken to avoid a future reoccurrence of the error. Note that white-out should never be used to correct research documentation. B. Regulatory Binder/Files 1. All investigators must maintain regulatory binders/files that contain all vital study documentation. The files should be organized in such a manner that they can be easily retrieved and documents located. The regulatory file should contain the following items. 2. Protocol Informed consent Investigators’ CV’s Copies of professional licenses Training certificates IRB approval/correspondence Sponsor/granting agency correspondence Signature list of research staff Monitoring log/reports Adverse event reports Minutes from staff meetings DSMP/DSMB meeting minutes Final study report If applicable to the study design, the following may also apply: Investigator’s brochure Form FDA 1572 (or Investigator’s Agreement) Drug accountability documentation Laboratory certifications and range of normal laboratory values Note: It is acceptable to establish a “central departmental file” for documentation that pertains to all studies conducted within that department. A cross-reference note should be placed in the specific study regulatory binder noting where these documents are located. For example, the central file may contain: Investigator/staff CVs / licenses / certificates UPMC laboratory certifications and range of normal laboratory values Staff training records C. Test Article Accountability 1. Note that the Investigational Drug Service, UPMC Department of Pharmacy must be notified of all research protocols wherein the research involves the administration of an investigational new drug or an approved drug. The Investigational Drug Service can be reached at: (412) 647-5350. 2. When conducting a study that involves an investigational agent, the principal investigator should maintain an inventory log for the test article. This log should include information such as the: Protocol number or title Name of the principal investigator Drug/device name Drug dosage form, strength and schedule Shipping records including the date and quantity of receipt Initial and ongoing inventory balance Lot number Expiration date Identification of the study participant Quantity and date dispensed Initials of the individual preparing and dispensing the product Amount transferred or wasted Date(s) and quantity returned by the study participant Date(s) and quantity returned to the sponsor Name, address, and telephone number of the sponsor 3. There should be a signed physician’s order for every test article dispensed. 4. In addition, the investigator should ensure that periodic inventories of the test article are performed. These inventories should ensure that each test article can be accounted for and any discrepancies reconciled.