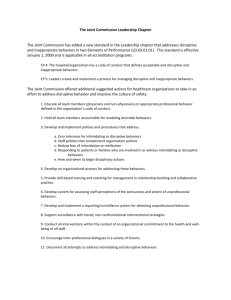
Behaviors that undermine a culture of safety have the potential to
advertisement

Impact of Behaviors that Undermine a Culture of Safety on Adverse Patient Events: An Evidence-Based Project By Susan Farley, Rhonda Garretson, Jennifer Singsank-Leffler Submitted in Partial Fulfillment of the Requirements for the Degree Master of Science in Nursing Nebraska Methodist College Department of Nursing Omaha, Nebraska Under the Supervision of Dr. Christopher J. Smallwood, PhD, RN July, 2015 BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 2 Table of Contents Title Page .........................................................................................................................................1 Table of Contents ............................................................................................................................2 Abstract ............................................................................................................................................5 Introduction .....................................................................................................................................6 Problem .......................................................................................................................................6 Purpose ........................................................................................................................................7 Background .................................................................................................................................8 Theory/Model .............................................................................................................................9 Significance ..............................................................................................................................10 Setting.......................................................................................................................................11 Stakeholders .............................................................................................................................12 Cost Benefits ............................................................................................................................12 Desired Outcome ......................................................................................................................13 PICO(T) Question ....................................................................................................................13 Search Plan Method .......................................................................................................................14 Search Plan Discussion ............................................................................................................14 Statement of Special Sources/Journals .....................................................................................14 PICO(T) Terms .........................................................................................................................15 Database Search Strategy .........................................................................................................15 Inclusion/Exclusion Criteria .....................................................................................................16 Analyzing the Literature ................................................................................................................17 BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 3 Literature Introduction ............................................................................................................17 Levels of Hierarchy of Evidence .............................................................................................17 Critical Appraisals ...................................................................................................................18 Article one: Laschinger (2014) ...........................................................................................18 Article two: Flynn, Liang, Dickson, Xie, and Suh (2012) ................................................19 Article three: Chipps, Stelmaschuk, Albert, Bernhard, and Holloman (2013)...................20 Article four: Walrath, Dang, and Nyberg (2010) ...............................................................22 Article five: Walrath, Dang, and Nyberg (2013) ..............................................................24 Article six: Roche, Diers, Duffield, & Catling-Paull (2010) .............................................26 Article seven: Wilson and Phelps (2013) ..........................................................................27 Synthesis Discussion of Evidence .................................................................................................29 New Understandings Generated by Evidence .........................................................................30 Limitations ..............................................................................................................................33 Implications/Impact of Evidence ............................................................................................34 Future Recommendations about Nursing Research ................................................................36 Future Recommendations about Nursing Education ...............................................................37 Future Recommendations about Nursing Administration .......................................................38 Future Recommendations about Nursing Practice ..................................................................39 Conclusion .....................................................................................................................................40 Reference List ................................................................................................................................42 BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 4 Appendix A ....................................................................................................................................47 Search Flow Diagram Appendix B ....................................................................................................................................49 Critical Appraisals Appendix C ....................................................................................................................................80 Matrix BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 5 Abstract The purpose of this evidence-based project was to understand the impact of clinician behaviors on patient safety events. The PICO(T) question represented is “Among hospitalized patients in acute care settings, how do behaviors that undermine a culture of safety affect the occurrence of adverse patient safety events?” Through a literature search using the Cumulative Index to Nursing and Allied Health Literature and PubMed databases, a hand search, and identified PICO(T) question terms, seven relevant articles were found. The literature analysis demonstrates increasing evidence supporting an association between behaviors that undermine a culture of safety and adverse patient safety events, presenting significant implications for the well-being of patients, staff, and healthcare organizations. More research is needed regarding the complexity of care, and all aspects of the clinician behavior construct. Recommendations for future nursing research include study of the practice environment and causation of behaviors that undermine a culture of safety. Future recommendations for nursing education include behavior recognition, conflict resolution, assertiveness training, and action steps when undermining behaviors occur. Recommendations for future nursing administration include establishing a positive practice environment, role modeling desired behavior, and empowering employees in establishing and maintaining an optimal safety culture. Future recommendations for nursing practice include advocating for staff education, behavior standards and accountability, as well as establishing a personal commitment of responsibility to foster a healthy practice environment. Understanding and addressing behaviors undermining a culture of safety must be a priority in order for healthcare organizations to achieve the high-reliability outcomes seen in other industries. BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 6 Impact of Behaviors that Undermine a Culture of Safety on Adverse Patient Events: An Evidence-Based Project There are varying terms characterizing behaviors that undermine a culture of safety in the workplace but research on what can be learned from those behaviors, including their consequences, needs continual exploring. If behaviors that undermine a culture of safety take place between healthcare team members, a breakdown in workflow can take place along with undesired patient outcomes. With the constant change dynamic in healthcare and the demand for increasing transparency among its organizations, it is vital to research how these undermining behaviors impact patient safety and then use that knowledge to develop strategies to effectively address them. Problem Behaviors that undermine a culture of safety are broad in scope, characterized by such terms as bullying, incivility, hostility, disruptive behaviors, and lateral/horizontal violence. A 2010 study demonstrated that 24 percent of registered nurses (RNs) reported experiencing a hostile workplace and 56 percent reported experiencing verbal abuse during the last year in which they worked (Buerhaus et al., 2012). These findings are relevant since a hostile workplace can interfere with a positive patient safety culture. Laschinger (2014) shared study outcomes linking negative patient safety cultures to increased work-related injuries, high medication error rates, and reluctance to report errors, and Squires’ findings that supportive professional practice environments are key to maintaining a patient safety climate. Laschinger (2014) discusses a definition of bullying as a repeated and prolonged exposure to psychological mistreatment directed as a specific target, and a definition of incivility as referring to low-intensity rude or disrespectful behaviors. The American Medical Association BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 7 describes disruptive behavior as verbal or physical personal conduct that potentially or actually negatively affects patient care, including but not limited to conduct which prohibits the ability to work with healthcare team members (Walrath, Dang, & Nyberg, 2010). The World Health Organization‘s definition of violence includes actual or threatened intentional use of power against others with a high likelihood of harm (Roche, Diers, Duffield, & Catling-Paull, 2010). Stanley, Martin, Nemeth, Michel, and Welton describe lateral or horizontal violence as any unwanted abuse or hostility within the workplace; Jackson, Firtko, and Edenborough characterize lateral/horizontal violence as a series of undermining incidents over time as opposed to an isolated conflict incident (Becher & Visovsky, 2012). Failure to address destructive clinician behaviors causes toxicity in the care environment to grow. Despite what is espoused as company core values, employees take their cues from those around them and adjust their behavior to fit in to the work environment; nothing is more destructive than the failure of leaders to manage these behaviors in their organizations (Porter O’Grady & Malloch, 2011). System stressors fueling the propensity for disruptive behavior include pressures to maintain patient throughput, a complex work environment, clinicians’ personality characteristics, role differences, and team member turnover (Walrath, Dang, & Nyberg, 2013). Regardless of etiology, these behaviors put patient safety at risk by negatively impacting the caregivers that patients entrust with their care. Purpose While there has been significant examination of a negative workplace on nurse outcomes, it is important to understand the impact of clinician behaviors that undermine a culture of safety on patient outcomes. The aim of this study is to complete a review of the literature to more fully determine the effects of clinician behaviors that undermine a culture of safety on the occurrence BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 8 of adverse patient safety events. This exploration will assist health organizations in setting priorities for enhancing interventions to improve patient safety. Background The climate of the care environment and its’ impact on patient safety has been an increasing area of focus for influential organizations in healthcare. Recognizing the negative impact that disruptive behaviors have on patient safety, the Joint Commission (TJC) published a Sentinel Event Alert in 2008 addressing this issue. TJC (2008) states “Intimidating disruptive behaviors can foster medical errors, contribute to poor patient satisfaction and to preventable adverse outcomes, increase the cost of care, and cause qualified clinicians, administrators and managers to seek new positions in more professional environments” (p. 1). TJC regulatory standards were subsequently amended to require organizations to have a code of conduct which defines destructive behaviors along with a process in place for managing them (Walrath, Dang, & Nyberg, 2010). Interestingly, disruptive behavior is a term commonly used in the literature and previously adopted by the Joint Commission (TJC) in their accreditation materials. However, because some health practitioners had a negative view of this terminology and it was considered ambiguous for some audiences, TJC replaced this term with behaviors that undermine a culture of safety, effective July 01, 2012 (TJC, 2012). Because this change confounds scholarly review, behaviors that undermine a culture of safety will encompass multiple terms for purposes of this study, including disruptive behavior, bullying, incivility, and lateral/horizontal violence. Previous studies have addressed behaviors resulting in abusive work environments. In a 1997 qualitative study, Farrell found that lateral violence was more stressful for nurses than physical assault from patients (Roche, Diers, Duffield, & Catling-Paull., 2010). In a 2005 study, BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 9 Rowe and Sherlock concluded that verbal bullying results in job stress, job dissatisfaction, missed work, and possibly decreased quality of care (Roche et al., 2010). Prior to embarking on their survey study conducted January 2004 through March 2007, Rosenstein and O’Daniel (2008) could find no documented studies directly linking disruptive behavior to negative clinical outcomes. Findings of their study revealed that 67 percent of the respondents agreed that disruptive behaviors were linked to adverse events – the result for medical errors was 71 percent and the result for patient mortality was 27 percent (Rosenstein & O’Daniel, 2008). The World Health Organization (WHO) recently identified workplace bullying as a serious public health threat (Laschinger, 2014). Theory/Model Description Understanding the different influences from theories of social learning and oppression is essential in understanding why behaviors that undermine a culture of safety occur in the workplace. In trying to explain the influences of theories on these negative behaviors, the Social Learning Theory and the Nursing Oppression Theory will be discussed. While the Social Learning Theory involves mimicking of negative behaviors, the Nursing Oppression Theory involves displaced anger. First, the Social Learning Theory can explain why coworkers imitate negative behaviors seen in the workplace. Walrafen, Brewer, and Mulvenon (2012) state that “Based on Bandura's theory, the workplace (world) and the employees (individuals) on some level cause each other's behavior (reciprocal determinism)” (p. 3). Some employees will see negative behavior happening in the workplace and choose to go along with it to try to fit in and be accepted by others. BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 10 Secondly, the Nursing Oppression Theory can help explain why there is hostility in healthcare among nurses and why behaviors that undermine a culture of safety exist. “Freire theorized that oppressed people internalize their situation by adopting the dominant group’s beliefs and values while minimizing their own” (Purpora & Blegen, 2012, para. 10). This theory helps explain why nurses feel less important and powerless in unhealthy work environments and can displace their hostility and anger towards others. Significance Focus on safety and quality is at the forefront in healthcare, now more than ever before. Once monitored internally only, health outcomes are increasingly in the public view and are now tied to service reimbursement. Hospitals in particular are under increasing pressure to improve care while reducing costs (Hines & Yu, 2009). Health Grades estimates that medical errors cause approximately 195,000 deaths annually in the United States (Hines & Yu, 2009). If the airline industry harmed as many people as healthcare, an angry outcry for reform from American citizens would take place throughout the country (Kerfoot, 2009). To frame it another way, “a checked bag on an airline flight is exponentially safer than a patient in an American hospital” (Nance, 2008, p. iii). There is a significant financial cost to patient harm. James found that medical errors in the United States are the third leading cost of death in hospitals, costing an estimated $17-$30 billion per year (Sahay, Hutchinson, & East, 2015). If a transformed healthcare system means high quality, cost efficient care for American citizens into the future, healthcare performance must move toward the transparency and high reliability of the airline industry; in order to do that, the barriers which are currently in the way of that objective must be understood. BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 11 Much effort has been focused on preventing hospital acquired conditions since the Centers for Medicare and Medicaid Services (CMS) changed their regulations in 2008 eliminating additional payment for these conditions, with additional provisions related to the Affordable Care Act only escalating the pay for performance climate. A 2010 study of registered nurses (RNs) and their perceptions of the healthcare environment found that 79 percent of respondents reported an increase in the number of performance improvement initiatives targeting hospital acquired conditions since the new CMS regulations were enacted (Buerhaus et al., 2012). However, part of the safety equation less explored is the environment of care in which caregivers practice and whether it is one that inhibits or promotes patient safety. The issue of behaviors that undermine a culture of safety and the impact on adverse patient safety events are in alignment with the Quality and Safety Education in Nursing (QSEN) competency of Safety and must be explored to better understand their influence on healthcare’s most critical component - patient outcomes. Setting Behaviors that undermine a culture of safety have the potential to take place in any setting where members of a healthcare team are working in collaboration to care for patients. Behaviors interfering with a culture of safety persist when there is tolerance and indifference, unwillingness to address it, and lack of awareness of the prevalence and impact on all aspects of the healthcare team including patients (Walrath, Dang, & Nyberg, 2013). These places include acute care settings, outpatient settings, and long term care facilities. For the purpose of this study, the focus will be on the acute care setting. According to the Department of Health and Human Services, 26% of hospitalized Medicare beneficiaries experienced an adverse event BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 12 during their hospital stay; forty-four percent of these were found to be preventable on physician review (Levinson, 2010). Stakeholders Patients are the main stakeholders in this discussion, as they are seeking care and it is their wellbeing that is affected by the outcome of negative behaviors. The second main stakeholders are the providers of care; nurses, physicians, and ancillary staff. Adverse patient outcomes have the potential to impact the professional and psychological well-being of the care giver through potential employment or licensure ramifications, feelings of remorse, and potential litigation. Hostile work environments, which include behaviors that undermine a culture of safety, may cause decreased employee retention as nurse’s satisfaction decreases and they seek employment elsewhere. Newly graduated nurses may be increasingly vulnerable and more predisposed to making medication errors as they lack familiarity with the work environment (Sahay, Hutchinson, & East, 2015). Other stakeholders include the families of the patients experiencing adverse patient safety events, the healthcare institution, and the agencies reimbursing the healthcare institution for the services provided. There have been many changes in reimbursement since 2008 when the Centers for Medicare and Medicaid started changing reimbursements for preventable adverse events. The changes mean that “Hospitals would be prohibited from billing Medicare for “serious, preventable adverse events” (Sohn, 2011, para. 5). Cost Benefits Adverse patient outcomes are costly for institutions. The amount paid out by Medicare only covers one-third of the cost incurred from treating these patients, leaving a large deficit that must be covered by the healthcare institution (Zhan, Friedman, Mosso, & Provost, 2006). This BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 13 lapse in funding has brought patient safety to the forefront and made it a renewed priority for administration as well as staff. The Centers for Medicare & Medicaid Services (2008) continue to monitor “never events” (errors that take place in healthcare that are costly and serious) and make determinations on what services and conditions they will and/or will not reimburse for. Desired Outcome The desired outcome of this literary review is to better understand the impact of behaviors that undermine a culture of safety among clinicians and the occurrence of adverse patient safety events. An adverse patient safety event is defined by the American Academy of Orthopaedic Surgeons as, “one that causes injury to a patient as the result of a medical intervention rather than the underlying medical condition. It represents unintentional harm to the patient” (Attarian, 2008, para. 3). In keeping with TJC and changes in terminology behaviors that undermine a culture of safety is an overarching term that includes lateral violence, disruptive behaviors, bullying, and incivility. Adverse patient outcomes would include hospital acquired infections, medication errors, patient falls, and wrong site surgeries. The results of this review will provide an analysis of how behaviors that undermine a culture of safety adversely affect patient outcomes. This study will allow healthcare organizations enhanced insight into the need for policies that support a healthy workplace and provide assistance with identification of strategies to achieve respectful, productive work environments. Such efforts will facilitate collaborative healthcare teams promoting the best possible outcomes for every patient, every time. PICO(T) Question The cost of medical errors in the United States in 2008 was 19.5 billion dollars and costs are continuing to rise. There was an estimated 200,000 people that died from preventable BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 14 medical errors (Andel, Davidow, Hollander, & Moreno, 2012). The key question to ask now is: Among hospitalized patients in acute care settings, how do behaviors that undermine a culture of safety compared to the absence of those behaviors, affect the occurrence of adverse patient safety events? This question follows the PICO(T) format outlined in Melnyk and Fineout-Overholt (2011) that will lead to the most relevant and evidenced based research. Search Plan Method Search Plan Discussion Healthcare is rapidly changing and outcomes from the most current research are required to promote evidence-based care. “Frequently updated bibliographic and/or full text databases that hold the latest studies reported in journals are the best, most current choices for finding relevant evidence to answer compelling clinical questions” (Melnyk & Fineout-Overholt, 2011, p. 42). The Cumulative Index of Nursing & Allied Health Literature (CINAHL Plus) and PubMed were the chosen databases to use in this search as both are expansive in scope. A computer search was conducted based on PICO(T) terms using Boolean operator methodology. This search presented a particular challenge in that both the intervention and the outcome focuses of the study are captured in a broad array of phrases throughout the literature, requiring a particularly extensive search of various terms and combinations. However, Raines (2013) informs us that the goal of a literature search is to identify evidence to support practice regardless of the obstacles that obtaining such evidence presents. In addition to the databases, a computer search of Google Scholar was also conducted, along with manual searches to try and maximize results. The importance of the search method should not be underestimated. Knowledge of how to effectively access the literature helps to BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 15 close the divide between evidence from research, and practice based on tradition in the clinical setting (Raines, 2013). PICO(T) Terms Table 1. PICO(T) Terms PICO(T) Terms P (population) Hospitalized patients I (intervention) Lateral/horizontal violence, workplace violence, incivility, hostility, disruptive behavior, clinician disruptive behavior Disruptive behavior prevention C (comparison) O (outcome) T (time) Patient safety, patient outcomes, medication errors, patient falls, wrong site surgery No terms used Database Search Strategy The search was begun in CINAHL Plus with the population term “hospitalized patients”; when combined with each intervention term using the Boolean operator and, the yield was zero articles but when combined with the Boolean operator or, 1270 articles were identified. Next, “hospitalized patients” and “disruptive behavior prevention” resulted in zero articles while “hospitalized patients” or “disruptive behavior prevention” yielded 785 articles. Finally, “hospitalized patients” and all outcome terms resulted in zero articles while “hospitalized patients” or all outcome terms yielded 2623 articles. To better narrow the literature field, various intervention terms were combined with various outcome terms. Intervention term “workplace violence” and the outcome term “patient safety” resulted in eight articles that were then manually reviewed for relevance based on inclusion criteria; of the eight, three pertained to the PICO(T) question under study. In searching BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 16 PubMed, “workplace violence” and “patient outcomes” yielded 20 articles and a manual review of those resulted in obtaining one article. “Disruptive clinician behavior” and “patient outcomes” resulted in zero articles but “disruptive clinician behavior” alone resulted in 68 articles and a manual review of those yielded two articles. The terms “incivility” and “patient outcomes” resulted in four articles of which one pertained. To be reasonably certain valuable research was not missed, a hand search was conducted of three journals for articles pertaining to a culture of safety and adverse patient outcomes; journals included were the Journal of Nursing Scholarship, JONA’s Healthcare Law, Ethics, and Regulation, and the Journal of Advanced Nursing. Six articles were found from this hand search but four were disregarded because they did not meet the inclusion criteria. This left two articles but these had already been identified through the other search activities. A Google Scholar web search was conducted using the various terms specified, however, the resulting articles focused on nurse outcomes, such as retention and satisfaction, not patient outcomes, so no useful material was found. In addition to the core studies ultimately identified, multiple supportive articles were found during the search process that increases depth of knowledge in related areas. A flow diagram of the search plan can be found in Appendix A. Inclusion/Exclusion Criteria Establishing inclusion and exclusion criteria to evaluate studies focuses a search to promote the most relevant evidence (Melnyk & Fineout-Overholt, 2011). Full text availability was a component of the inclusion criteria. Full copies of studies are highly recommended as this allows repeated review for important details (Polit & Beck, 2012). In addition to full text availability, the other inclusion criteria used in evaluating articles for this study were English language, peer reviewed research, and publication within the last five years. Foreign language BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 17 articles and articles published earlier than 2009 were excluded from consideration. Focusing a search is critical to facilitating the most valuable evidence-based project outcomes. Also important is being consistently mindful of the connection of search efforts to the patient. Raines (2013) suggests that “knowing how to find evidence to support nursing practice behavior and interventions is a professional responsibility and enhances patient outcomes” (p. 205). Analyzing the Literature An extensive search resulted in eight articles selected for this study. After conducting critical appraisals of each article, one was discarded for content weakness in relation to the study PICO(T) question. The seven articles remaining were carefully examined to determine trustworthiness (qualitative research) and validity/reliability (quantitative research). A matrix table was created to organize the article appraisal data. Headings were used for the matrix table as applicable to qualitative or quantitative research articles and include: article citation and level of evidence, purpose and conceptual framework, method of data collection and analysis, measurement tools, sample and size, results, and summary comments. The matrix table can be found in Appendix C. Levels of Hierarchy of Evidence The concepts and hierarchy of evidence described in Polit and Beck (2012) were used to evaluate the types and strength of the evidence presented in each article. The hierarchy described in Polit and Beck (2012) is designed as a seven-level pyramid with the highest point – Level I encompassing the strongest possible evidence which is systematic reviews of randomized control trials (RCTs), followed by systematic reviews of nonrandomized trials. Level II includes single RCTs and single nonrandomized trials, followed below by Level III containing systematic reviews of correlational/observational studies. Level IV involves single correlational/observational studies and Level V contains systematic review of BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 18 descriptive/qualitative/physiologic studies. Nearing the base of the pyramid is Level VI, composed of single descriptive/qualitative/physiologic studies and at the bottom is Level VII evidence which is the opinion of authorities and expert committees. Overall, systematic reviews of multiple studies are stronger than single studies within the same category. Of the seven articles appraised for this study, two were Level VI evidence and five were level IV. One caveat which Polit and Beck (2012) emphasize is that this hierarchy cannot be universally applied for ranking evidence validity and is most appropriate for research questions about the effects of clinical interventions. Polit and Beck (2012) note that the hierarchy would not be relevant for questions related to the patient experience, however, that does not mean this area is less important for nursing practice. Whether investigating efficacy, safety, and cost effectiveness of nursing interventions; determinants of well-being; the nature of patient experiences; or the quality of nursing assessment measures, the emphasis for determining best evidence should be on findings that are methodologically appropriate, rigorous, and relevant for the pressing clinical questions at hand (Polit & Beck, 2012). The focus of this study involves the complexity of the lived clinician experience with behaviors that undermine a culture of safety and how that potentially impacts patient outcomes, representing a newer focus for research efforts. Critical Appraisals Laschinger (2014) conducted a single observational study that investigated “the impact of subtle forms of workplace mistreatment (bullying and incivility) on Canadian nurses’ perceptions of patient safety risk and, ultimately, nurse-assessed quality and prevalence of adverse events” (p. 285). The goal of Laschinger’s research was to see what effect workplace bullying and incivility had on the perception of patient safety and adverse events. Laschinger BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 19 used five different measurement tools in this study consisting of the Negative Acts Questionnaire Revised (NAQ-R), the Cortina’s Workplace Incivility Scale, a 5-point Likert scale, a Sochalski 0-4 scale, and the Aiken et al 1-4 rating scale. The results of the study showed that bullying and all sources of incivility were significantly related to nurse-assessed quality of care, adverse events, and perceptions of patient safety risk. Patient/family complaints were the individual adverse event most strongly related to bullying and physician and coworker incivility. The study also revealed that subtle forms of workplace mistreatments can have detrimental effects on patient safety outcomes. While there are limitations to the study including use of cross-sectional data, low questionnaire response rate, using a targeted sample, and patient outcomes being nurse-assessed, study methods demonstrated sufficient rigor that the findings can be considered valid and reliable. Flynn, Liang, Dickson, Xie, and Suh (2012) conducted a single observational study examining “the relationships among characteristics of the nursing practice environment, nurse staffing levels, nurses’ error interception practices, and rate of nonintercepted medication errors in acute care hospitals” (p. 180). The goal of the Flynn et al. research was to examine whether or not the environment that nurses work in contributes to the rate of nonintercepted medication errors. The measurement tools used in this study were the Practice Environment Scale of the Nursing Work Index (PES-NWI) and a four item scale on interception practices. The study sample included 14 American acute care hospitals of various sizes in New Jersey, all designated as teaching hospitals. Survey data was totaled to the unit level which was then linked with unit level staffing and error data in order to understand the relationships among study variable. Sample size included 82 medical-surgical units; critical care units and step-down units were excluded. BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 20 The results of the study demonstrated that a supportive practice environment prevents medication errors. All subscales of the PES-NWI except for Staffing and Resource Adequacy were positively associated with error interception practices. The subscales of Collegial NursePhysician Relationships and Foundations for Quality care were most strongly associated with nurses’ interception practices. As the authors note, this study highlights that nurses in a supportive environment demonstrate higher quality nursing practices. These practices include interception behaviors which are associated with fewer adverse patient events. The most significant limitation with this study is the use of incident reports for data collection in relation to the well documented underreporting of medication errors or near misses. A mean error rate below the national average appears to validate this concern; direct observation or chart reviews are considered more reliable for studying medication errors and should be considered for future studies. Another limitation concerns the tools used for measuring interception practices in this study; although developed through extensive qualitative interviews, further evaluation of reliability is needed. Despite stated limitations, the validity and reliability of the study findings can be considered reasonably sound and lend support to the PICO(T) question from the standpoint that supportive nurse practice environments are associated with less adverse patient safety events. The descriptive study by Chipps, Stelmaschuk, Albert, Bernhard, and Holloman (2013) examined “whether the demographic variables of gender, ethnicity, hospital, years of experience on the unit, years in the profession, and job title predict the experience of workplace bullying; whether a relationship exists between workplace bullying and emotional exhaustion; and whether bullying is associated with perceptions of patient safety in the OR” (p. 479). The goal of the Chipps et al. study was to determine what effect bullying had in the operating room (OR). There BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 21 were three measurement tools used in this study including the Negative Acts QuestionnaireRevised (NAQ-R), a nine item Emotional Exhaustion Subscale of the Maslach Burnout Inventory (MBI) seven point Likert scale, and 23 additional questions. This study used a cross-sectional survey design and a convenience sample of 167 participants including: RN’s, surgical technologists, and unlicensed perioperative personnel working in the ORs. The participants were from two different academic medical centers that were both Magnet designated. Using stated tools, the study measured workplace bullying, emotional exhaustion, and the perception of job stress related to bullying experiences or the witnessing on bullying. Data was analyzed using the SPSS Statistics computer software program along with inferential statistics including: correlational analysis, multiple regressions, and logistic regression analysis. The results of the study demonstrated that 59% of study participants reported witnessing coworker bullying weekly and 34% reported identifying at least two bullying acts weekly. The most common act of bullying is identified as having one’s opinion ignored with 28% of respondents reporting experiencing being ignored. Study results also show that while differences in the experience of bullying is reported among varying hospitals and ethnicities, there is a moderate, positive correlation between bullying and emotional exhaustion. Interestingly, only 6% of respondents indicated a perception that patient safety was compromised due to experiencing negative acts, which is contrary to a variety of previous studies. While nearly twothirds of participants reported witnessing coworkers being bullied, less than one-tenth of respondents identified themselves as being bullied. The authors note that the disparity between observed and experienced bullying in relation to a low perception of patient safety compromise BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 22 may be explained by bullying not being viewed as problematic, or by the result of a survey limitation in question wording, using the term negative acts instead of bullying. Other study limitations include survey length, voluntary participation, and a low response rate, rising into question possible selection bias and representativeness of the results. The authors note the possibility that those who have experienced bullying may have a greater desire to participate or, alternatively, perpetrators may shun participation. In addition, the third tool used questions developed by the authors. Although questions developed were peer-reviewed for clarity, the questions may not have been completely effective in obtaining the information that the authors were seeking. Despite the limitations, reasonable validity and reliability can be inferred. While the research relates to the focus of the PICO(T) question, the results do not support a relationship between bullying and adverse patient safety events, however, a correlation between bullying and emotional exhaustion was established. It is reasonable to think that this and other consequences of bullying may impact quality nurse behaviors, ultimately affecting patient safety, but further study is required. The authors recommend additional research to fully understand the phenomenon of bullying and related consequences. The single qualitative study of Walrath, Dang, and Nyberg (2010) examined the experiences of hospital RNs related to disruptive behavior. The purpose of the study was to gain understanding of how RNs describe disruptive clinician behavior and its perceived impact, based on their observed and actual experiences. Focus group sessions involving 96 RNs from a variety of practice settings within an acute care hospital were the mechanism for obtaining the data. Findings revealed the occurrence of disruptive behavior in all practice settings, involving a variety of healthcare personnel; 225 disruptive behavior events were coded and 168 different BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 23 disruptive behaviors were identified and synthesized into 21 categories. Three themes emerged among these categories: incivility, psychological aggression, and violence. Physicians were identified as instigators in 42% of events, nurses in 29% of events, support personnel in 27% of events, and management in two percent of events. Triggers for disruptive behavior and RN responses to disruptive behavior were also explored and the conceptual model Johns Hopkins Model for Disruptive Clinician Behavior was presented. The findings of Walrath et al. (2010) confirmed that disruptive behavior affects the RN, the practice setting, and most importantly for the PICO(T) question being explored – the patient. RN participants described emotional distress and distraction from patient care, and priority conflicts between patient care and operational needs. Concerns regarding a decrease in quality care, increased risk to patient safety, care delivery delays, and disrupted working relationships were also described. There are limitations to this study that restrict the dependability and transferability of learnings, such as convenience sampling with low response rate resulting in participants not representative of the population of RNs employed at the organization and inclusion of only a single study site. However, the credentials of the researchers are indicative of adherence to scholarly research methods; rigor in conducting the study was demonstrated and the study can be considered trustworthy. Despite the study limitations, the experiences described by RN participants provide insight into the disruptive behavior construct and provides direction for future inquiry of this phenomenon in the acute care setting. This 2010 study by Walrath et al. supports the PICO(T) question under examination, pointing to an emerging link between behaviors that undermine a culture of safety - described in their study as disruptive clinician behavior - and adverse patient safety events in acute care settings. The authors recommend increasing awareness and BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 24 establishing environments that recognize, acknowledge, and openly discuss disruptive behavior in order to achieve a climate of civility as an important component of a culture of safety. In follow-up work to their previous study, the purpose of the single correlational study by Walrath, Dang, and Nyberg (2013) was to understand the complexities of disruptive behavior in a large academic medical center in order to (a) determine type, frequency, scope, and impact of clinicians’ personal experience with disruptive behavior; (b) compare the disruptive behavior experiences of RNs and medical doctors (MDs); and (c) customize interventions for RNs, MDs, interprofessional teams and the organization to improve the culture of patient safety. A survey instrument entitled Disruptive Clinician Behavior Survey for Hospital Settings was developed and appropriately validated to capture the data sought. A study population of 5,710 was targeted that included three clinician groups made up of (a) RNs; (b) MDs; and (c) affiliates including nurse practitioners, nurse midwives, and physician assistants. Ultimately, there were 1,559 study participants. Study findings demonstrated that 84% of respondents reported personally experiencing disruptive behavior during the past year, with 26.4% reporting it was daily or weekly, 29.4% reporting it was monthly, and 67% reporting that the behavior had been going on for a year or more. In addition, 73% of respondents reported observing a coworker who was a target of this behavior. RNs experienced a significantly higher frequency of disruptive behavior than MDs. Disruptive behavior was reported more frequently within the MD staff and the affiliates reported MDs as having the most negative impact. Of particular relevance to the PICO(T) question being explored, there were 189 events of patient harm reported by participants related to disruptive behavior, lending further emphasis that behaviors that undermine a culture of safety are associated with adverse patient safety events in acute care settings. But interestingly, study BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 25 findings also indicate that MDs and RNs speak up when observing behavior that negatively impacts patients and do not let the person exhibiting disruptive behavior present a barrier to patient care and the reporting of patient deterioration which is in contrast to previous research findings. Study findings also identified that disruptive behaviors have triggering events, such as intrapersonal, interpersonal, or organizational in nature; participants specified organizational triggers such as high census, volume, patient flow, environmental overload, and unresolved system issues as the most frequently occurring, lending insight into where to target prevention strategies. There are some limitations to this 2013 study by Walrath et al. which constrain the learning regarding the complexities of disruptive behavior under examination. Due to assessment following the study that connotations of the term disruptive behavior may predispose how respondents answered, the survey instrument was retitled to a more neutral phrasing: Survey of Unprofessional Behaviors: Triggers, Responses, Impacts. Related to the findings that indicate clinicians speak up and do not let disruptive behavior get in the way of patient care, the authors acknowledge that the sensitivity of this survey item may have predisposed participants to sacrifice accuracy of their responses in favor of one that would be perceived as more socially acceptable. Lastly, a low response rate (possibly due to survey length and/or fear of being identified), lack of data on non-responders, and the potential that responders were victims of disruptive behaviors raise into question possible selection bias and representativeness of the results. The authors have since shortened the survey instrument and decreased specificity of demographic items in hopes to increase participation in future studies. However, based on the credentials of the researchers as previously discussed and the rigor of survey instrument development and methods, reasonable validity and reliability can be inferred. The authors note BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 26 that a culture of trust, mutual respect, and collegiality are the hallmarks of a culture of safety and recommend organizational assessments to guide action planning to improve this important aspect of the environment of care. With an aim to relate nurses’ perceptions of violence on medical-surgical units (including emotional abuse, threat, or actual violence) to the nurse practice environment and patient outcomes, the single correlational observational study by Roche, Diers, Duffield, and CatlingPaull (2010) is a secondary analysis of data collected in two previous studies. A cross-sectional collection of data was obtained by surveys, along with primary data collected for one week on 94 medical-surgical nursing units in 21 hospitals in two states of Australia. The Nursing Work Index-Revised (NWI-R), the environmental Complexity Scale (ECS), the PRN-80 measure of patient acuity, and survey questions on workplace violence were combined with primary data regarding staffing, skill mix, and patient outcomes – specifically, falls and medication errors. There were 2,487 participants, representing an 80.3% response rate. Study findings indicated that while patients and families were the sources of most of the perceived violence and emotional abuse, up to a fifth was reported to be from co-workers. Findings related to patient outcomes revealed a positive association between physical violence and falls, medication errors, and late administration of medication. In addition, threats of violence were linked to both falls and medication errors. Although caution is warranted in assimilating these associations due to the low rates for adverse events, the authors note some correlations were supported by Poisson regression analyses specific to outcome measures with low rates. In addition to the low adverse outcome rates limiting statistical power, the study was also limited by self-reporting and a seven day data collection period which may have caused some omissions in capturing adverse events. However, the credentials of the researchers are BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 27 indicative of adherence to scholarly research methods and the study was conducted with sufficient rigor to consider it valid and reliable. The study by Roche et al. pertains to the PICOT question being examined through relating perceptions of violence in the acute care setting to the nurse practice environment and patient outcomes. Violence is repeatedly an element for nurses to deal with in the environment of care. The authors note that study outcomes point to perceptions of violence as more associated with qualities of the work environment than with patient populations. The authors share that “perceptions of violence were related to adverse patient outcomes through unstable or negative qualities of the working environment” (Roche et al., 2010, p. 13). This study points toward actionable items in the care environment that hospitals can address to improve a culture of safety. The authors urge the importance of understanding the complexity of the care environment and the relationship of violence to patient outcomes so meaningful change can be implemented. In their single observational study, Wilson and Phelps (2013) explored horizontal hostility (HH) in an acute care hospital. Relevant to the PICO(T) question under examination, the aim of the study was to determine the perceived level of HH among nurses in one 220 bed community hospital and, if present, determine the extent that HH behaviors (RN to RN or MD to RN) directly influence nurse behaviors related to patient care and safety. A 28 item survey instrument was developed, modeled after the American Association of Critical Care Nurses’ study entitled Seven Crucial Conversations in Healthcare and the survey by Stanley et al. entitled Lateral Violence Nursing Survey. The survey instrument was distributed by members of the hospital’s Nursing Research Council to all 500 RNs used by the hospital, excluding registry and traveling nurses, in a two month period. The response rate was 26% (n = 130) with 80 respondents reported to be direct patient care providers and 17 were unit-based charge nurses; 11 BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 28 were in indirect care roles and 22 chose not to identify their role. Once collected, completed surveys were reviewed and transcribed by the PhD-prepared nurse researcher who was not employed by the hospital or familiar with individual units or nurses. Descriptive statistics were used to summarize demographic characteristics and item responses but inferential statistical methods were not used because causation was not an intended focus of the study. When asked about frequency of witnessing a peer or physician demonstrating bullying behavior, results showed nearly 60% of respondents observed HH at least monthly, with a majority of those stating it was weekly, with “nurse from my unit” then “a physician” as the top two sources, followed by “a charge nurse”, and “a nurse from another department”. When asked who they spoke with about perceived HH, 58% of participants spoke with coworkers while only 17.3% addressed the source directly. The most common reason for failure to confront was lack of trust anything would change and that such a confrontation would only make their work situation worse. Although response to the survey item addressing nurse behaviors in reaction to HH was very limited, the authors were able to demonstrate a correlation between HH and practice behaviors that compromise patient safety. For example, greater than 30% of respondents indicated interpreting an unreadable physician order the best they could rather than calling to get clarification. Although author credentials and methods were commensurate with scholarly research, development of the survey instrument was not fully explored and surveys were reviewed and transcribed by a single (PhD-prepared) author. Major limitations were present in this study, severely limiting validity and reliability, one of the most significant being the number of nurses choosing not to answer several of the study variables which restricted the kinds of analyses possible. Many nurses did not want to identify their home unit and the authors raise the BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 29 possibility that asking participants for this information was a design flaw. Although this thwarted direct linkage of adverse events to levels of perceived hostility at the unit level, the authors urge that until this happens, the full scope of HH on patient safety will not be understood. Wilson and Phelps (2013) also hoped to examine nurse behaviors in response to HH in relation to adverse events in order to establish a connection between HH and poor patient outcomes but limited sample size in this survey section prevented the statistical power to do so. Because of the limitations discussed and the single setting for the study, generalizability of results is not possible. The overall low response rate raises into question selection bias, prompting concern that participants were not representative of the population of RNs employed at the organization and that participants were skewed toward those who had experience with HH and wanted to share their account. Despite the many challenges, study results do indicate a connection between HH and patient safety threats, and illuminate the need for further research in this area. Synthesis Discussion of Evidence With an escalating climate of pay for performance, patient outcomes are an increasing area of hospital concern and focus. When the Centers for Medicare and Medicaid Services (CMS) began to cease payment for treating preventable hospital-acquired conditions such as pressure ulcers, urinary tract infections, and blood stream infections; nurses received increased education and training opportunities but also an increase in their workload without added supports such as staffing or compensation (Buerhaus et al., 2012). The stressors on clinicians to produce positive outcomes and prevent harm are great, particularly challenging given their complex and dynamic work environment. While much has been done to improve clinical practice to prevent hospital-acquired conditions, behaviors that undermine a culture of safety and their BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 30 influence on adverse patient events represents a newer area of exploration and one that must be understood if hospitals are to become high-reliability organizations in their provision of healthcare services. New Understandings Generated by the Evidence While direct correlation of behaviors undermining a culture of safety and adverse patient safety events are only beginning to emerge, this systematic review of the most recent research demonstrates a strengthening connection. Laschinger (2014) demonstrated that bullying and all sources of incivility were significantly related to nurse-assessed quality of care, adverse events, and perceptions of patient safety risk. Flynn et al. (2012) found that nurses in a supportive environment demonstrate higher quality nursing practices including the use of interception behaviors, and that a supportive practice environment helps to prevent medication errors. While Chipps et al. (2013) did not determine a correlation between bullying and adverse patient safety events, they did demonstrate a correlation between bullying and emotional exhaustion. It would be logical to take the findings of Chipps et al. and interpret them inversely of the findings of Flynn et al., hypothesizing that the emotional exhaustion related to bullying may compromise patient safety through lower quality nursing practices which, in fact, is supported by the findings of Walrath et al. (2010). In Walrath et al. (2010), an emerging link was demonstrated between adverse patient safety events and disruptive clinician behavior evidenced by RN respondent descriptions of emotional distress and distraction from patient care. Also in Walrath et al. (2010) were concerns regarding decreased care quality, increased risk to patient safety, and care delivery delays as a result of disruptive clinician behaviors. These findings were also consistent with Wilson and Phelps (2013) who were able to demonstrate a correlation between HH and behaviors that BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 31 compromise patient safety but were unable to demonstrate a link between nurse behaviors in response to HH and adverse safety events due to their limited sample size, representing a valuable area for future study. Representing one of the larger, more comprehensive research efforts in this review, findings in the follow-up study by Walrath et al. (2013) included 189 events of patient harm reported by study participants as related to disruptive clinician behavior, providing one of the few studies pointing to a direct association between the two variables. Roche et al. (2010) also demonstrated a more direct correlation between undermining safety behaviors and adverse safety events through a positive association between physical violence and falls, medication errors, and late administration of medication, as well as threats of violence linked with both falls and medication errors. While patients and families were found to be the main source of violence and threats in the study by Roche et al., it is important to note that up to one-fifth of the incidents reported were from coworkers. In addition, while the focus in organizations may tend to be on hostile patients and families as sources of clinician abuse in the practice environment, Roche et al. also found that perceptions of violence are actually more associated with qualities of the work environment than with patient populations. In addition to furthering insight into the effect of behaviors that undermine a culture of safety on patient outcomes, this systematic review also expanded knowledge regarding other aspects of the issue, including prevalence. Undermining safety behaviors were reported to occur within many practice settings and may be more frequent than might have previously been believed. Walrath et al. (2010) found disruptive behavior among all practice settings represented by study participants. Chipps et al. (2013) found 59% of study participants witnessed coworker bullying weekly and 34% reported identifying at least two bullying acts weekly. In Walrath et al. BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 32 (2013), 84% of respondents reported personally experiencing disruptive behavior in the past year, with 26.4% reporting it as daily or weekly, 29.4% reporting it was monthly, and 67% reporting it had been going on for a year or more. Findings by Wilson and Phelps (2013) demonstrated that 60% of respondents observed HH at least monthly. When envisioning the amount of clinicians in a single hospital alone, the number of clinicians potentially exposed to negative safety behaviors throughout the United States is stunning. Additional insight from this review supporting greater understanding of the phenomena is expanded awareness regarding types and sources of negative safety behaviors. Behaviors undermining a culture of safety are expressed in many forms and involve a variety of personnel. Walrath et al. (2010) identified 168 disruptive behavior types and synthesized the types into 21 categories; the three themes that emerged from these categories were incivility, psychological aggression, and violence. The instigators of the disruptive behavior included physicians (42%), nurses (29%), support personnel (27%), and management (2%). In Walrath et al. (2013), RNs experienced significantly higher frequency of disruptive behavior than MDs and such behavior was reported more frequently within the MD staff. Participants that reported witnessing bullying behavior in the study of Wilson and Phelps (2013) noted nurse within my unit, then physicians as the top two sources, followed by charge nurse and a nurse from another department. While it might be natural to focus on the more extreme circumstances, Laschinger (2014) highlighted the important distinction that even subtle forms of workplace mistreatments can have detrimental effects on patient safety outcomes. This is illustrated by the findings of Chipps et al. (2013) in which the most common act of bullying was identified as having one’s opinion ignored, with 28% of the respondents reporting experiencing being ignored. In settings where identification of risk requires team members at any BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 33 level to feel free to speak up and others to actively listen in order to prevent errors from reaching the patient, these findings are highly concerning and should cause healthcare organizations to take notice. Causation is only beginning to be examined but is important to identifying remedies and this systematic review provided new insights in this area, as well. Walrath et al. (2013) found that disruptive behavior has triggering events that are intrapersonal, interpersonal, or organizational in nature; study participants identified organizational triggers such as high census, volume, patient flow, environmental overload, and unresolved system issues as the most frequently occurring. Hospitals need to better understand how their workflow decisions in response to organizational pressures might have more subtle but substantial negative downstream consequences unless there are mitigating strategies to improve the practice environment and promote safety. The Social Learning Theory and the Nursing Oppression Theory can help inform understanding about why these behavioral responses occur and tools such as the Survey of Unprofessional Behaviors: Triggers, Responses, Impacts can assist organizations in assessing their individual settings in order to make meaningful action plans to improve their safety culture. Limitations This review study was impacted by the fact that the topic is a newer area of exploration and, as such, the volume of evidence that is currently available is limited. While most of the research reviewed strengthened the perception of an association between behaviors that undermine a culture of safety and adverse patient safety outcomes, only two of the studies were able to establish a direct correlation. The focus represents a particularly challenging area to conduct research for a variety of reasons, one of which is the sensitivity of the subject matter which may constrain the acquisition of willing study participants representative of the study BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 34 population, as well as confound the development of study designs that facilitate objective data collection. Those investigators who have already embarked on the journey should be appreciated and the learnings from these pioneers will influence subsequent research, eventually allowing a rich understanding of this important area to patient safety. Implications/Impact of the Evidence This review study underscores understanding that clinician behavior matters to patient safety. The primary implication of this study for hospitals and those who serve within them is the need to appreciate the effects of a hostile work environment on patient outcomes, and embrace a priority to assess and address those issues to promote a culture of safety. Hospitals are dynamic environments with differences in hierarchy and disciplinary structures among the various professions that make up the healthcare team; this complexity presents challenges in building a culture of patient safety (Manojlovich et al., 2014). An intervention plan may seem daunting but resources exist to aid in the effort. The Joint Commission provides a blueprint of recommendations that organizations can implement to address behaviors compromising a culture of patient safety, including the areas of recognition and awareness; cultural commitment/leadership/champions; policies and procedures; incident reporting; structure and process; initiating factors; education and training; communication tools; BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY discussion forums; and intervention strategies (Rosenstein & O’Daniel, 2008, p. 468-470). 35 Ensuring a healthy work environment to promote safety is the right thing to do for the primary stakeholder, the patient, but it is also the right thing to do for the well-being of those who are entrusted to provide care. However, other implications of this review study exist, as well, supporting the need to optimize patient safety through positive work cultures. There are financial ramifications in allowing behaviors undermining patient safety to persist. In supporting literature, Becher and Visovsky (2012) shared Gerardi and Connel’s estimates that horizontal violence is estimated to cost $30,000-$100,000 annually for each victim through absenteeism, treatment for depression and anxiety, decreased work performance, and increased turnover; they also shared Pendry’s replacement cost estimate of one specialty nurse possibly exceeding $145,000. Particularly critical with nursing as the largest profession involved in healthcare, nursing workforce attrition reduces the quality and quantity of care provided with significant implications for health outcomes (Huntington et al., 2011). The relationship between nursing and care quality needs to be appreciated, particularly now when recruitment and retention of talent is vital; hospitals and the United States overall cannot afford to be shortsighted in this regard. As a top occupation for job growth, the RN workforce is expected to grow 19% by 2022 to 3.24 million and the nursing shortage is expected to grow to 260,000 by 2025, representing a shortage twice as large since the mid-1960s (American Association of Colleges of Nursing [AACN], 2014). There seems to be a significant gap between knowledge of the practice environment, recommendations for change and change occurring, resulting in nurses intending to leave the profession (Huntington, et al., 2011). Hospitals must do all they can to retain and BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 36 recruit a robust nursing workforce, being ever mindful that, in addition to filling vacancies, these efforts have an important impact on patient well-being. This review study expanded knowledge of the practice environment and provided evidence that destructive clinician behavior affects many facets of care delivery, all of which can negatively impact patient safety. The call to do no harm is the guiding principle for all healthcare professionals and, yet, it continues to occur. In addition to related hardship experienced by the patient, another organizational consequence to lack of a safety culture is the burden of cost associated with patient harm. Previously, costs to Medicare for hospital acquired conditions was in the billions annually; CMS reported 29,536 vascular catheter-associated infections in 2007 resulting in an average cost of $103,027 per hospitalization totaling over $3 billion (Himes & Yu, 2009). With the Affordable Care Act and the current pay for performance climate, these costs are increasingly shifting to the provider; combined with costs related to legal actions associated with poor patient outcomes, there is increasing urgency for financial reasons alone to ensure high quality care. This review study helps to illuminate that, along with clinical strategies, a focus on clinician behaviors needs to be included in the repertoire of evidence-based action items important to care quality; the benefit can be expected to far outweigh the cost of not doing so. In alignment with other influential healthcare organizations, Safety and Teamwork and Collaboration are included as two of the Quality and Safety Education in Nursing (QSEN) competencies (AACN, 2012), lending emphasis that effort in this area should be a priority. Future Recommendations about Nursing Research The area of clinician behaviors undermining to a culture of patient safety represents rich ground for future study. Chipps et al. (2013) recommend additional research to better understand the phenomenon of bullying and related consequences. The issue actually encompasses many BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 37 behavior types including bullying, hostility, incivility, disruptive behavior, and lateral/horizontal violence and each once should be fully explored. Nurse practice behaviors, in response to negative clinician behaviors, is another area that needs to be thoroughly examined in order to confidently understand the impact on patient safety. Wilson and Phelps (2013) highlighted the need to connect adverse events to perceived hostility at the unit level in order to better establish a direct correlation to patient safety. The issues of behaviors that undermine a culture of safety in relation to adverse patient events cannot be studied in isolation since the lived experience of clinicians - their perceptions, reactions, and response behaviors - are complex, as are the organizations in which they work. As systems within the body can affect each other in profound ways for good or ill, patient safety is significantly impacted by the practice environment through those providing their care. In Roche et al. (2010), the authors encourage greater understanding regarding the complexity of the care environment and the relationship between clinician behaviors and patient outcomes so meaningful change can happen. This understanding should also be extended to include causation which is only beginning to be explored and is the key to hospitals establishing supportive systems and standards, in appreciation that healthier practice environments lead to safer patients. Future Recommendations about Nursing Education The findings of this study indicate that the opportunities for nursing education within the realm of this issue are broad. In relation to nurses speaking up in the face of hostility, findings were mixed. For example, while participants in Walrath et al. (2013) reported 189 events of patient harm related to disruptive behavior, findings also indicated that clinicians speak up in the face of disruptive behavior and do not let it interfere when patient safety is at risk (in contrast to earlier research). On the contrary, the findings of Wilson and Phelps (2013) indicated a lack of BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 38 confronting behaviors and demonstrated a correlation between HH and practice behaviors that compromise patient safety. Other findings such as those by Chipps et al. (2013), point to the possibility that bullying is not viewed as problematic. In supporting literature, Lachman (2014) discussed the Code of Ethics for Nurses as established by the American Nurses Association (ANA), noting that these standards clearly define intimidating behavior as unethical and outline a nurse’s responsibility not to engage in those behaviors and to act on circumstances to the contrary. Therefore, areas of staff education should include; behavior standard expectations, behavior recognition, conflict resolution, communication and assertiveness training, available organizational resources, actions to take when such behavior is encountered, how to document such behavior, and the overall connection to patient safety. Future Recommendations about Nursing Administration The recommendations for nursing administration based on this review study are significant. Hospitals are inherently complex, stressful work environments; between worried customers and their families who do not want to be there in the first place to the challenges experienced by those who care for them, including varied work hours, variable resources, and often perceived lack of recognition, the potential consequences of a negative hospital culture on productivity, patient satisfaction, and patient safety are enormous (Huseman, 2009). Hospital culture is largely established from the top down and nurse administrators have primary responsibility in establishing environments that promote wellness of patients and staff members. If expectations are not set promoting an optimal culture of safety with a climate in which all clinicians are held accountable to those expectations, departments will establish their own cultures and, unfortunately, ones not always in the best interest of patients, clinicians, and the organizations in which they serve. The ANA Code of Ethics outlines the responsibility of nurse BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 39 leaders to implement and enforce policies, processes, and education to correct behaviors undermining a culture of safety (Lachman, 2014). Nurse leaders must require a positive practice environment; they need to be skilled at crucial conversations in order to do so, as well as role model the behavior expectations they seek to enforce. Administrators should take note that the evidence demonstrates a priority to establish environments that recognize, acknowledge, and openly communicate to achieve a climate of civility as an important component to patient safety (Walrath, 2010). Administrators should know the climate that exists in their organizations through a lens of understanding that a culture of trust, mutual respect and collegiality are hallmarks of a safety culture; they should conduct organizational assessments to guide action planning (Walrath, 2013). In supporting literature, McNamara (2012) acknowledges the potential harmful effects of incivility on patients and recommends equipping nurses with anti-bullying tools, including (a) organizational resources, (b) education, (c) expectations to role model appropriate behavior, and (d) not allowing such behavior to go unaddressed. Administrators need to make resource allocation decisions supporting a positive safety culture but they cannot expect to do so on their own; their actions must empower others in establishing and maintaining a culture of civility and safety throughout all levels of the organization if such a culture is to be sustained. Future Recommendations about Nursing Practice This review study confirmed an increasing association between behaviors undermining a culture of safety and adverse patient outcomes. Undermining safety behaviors, if left unchecked, can create a negative practice environment that spreads just as readily as an aggressive cancer, sickening more and more of the organization and ultimately harming patients. People tend to remember failure more than success, react more strongly to negative stimuli than positive, and BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 40 trust negative information more than positive (Huseman, 2009). Hospital culture in many ways has taught nurses to tolerate, even accept incivility as an unavoidable aspect of the profession – this needs to change going forward. While nurse leaders should establish the framework for a required safety culture through education, behavior standards, and accountability, each individual nurse must embrace the evidence linking uncaring behaviors to patient safety and take personal responsibility in their own practice to create care environments that support wellness. Conclusion The emphasis for hospitals to ensure positive patient outcomes is stronger than ever before. While significant evidence exists regarding the impact of clinician behavior on nurse outcomes such as satisfaction and retention, the purpose of this evidence-based review was to better understand the impact of clinician behaviors that undermine a culture of patient safety on patient outcomes. After an extensive search, critical appraisals were conducted of seven research articles meeting the inclusion criteria. Results demonstrate emerging evidence supporting clinician behavior as a critical element to safety culture and it should no longer take a back seat when setting strategic priorities to enhance patient safety. Hospitals need to assess their cultures and address destructive behavior patterns in order to do what is best for patients, employees, and their bottom line. More research is needed regarding the complexity of care and all aspects of the clinician behavior construct, particularly the direct impact on adverse patient events; these efforts will enrich understanding and support meaningful decision making to improve safety. Huseman (2009) suggests “It is the virus of negativity that must be battled in order to help sick hospitals become well. Only a positive culture can secure the health and wellness for a hospital, its employees and its patients” (p. 63). Through continued research, education, ownership, and personal accountability on the part of the entire healthcare team to remedy behaviors BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 41 undermining to a culture of safety, positive outcomes for patients and all involved can be significantly strengthened. If there is a will and a commitment to do so, healthcare can achieve and exceed the high-reliability of the airline industry; focus on behaviors undermining a culture of safety is an important aspect in achieving that goal. BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 42 References American Association of Colleges of Nursing. (2014). Nursing shortage fact sheet. Retrieved from http://www.aacn.nche.edu/media-relations/fact-sheets/nursing-shortage American Association of Colleges of Nursing. (2012). Graduate-level QSEN competencies: Knowledge, skills and attitudes. Retrieved from http://www.aacn.nche.edu/faculty/qsen/competencies.pdf Andel, C., Davidow, S.L., Hollander, M., & Moreno, D.A. (2012). The economics of healthcare quality and medical errors. Journal of Healthcare Finance, 39(1). 39-50. Retrieved from http://www.wolterskluwerlb.com/health/sites/default/files/JHCF_The%20Economics%20 of%20Health%20Care%20Quality%20and%20Medical%20Errors.pdf Attarian, D. (2008). What is a preventable adverse event? American Academy of Orthopaedic Surgeons Now, 2(5) 22-25. Retrieved from http://www.aaos.org/news/aaosnow/may08/managing6.asp Becher, J., & Visovsky, C. (2012). Horizontal violence in nursing. Medsurg Nursing, 21(4), 210-232. Retrieved from https://www.amsn.org/sites/default/files/documents/practiceresources/healthy-work-environment/resources/MSNJ-Becher-Visovsky-21-04.pdf Buerhaus, P., DesRoches, C., Applebaum, S., Hess, R., Norman, L., & Donelan, K. (2012). Are nurses ready for health care reform? A decade of survey research. Nursing Economics, 30(6), 318-329. Retrieved from http://www.medscape.com/viewarticle/778502_4 Centers for Medicare and Medicaid Services. (2008). Center for Medicaid and state operations. Retrieved from http://downloads.cms.gov/cmsgov/archiveddownloads/SMDL/ downloads/SMD073108.pdf BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 43 Chipps, E., Stelmaschuk, S., Albert, N. M., Bernhard, L., & Holloman, C. (2013). Workplace bullying in the OR: Results of a descriptive study. AORN Journal, 98(5), 479-493. Retrieved from http://dx.doi.org/10.1016/j.aorn.2013.08.015 Flynn, L., Liang, Y., Dickson, G. L., Xie, M., & Suh, D. (2012). Nurses' practice environments, error interception practices, and inpatient medication errors. Journal of Nursing Scholarship, 44(2), 180-186. doi:10.1111/j.1547-5069.2012.01443.x Hines, P. A., & Yu, K. M. (2009). The changing reimbursement landscape: Nurses’ role in quality and operational excellence. Nursing Economics, 27(1), 7-13. Retrieved from http://www.thecamdengroup.com/wp-content/uploads/Nursing-Role-OperationalEffectiveness.pdf Huntington, A., Gilmour, J., Tuckett, A., Neville, S., Wilson, D., and Turner, C. (2011). Is anybody listening? A qualitative study of nurses’ reflections on practice. Journal Of Clinical Nursing, 20, 1413-1422. doi:10.1111/j.1365-2702.2010.03602.x Huseman, R. C. (2009). The importance of positive culture in hospitals. Journal of Nursing Administration, 39(2), 60-63. doi: 10.1097/NNA.0b013e318195a845 Joint Commission on Accreditation of Healthcare Organizations. (2012). Leadership standard clarified to address behaviors that undermine a safety culture. Joint Commission Perspectives, 32(1), 7. Retrieved from http://www.jointcommission.org/assets/1/6/Leadership_standard_behaviors.pdf Kerfoot, K. K. (2009). Good is not good enough: The culture of low expectations and the leader’s challenge. Nursing Economics, 27(1), 54-55. Retrieved from http://www.highbeam.com/doc/1G1-194701259.html BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 44 Lachman, V. D. (2014). Ethical issues in the disruptive behaviors of incivility, bullying, and horizontal/lateral violence. MEDSURG Nursing, 23(1), 56-58. Laschinger, H. K. (2014). Impact of workplace mistreatment on patient safety risk and nurse-assessed patient outcomes. Journal of Nursing Administration, 44(5), 284-290. doi:10.1097/NNA.0000000000000068 Levinson, D.R. (2010). Adverse events in hospitals: National incidence among Medicare beneficiaries. Department of Health and Human Services. Retrieved from http://oig.hhs.gov/oei/reports/oei-06-09-00090.pdf Manojlovich, M., Kerr, M., Davies, B., Squires, J., Mallick, R., and Rodger, G. L. (2014). Achieving a climate for patient safety by focusing on relationships. International Journal for Quality in Health Care, 26(6), 579-584. doi:10.1093/intqhc/mzu068 McNamara, S. A. (2012). Incivility in nursing: Unsafe nurse, unsafe patients. AORN Journal, 95(4), 535-540. doi:10.1016/j.aorn.2012.01.020 Melnyk, M.B., & Fineout-Overholt, E. (2011). Evidenced-based practice in nursing and health care: A guide to best practice (2nd ed.). Philadelphia, PA: Lippincott Williams & Wilkins. Nance, J. J. (2008). Why hospitals should fly: The ultimate flight plan to patient safety and quality care. Bozeman, MT: Second River Healthcare. Polit, D. F., & Beck, C. T. (2012). Nursing research: Generating and assessing evidence for nursing practice (9th ed.). Philadelphia, PA: Lippincott Williams & Wilkins. Porter O’Grady, T., & Malloch, K. (2011). Quantum leadership: Advancing innovation, transforming care (3rd ed.). Sudbury, MA: Jones & Bartlett Learning. Purpora, C., & Blegen, M. (2012). Horizontal violence and the quality and safety of patient care: A conceptual model. Retrieved from http://www.hindawi.com/journals/nrp/2012/306948/ BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 45 Raines, D. A. (2013). Finding the evidence. Neonatal Network, 32(3), 203-205. Retrieved from http://dx.doi.org/10.1891/0730-0832.32.3.203 Roche, M., Diers, D., Duffield, C., & Catling-Paull, C. (2010). Violence toward nurses, the work environment, and patient outcomes. Journal of Nursing Scholarship, 42(1), 13-22. doi:10.1111/j.1547-5069.2009.01321.x Rosenstein, A. H., & O’Daniel, M. (2008). A survey of the impact of disruptive behaviors and communication defects on patient safety. The Joint Commission Journal on Quality and Patient Safety, 34(8), 464-471. Retrieved from http://www.mc.vanderbilt.edu/root/pdfs/nursing/ppb_article_on_disruptive.pdf Sahay, A., Hutchinson, M., & East, L. (2015). Exploring the influence of workplace supports and Relationships on safe medication practice: A pilot study of Australian graduate nurses. Nurse Education Today, 35, 10-16. doi:10.1016/j.nedt.2015.01.012 Sohn, D. (2011). Update on never events. Retrieved from http://www.aaos.org/news/aaosnow/jul11/managing6.asp The Joint Commission. (2008). Behaviors that undermine a culture of safety (Sentinel Event Alert, Issue 40). Retrieved from http//www.jointcommission.org/assets/1/18/SEA_40.pdf Walrafen, N., Brewer, K., & Mulvenon, C. (2012). Sadly caught up in the moment: An exploration of horizontal violence. Nursing Economics. Retrieved from http://www.medscape.com/viewarticle/760015_4 Walrath, J., Dang, D., & Nyberg, D. (2013). An organizational assessment of disruptive clinician behavior: Findings and implications. Journal of Nursing Care Quality, 28(2), 110-121. doi:10.1097/NCQ.0b013e318270d2ba BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 46 Walrath, J., Dang, D., & Nyberg, D. (2010). Hospital RNs' experiences with disruptive behavior: a qualitative study. Journal of Nursing Care Quality, 25(2), 105-116. doi:10.1097/NCQ.0b013e3181c7b58e Wilson, B. L., & Phelps, C. (2013). Horizontal hostility: A threat to patient safety. JONA’s Healthcare Law, Ethics, and Regulation, 15(1), 51-57. doi: 10.1097/NHL0b013e3182861503 Zhan, C., Friedman, B., Mosso, A., & Provost, P. (2006). Medicare payment for selected adverse events: Building the business care for investing in safety. Health Affairs. Retrieved from http://content.healthaffairs.org/content/25/5/1386.long BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY Appendix A Search Flow Diagram 47 BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 48 Among hospitalized patients in acute care settings, how do behaviors that undermine a culture of safety compare to the absence of behaviors that undermine a culture of safety, affect the occurrence of adverse patient safety? Search completed in databases Pub MED (PM) and CINAHL Plus (CNL) Hand search: Journal of Nursing Scholarship, JONA’S Healthcare Law, Ethics, and Regulation, and Journal of Advanced Nursing. Inclusion: Full Text available, Language- English, published in the last 5 years, reviewed, CINAHL Plus- Research Exclusions: Foreign language articles, Articles earlier than 2009. Population Intervention Comparison Outcome Hospitalized patients PM 813 CNL 754 Lateral violence PM 5 CNL 11 Disruptive behavior prevention PM 10 CNL 31 Patient safety PM 4774 CNL 2223 Workplace violence PM 30 CNL 188 Medication errors PM 393 CNL 549 Incivility PM 3 CNL 40 Combined using “or” 785 Hostility PM 71 CNL 113 Disruptive behavior PM 130 CNL 191 All combined using “or” 1270 Combined using “and” 0 All combined using “and” 0 All combined using “and” 0 All combined using “or” 3336 Patient Falls PM 600 CNL 41 Wrong site surgery PM 17 CNL 14 All combined using “and” 0 All combined using “or” 2623 Hand Search All terms 6 BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY Appendix B Critical Appraisals 49 BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 50 Critical Appraisal of Qualitative Research Form Citation: Walrath, J. M., Dang, D., & Nyberg, D (2010). Hospital RNs’ experiences with disruptive behavior: A qualitative study. Journal of Nursing Care Quality, 25(2), 105-116. doi:10.1097/NCQ.0b013e3181c7b58e Purpose: The purpose of the study was to conduct focus groups with RNs to gain an understanding of how RNs describe disruptive clinician behavior and its impact based their observed and actual experiences on the front lines of patient care delivery. Level of evidence: Single Qualitative Study-Level VI Study trustworthiness: Use Polit and Beck pages 509-510 and 576-577 to complete this table. Aspect of study Problem and research questions Comments of strengths and weaknesses Disruptive clinician behavior and the potential effects on organizational culture, nurse satisfaction, and patient safety and care quality are growing concerns that need to be addressed. What are RNs’ perceptions regarding the characteristics of clinician disruption behavior and what is the perceived impact based on their observed and actual experiences in a patient care setting? Theoretical base: Literature review completed, conceptual underpinning Literature review reveals that disruptive behavior is prevalent in healthcare. Joint Commission issued a 2008 Sentinel Event Alert in response to growing recognition that disruptive behavior negatively impacts care quality and patient safety. Regulatory standards now require organizations to have a code of conduct and a process for managing negative behaviors. Despite numerous disruptive behaviors reflected in the literature, most have inconsistent or imprecise definitions. Disruptive behavior is a complex construct and full understanding requires examination of causes, individual responses, effects on individuals and organizations, and perceptions of harm to patients. However, the researchers found no conceptual framework that included these interrelated concepts in a meaningful way. The researchers adapted Pearson and colleagues’ framework on workplace incivility and developed a framework for organizing and describing disruptive behavior, which included 4 primary concepts: triggers, disruptive behaviors, responses, and impacts. Ethical issues Design and tradition No ethical issues were identified. Descriptive qualitative study – no specified tradition BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY Sample and setting Purposive convenience sampling of 96 RNs in an acute care hospital within an academic medical center located in the Northeastern United States. The recruitment process invited participation through information of the study distributed across the Department of Nursing via posters, internal Web sites, and individual letters to RNs (N = 2467). 32.3% of participants were nurse managers and shift coordinators; 52% were staff nurses; 15.6% were advanced practice nurses. 95% of participants were female. 70.8% were white; 12.5% were Asian; 9% were black; 3.1% were Hispanic/Latino. Data collection and procedures IRB approval and oral consent from participants obtained. A clinical psychologist external to the organization facilitated 90-minute focus group sessions, using semi structured interview questions based on the conceptual framework. Focus group size was from 7 to 14 RNs. Pseudo names were used when describing individuals involved in disruptive behavior events to ensure confidentiality of sensitive information. The sessions were audio-recorded and held between January and March 2008. Rigor Reasonable rigor was demonstrated; credentials of researchers indicative of adherence to scholarly research practices. Data analysis The recorded sessions were transcribed verbatim and validated for accuracy against the original recordings. Nudist6 software program designed for narrative analysis was used to manage the interview data and facilitate the coding process. Deductive and inductive processes were used to code the data. Two members of the research team independently assigned codes to text segments of the transcribed interviews. After reaching consensus on the codes through comparison and discussion, the full research team was convened to review, identify patterns, and synthesize the initial codes into broader categories. These categories were further synthesized into major themes and organized according to the 4 primary concepts in the conceptual framework. Findings and theoretical integration Participants reported the occurrence of disruptive behaviors in all practice settings and between /among a wide variety of healthcare personnel. 168 different disruptive behaviors were identified and then 51 BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY synthesized into 21 categories. Within these categories, 3 themes emerged: incivility, psychological aggression, and violence. The 10 most frequently identified categories within these themes were rude/disrespectful (Incivility); engaging in gossip, intimidation/threats, passive aggressive behavior, refusal to do one’s job, verbal aggression, power play, condescending language/dress down, professional disregard (Psychological aggression); and physical violence (Violence). Out of the personal experiences reported, 225 disruptive behavior events were coded. Physicians were identified as instigators in 42% of events; nurses in 29% of events; support personnel in 27% of events; and management in 2% of events. Triggers, RN responses, and impacts on the RN, patient, and nurse’s practice setting were also identified. Interpretations, implications and recommendations This study adds evidence that disruptive behavior has been observed or experiences throughout all levels of nursing and among major professional groups. In addition to RNs and MDS, support personnel were identified as instigators and targets. The impact on the organization increases as the roles and numbers of individuals involved in disruptive behavior grows. Disruptive behavior affects the RN, patient, and the practice setting. Distraction from patient care, physical and emotional distress, and priority conflicts between patient care and operational needs were described by the RN participants. Concerns regarding a decrease in quality care, increased risk to patient safety, care delivery delays, and disrupted working relationships were also described. Recommendation: Increasing nurse leaders’ and staff’s awareness and creating an environment in which disruptive behavior is recognized, acknowledged, and openly discussed are important steps in establishing a culture of civility and patient safety. Global issues See literature review section above. Overall Comments from analysis: (speak to credibility, dependability, transferability & confirmability) 52 BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 53 Credibility: (confidence in the truth) The study was limited to RNs due to the funding agency’s requirements which limits representativeness of the findings; while there is no reason to question the validity of findings among the participants, results and understanding of the issues could be enhanced by wider participation among diverse groups of healthcare professionals. Dependability: (stability over time) Convenience sampling of volunteers resulted in participants not representative of the population of RNs employed in the organization. Participants were older, more experienced, more educated, and less diverse than the body of nursing staff where this study was conducted. A 3.9% response rate and the potential that participants were victims of disruptive behavior over the course of their careers and were more ready to share their experiences raises the possibility of selection bias. Transferability: (to other settings) Findings from study focus groups represent RNs experiences and observations in an academic medical center and may not be representative of experiences in other hospital settings. Confirmability – (objectivity or neutrality of the data and interpretations) The linear relationship of the variables presented in the conceptual framework influenced the researchers’ approach to the data collection and also may have influenced the analysis of the qualitative data. Further exploration of the interdependencies and relationships among the 4 framework concepts would deepen understanding. Despite the study limitations, the lived experiences described by RN participants provide insight into the disruptive behavior construct and provides direction for future inquiry of disruptive behavior in acute care settings. BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 54 Critical Appraisal of Quantitative Research form Citation: Chipps, E., Stelmaschuk, S., Albert, N. M., Bernhard, L., & Holloman, C. (2013). Workplace bullying in the OR: Results of a descriptive study. AORN Journal, 98(5), 479-493. http://dx.doi.org/10.1016/j.aorn.2013.08.015 Study purpose or research questions: “The study sought to determine whether the demographic variables of gender, ethnicity, hospital, years of experience on the unit, years in the profession, and job title predict the experience of workplace bullying; whether a relationship exists between workplace bullying and emotional exhaustion; and whether bullying is associated with perceptions of patient safety in the OR” (Chipps, Albert, Bernhard, and Holloman, 2013, p.1). Level of evidence: Level VI- descriptive study Study validity: Use your research text to guide you in determining bias in the following steps of the research process (Polit and Beck pages 230-231. Validity analysis criteria Problem and purpose statements Mark an x if very serious concerns Your comments re major strengths and weaknesses The problem in the study is workplace bullying in the OR. The purpose of this study was to: Describe the incidence of workplace bullying among perioperative RNs, surgical technologists, and unlicensed perioperative personnel at two academic medical centers Determine whether the demographic variables of gender, ethnicity, years of experience on the unit, years in the profession, and job title predict the experience of workplace bullying Determine whether there is a relationship between workplace bullying and emotional exhaustion among perioperative staff members Determine whether workplace bullying is associated with perceptions of patient safety in the OR BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY Theoretical base from lit review and conceptual framework and concept definitions This study used a model of bullying from Hutchinson et al. In this model “organizational antecedents” must be present for bullying to exist in the work environment. Bullying includes terms of workplace incivility, disruptive behaviors, peer incivility, horizontal violence, and lateral violence. Design Cross-sectional survey. Ethical issues No ethical issues were identified Sample and setting Inclusion and exclusion criteria Selection method (random selection or assignment, convenience Size of n Included RNs, surgical technologists, unlicensed perioperative personnel working in ORs at two academic Magnet medical centers Measurement tools *Negative Acts Questionnaire- Revised (NAQ-R)22 items. Cronbach alpha scores ranging from 0.81 to 0.92 Exclusion criteria included employment for fewer than six months on the unit and less than a 50% work week n= 167 *Nine item Emotional Exhaustion Subscale of the Maslach Burnout Inventory (MBI) Seven point Likert scale 0-6, never to daily, scores split and coded into 0-16-low, 17-26-moderate, 27 or morehigh. Cronbach alpha score 0.91. *23 additional questions including eight demographic questions, eight questions related to bullying experiences and witnessing bullying behaviors at work, and seven questions about the effect of bullying on near errors, errors, expectations, and safety of patients. Nurse experts, clinical nurse specialists, nurse administrators, and staff nurses reviewed questions for clarity. 55 BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY Data collection After receiving institutional review board approval at both hospitals, the research team met with staff to introduce the study. Surveys were put in mailboxes of all eligible participants with cover letters stating that potential participants could opt out by simply not returning the survey. Procedures The return of the survey implied consent. Enrollment lasted for 1 month. At hospital A surveys were returned via sealed envelope in a locked box in the break room. Hospital B surveys were given preaddressed envelopes to be returned to the hospital principal investigator via interoffice mail. Data analysis SPSS Statistics software to analyze the data. Inferential statistics, correlational analysis, multiple regression, and logistic regression analyses. Findings (discussion of results) and Demographic differences were significant between hospitals. Interpretation of findings : conclusions of what is true , implications of conclusions Approximately one-third of participants would be characterized as targets of workplace bullying. 59% reported witnessing coworkers being bullied 6 % reported they never experienced bullying on all 22 items Perpetrators Other employees on unit 56% RNs on their unit 56% Physicians 44% RN managers 33% Charge RNs 11% Hospital A almost 3 times more likely to be a target for bullying than Hospital B White respondents reported bullying intensity scores 3.8 points higher than black respondents and 4.7 points higher than “other” respondents A significant moderate, positive correlation among 56 BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 57 bullying frequency, bullying intensity, and emotional exhaustion exists. A moderate, negative correlation of bullying frequency, bullying intensity, and job satisfaction exists. 3% indicated that bullying affected errors and perceptions of patient satisfaction. 6% indicated that bullying affected patient safety Respondents associated 8 negative acts with perceived compromises in patient safety Recommendations based on implications Further descriptive research on workplace bullying in the OR. Interventions to ameliorate workplace bullying. Incorporate workplace bullying messages into training programs. Presentation Association of Peri Operative Registered Nurses (AORN) journal. Credentials of the researcher Chipps PhD, RN Stelmaschuk BSN, RN Albert PhD, CCNS, CHFN, CCRN, NE-BC, FAHA, FCCM Bernhard PhD, RN Holloman PhD Assessment of validity of findings. There were 3 tools used. The first two tools are established measurement tools and measure what they are supposed to measure. The third tool used questions made up by the authors, these questions were peer-reviewed for clarity but the questions may have not specifically answered what the authors were trying to get answered. Study Reliability: The consistency of the tools used is good so reliability would be good. What are the results? What are the statistical answers to the research questions (statistical significance)? BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 58 NAQ-R behavior Monthly Weekly Daily Total Having your opinion ignored 13.3% 8.5% 6.1% 27.9% Being shouted at 14.5% 10.2% 2.4% 27.1% Withholding information that affects your performance 8.6% 11.0% 6.7% 26.3% Being humiliated or ridiculed 10.3% 11.5% 3.6% 25.4% Having gossip or rumors spread about you 7.4% 9.3% 8.6% 25.3% Ordered to do work below your competency level 6.8% 6.8% 9.3% 22.9% Being ignored or isolated from the rest of the work group 6.7% 11.0% 3.7% 21.0% Being ignored or facing hostility when you approach 10.4% 6.1% 2.4% 18.9% Insulting or offensive remarks about you 5.5% 6.1% 5.5% 17.1% Key areas of responsibility replaced with trivial/unpleasant tasks 4.9% 8.6% 3.1% 16.6% Excessive monitoring of your work 5.6% 6.8% 3.1% 15.5% Persistent criticism of your work 6.1% 5.5% 3.0% 14.6% Assigned tasks with impossible deadlines 12.0% 10.0% 2.0% 24.0% Unmanageable workload 6.1% 6.1% 1.8% 14.0% Repeated reminders past of errors 7.3% 4.3% 1.8% 13.4% Pressure to give up what you are entitled to (eg, sick time, vacation) 6.7% 4.3% 1.8% 12.8% Subject of constant teasing or sarcasm 5.5% 3.0% 4.2% 12.7% Practical jokes carried out by people you get along with 5.5% 1.8% 4.3% 11.6% Intimidating behavior such as shoving or finger-pointing 4.9% 3.7% 2.4% 11.0% Having allegations made against you 6.1% 2.4% 2.4% 10.9% Hints to quit your job 2.4% 2.4% 0.6% 5.4% Threats of violence and physical abuse 2.4% 0.6% 0.6% 3.6% Average number of bullying acts that participants experienced more often than never (ie, intensity) was 9.7 (SD 6.38) BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 59 Average of 2.1 (SD 3.75) acts weekly or daily (ie, frequency) Most frequently experienced acts occurring weekly or daily were having rumors or gossip spread (50%), being ordered to work below competency level (46.3%), being humiliated (45.4%), having information withheld (43.6%), and being excluded (41.8%). A significant moderate, positive correlation among bullying frequency (rho .56, P < .001), bullying intensity (rho .54, P < .001), and emotional exhaustion exists. There is a moderate, negative correlation among bullying frequency (rho e.31, P < .001), bullying intensity (rho e.29; P < .001), and job satisfaction. Eight negative acts in this study with perceived compromises in patient safety impossible deadlines (odds ratio 2.4 [95% CI, 1.4-4.0]) having opinions ignored (odds ratio 2.3 [95% CI, 1.4-3.7]) having false allegations made (odds ratio 2.0 [95% CI 1.2-3.3]) excessive monitoring of work (odds ratio 2.0 [95% CI, 1.2-3.1]) hints from others that the respondent should quit his or her job (odds ratio 1.9, [95% CI, 1.0-3.5]) being reminded of errors or mistakes (odds ratio 1.8 [95% CI, 1.1-3.0]) being humiliated at work (odds ratio 1.8 [95% CI, 1.1-3.0]) being the target of practical jokes (odds ratio 1.7 [95% CI, 1.1-2.8]). What is the clinical significance of the results? The clinical significance of the results is that workplace bullying was shown to affect the perception of compromised patient safety. Applicability: This was an OR study which can limit the applicability to lower stress units of care. Overall Comments on validity and reliability: There are limitations to this study since crosssectional data was used and precludes attribution of cause and effect among the study variables. The low questionnaire response rate of 28.7% also is limiting. BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 60 Critical Appraisal of Quantitative Research form Citation: Flynn, L., Liang, Y., Dickson, G. L., Xie, M., & Suh, D. (2012). Nurses' practice environments, error interception practices, and inpatient medication errors. Journal of Nursing Scholarship, 44(2), 180-186. doi:10.1111/j.1547-5069.2012.01443.x Study purpose or research questions: “to determine the relationships among characteristics of the nursing practice environment, nurse staffing levels, nurses’ error interception practices, and rate of nonintercepted medication errors in acute care hospitals” (Flynn, Liang, Dickson, Xie, and Suh, 2012, p 180). Level of evidence: Level IV- single observational study Study validity: Use your research text to guide you in determining bias in the following steps of the research process (Polit and Beck pages 230-231. Validity criteria analysis Mark an x if very serious concerns Problem and purpose statements Your comments re major strengths and weaknesses Problem- medication errors Purpose- “to determine the relationships among characteristics of the nursing practice environment, nurse staffing levels, nurses’ error interception practices, and rate of nonintercepted medication errors in acute care hospitals” (Flynn, Liang, Dickson, Xie, and Suh, 2012, p 180). Theoretical base from lit review and conceptual framework and concept definitions Reason’s error theory Design Correlational Ethical issues No ethical issues- reviewed by Rutgers University Institutional Review Board and IRBs of participating hospitals. Sample and setting Inclusion and exclusion criteria Inclusion- survey participants be registered nurses employed in a position of staff nurse on their unit. Exclusion- float staff not included. All nurses that met inclusion criteria were invited to The Nursing Organization and Outcomes Model- link between the presence of characteristics in the environment that support professional nursing practice and positive patient outcomes. BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY Selection method (random selection or assignment, convenience Size of n Measurement tools 61 participate. n= 686 *PES-NWI *Four item scale of interception practices Data collection 8 month period- number of medication errors per 1000 patient days and the number of RN hours per patient day. Nurse surveys distributed and collected by study liaison. Procedures Participants given written document- informed consent, description of study, study purpose, and rights as research subject. Mean response rate 96% Data analysis Correlation coefficients computed between variables Findings (discussion of results) and Interpretation of findings : conclusions of what is true , implications of conclusions Recommendations based on implications A supportive practice environment was positively associated with error interception practices among nurses in the sample of medical-surgical units. Importantly, nurses’ interception practices were inversely associated with medication error rates. Presentation Journal of Nursing Scholarship Credentials of the researcher Flynn PhD, RN, FAAN Liang PhD Dickson PhD, RN Xie PhD Suh PhD The validity of the findings is sound. The studies evaluating methods are measuring the concepts that they are trying to measure. Assessment of validity of findings. Nurses need supportive environments to intercept medication errors. BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 62 Study Reliability: The consistency of the tools used is good so reliability would be good. What are the results? What are the statistical answers to the research questions (statistical significance)? Variable β SE df t p Nurses’ interception practices −0.19 0.08 73.98 −2.48 .015 Nursing practice environment −0.26 0.30 79.95 −0.87 .388 composite score What is the clinical significance of the results? If nurses have a supportive environment they employ practices that can assist in interrupting medication errors before reaching the patient. Applicability: Study is applicable with the high number of medication errors. Overall Comments on validity and reliability: The biggest problem with this study is the use of incidence reports and the underreporting of medication errors or near errors. BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 63 Critical Appraisal of Quantitative Research form Citation: Laschinger, H. K. (2014). Impact of workplace mistreatment on patient safety risk and nurse-assessed patient outcomes. Journal of Nursing Administration, 44(5), 284-290. doi:10.1097/NNA.0000000000000068 Study purpose or research questions: “To investigate the impact of subtle forms of workplace mistreatment (bullying and incivility) on Canadian nurses’ perceptions of patient safety risk and, ultimately, nurse-assessed quality and prevalence of adverse events” (Laschinger, 2014, p. 284). Level of evidence: Level IV- Single observational study Study validity: Use your research text to guide you in determining bias in the following steps of the research process (Polit and Beck pages 230-231. Validity analysis criteria Problem and purpose statements Mark an x if very serious concerns Your comments re major strengths and weaknesses The problem in the study is the impact of bullying and incivility on patient safety risk and nurse-assessed patient outcomes. The purpose of this study was “to investigate the impact of subtle forms of workplace mistreatment on Canadian nurses’ perceptions of patient safety risk and, ultimately nurse-assessed quality and prevalence of adverse events” (Laschinger, 2014, p. 284). Theoretical base from lit review and conceptual framework and concept definitions Concept of workplace bullying of Einarsen and Mikkelsen Design Correlational Ethical issues No ethical issues Sample and setting Inclusion and exclusion criteria Selection method Inclusion- Ontario hospital nurses on College of Provincial registry list. Exclusion- not on list Construct of workplace incivility of Andersson and Pearson Random sample of Ontario hospital nurses BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY (random selection or assignment, convenience Size of n Measurement tools 64 Response rate of 52% n= 641 *NAQ-R Negative Acts Questionnaire Revised *Cortina’s Workplace Incivility Scale *5-point Likert scale for perceptions of the effects of negative interpersonal interactions in the workplace *Sochalski Scale 0-4 rating nurses perceptions of the frequency of common adverse patient outcomes over the past year *Aiken et al 1-4 rating the quality of care of their unit Data collection Questionnaire mailed out to participants Responders: 88.7% women 60.7 baccalaureate prepared 69% full time 78.3% acute care Procedures Questionnaire mailed out initially then reminder letter sent 3 weeks later then a replacement package sent out 1 month after reminder. Data analysis Used Statistical Package for Social Sciences. Direct and Indirect effects of bullying and incivility on quality of care and frequency of adverse events. Used the approach of Baron and Kenny to test mediationthe extent to which an intervening variable influences the impact of an independent variable on an outcome variable. Findings (discussion of results) and Interpretation of findings : conclusions of what is true , Bullying and all sources on incivility were significantly related to nurse-assessed quality of care, adverse events, and perceptions of patient safety risk. Patient/family complaints were the individual adverse BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY implications of conclusions 65 event most strongly related to bullying and physician and coworker incivility. Subtle forms of workplace mistreatment can have detrimental effects on patient safety outcomes. Recommendations based on implications Create environments that support professional nursing practice that promote high-quality patient care and establish positive patient safety cultures. Prevent negative interpersonal interactions; establish zero tolerance bullying/workplace incivility policies. Presentation Article in the Journal of Nursing Administration (JONA) Credentials of the researcher Assessment of validity of findings. PhD, RN FAAN, FCAHS The validity of the findings is sound. The studies evaluating methods are measuring the concepts that they are trying to measure. Study Reliability: The reliability or accuracy and consistency of the study are reliable. What are the results? What are the statistical answers to the research questions (statistical significance)? Descriptive statistics mean (SD) Exposure to bullying experience was not high 1.45 (0.59) Nurses reported relatively high quality of patient care on their units 3.34 (0.69) Relatively few experiences of adverse events 2.03 (0.69) Low workplace violence-related patient safety risk 2.31 (1.04) Mediating Effects of Patient Safety Risk Patient care quality and physician incivility B= -0.234, p< .05 Bullying and overall frequency of patient adverse events B= 0.241, p< .05 Physician incivility and overall frequency of patient adverse events B= 0.166, p< .05 Coworker incivility B= 0.148, p< .05 BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 66 Workplace mistreatment related to patient safety risk Bullying B= 0.328 Physician incivility B= 0.228 What is the clinical significance of the results? Patient safety is the clinical significance. Applicability: Overall, the study suggests that workplace mistreatment can threaten patient safety outcomes. Overall Comments on validity and reliability: There are limitations to this study since crosssectional data was used and precludes attribution of cause and effect among the study variables. The low questionnaire response rate and targeted sample limit generalizability and patient outcomes were nurse-assessed not institutional data. BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 67 Critical Appraisal of Quantitative Research form Citation: Roche, M., Diers, D., Duffield, C., & Catling-Paull, C. (2010). Violence toward nurses, the work environment and patient outcomes. The Journal of Nursing Scholarship, 42(1), 13-22. Doi: 10:1111/j.1547-5069.2009.01321.x Study purpose or research questions: “To relate nurses’ self-rated perceptions of violence (emotional abuse, threat, or actual violence) on medical-surgical units to the nursing working environment and to patient outcomes,” (Roche, Diers, Duffield, & Catling-Paull, 2009). Level of evidence: Single correlational/observational study-Level IV Study validity: Use your research text to guide you in determining bias in the following steps of the research process (Polit and Beck pages 230-231. Validity criteria analysis Mark an x if very serious concerns Problem and purpose statements Theoretical base from lit review and conceptual framework and concept definitions Design Ethical issues Sample and setting Inclusion and exclusion criteria Selection method (random selection or assignment, convenience Size of n Measurement tools Your comments re major strengths and weaknesses Problem-An unsafe working environment is detrimental to nurses’ ability to deliver safe, quality care. Purpose-Rate nurses’ perception of violence in medicalsurgical units and relate this to patient outcomes Conceptual Framework Cross sectional collection of data. No ethical issued identified 94 randomly selected medical surgical wards in 21 public hospitals across two states in Australia. ED’s, ICU’s, Pediatrics, Obstetrics, and Psychiatric units were excluded. Random selection All nurses on the floor were asked to complete survey including clinical nurse specialists, registered nurses, enrolled nurses, certified nursing assistants, and training nurses were polled. N=3099, overall response rate 80.3% 49 item Nursing Work Index-Revised Environmental Complexity Scale 11 question nursing intervention questionnaire about interventions that were delayed or not done. Staffing matrix of the institutions BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY Data collection 68 PRN-80 Patient acuity scale Surveys were collected for seven consecutive days on each unit from 2004-2006 and primary data were collected by a trained nurse data collector. RN=72.3 Procedures Data analysis Findings (discussion of results) and Interpretation of findings : conclusions of what is true , implications of conclusions Recommendations based on implications Presentation Credentials of the researcher Assessment of validity of findings. Surveys were filled out for seven consecutive days on each unit and were collected by trained nurse data collectors with no affiliation to the hospital. Data was collected from nurses and also by matrix and census of the floor. Concurrent medical records were also used. Categorical variables were transformed to X per ward. Continuous variables were calculated as a mean for the ward. Explanatory variables were added to statistical models in sequence using a -2 log likelihood value. Poisson regression models were used in the case of low event counts of patient outcomes. As ward environments becomes less stable (fewer RN’s, increased workload, unanticipated changes in patient status, perceived low nurse leadership, low nurse autonomy, poor relationships with physicians, patients awaiting placement) perceived violence increases. This increases the poor patient outcomes related to patient falls. Use tools to identify violent patients. Encourage reporting of incidents, management support strategies, agencies must address disruptive behavior of any employee or participating physician. Journal of Nursing Scholarship Michael Roche, RN, MHSc, CertMHN Donna Diers, RN, PhD Christine Duffield, RN, MHP, PhD Christine Catling-Paull, RN, MSc, RM The validity of the findings is sound. The study variables adequately measure violence (actual and perceived) toward nurses and the patient outcomes. Study Reliability: What are the results? What are the statistical answers to the research questions (statistical significance)? BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 69 Correlation of Patient Adverse Events per Ward and Nurses Experiencing Violence Falls Med Errors Delays in med admin Physical Violence 0.21 0.22 0.15 Threat of Violence 0.19 0.22 0.10 The threat of physical violence along with actual physical violence is statistically relevant for adverse patient outcomes. There is a positive correlation between the three outcomes and actual physical violence. There was a positive correlation between threats of violence and medication delays and falls. Out of 947 nurses that reported emotional abuse, 14.7% stated that they had received emotional abuse from a nursing co-worker and 9.8% polled that they had received emotional abuse from more than one source. What is the clinical significance of the results? If nurses have adequate resources and a full staffing matrix, poor patient outcomes are decreased. Perceived violence will increase the likelihood that nurses will seek employment elsewhere. Applicability: The study is applicable to medical-surgical units exclusively. Further testing would be needed to apply to all floors in the acute care setting. It is also polling violence that was from patients directed at nurses not just nurse to nurse or physician to nurse violence. Overall Comments on validity and reliability: The issue with validity and reliability is that the study depends of the reporting of incidence which it states the nursing staff is not always filling out the correct paperwork or they are reluctant to do so. BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 70 Critical Appraisal of Quantitative Research form Citation: Walrath, J. M., Dang, D., & Nyberg, D. (2013). An organizational assessment of disruptive clinician behavior: Findings and implications. Journal of Nursing Care Quality, 28(2), 110-121. doi:10.1097/NCQ.0b013e318270d2ba Study purpose or research questions: To understand the complexities of disruptive behavior in a large academic medical center in order to 1) determine type, frequency and scope of clinicians’ personal experience with disruptive behavior and impact on staff, patients, and the organization 2) compare the disruptive behavior experiences of RNs and MDs, and 3) customize interventions for RNs, MDs, interprofessional teams and the organization to foster culture change and enhance patient safety. Level of evidence: Single Correlational Study –Level IV Study validity: Use your research text to guide you in determining bias in the following steps of the research process (Polit and Beck pages 230-231. Validity analysis criteria Problem and purpose statements Mark an x if very serious concerns Your comments re major strengths and weaknesses Problem: Disruptive behavior between clinicians is an entrenched and intractable problem that undermines the culture of safety for patients and clinicians. The purpose of the study was to understand the complexities of disruptive behavior in a large academic medical center. The objectives were to 1) determine the type, frequency, and scope of clinicians’ personal experiences with disruptive behavior and impact on staff, patients, and the organization; 2) compare disruptive behavior experiences of RNs and MDs; 3) customize interventions for RNs, MDs, interprofessional teams, and the organization to foster culture change and enhance patient safety. Theoretical base from lit review and conceptual framework and concept definitions Disruptive behavior is a multidimensional construct demonstrated by numerous types of behaviors; current literature presents a fragmented perspective of this complex problem. In a previous qualitative study (See Walrath, Dang, & Nyberg, 2010), the authors presented Johns Hopkins Model for Disruptive Clinical Behavior to increase clarity to the large literature base and improve understanding on the topic. This model explains disruptive behavior using 4 concepts: triggers, disruptive BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 71 behaviors, responses, and impacts. Disruptive behavior is defined as “personal conduct, whether verbal or physical, that negatively affects or potentially may affect patient care including, but not limited to, conduct that interferes with one’s ability to work with the other members of the healthcare team.” The survey instrument subsequently developed and used in this study was guided by this conceptual model. Design Descriptive survey; an instrument Disruptive Clinician Survey for Hospital Settings was developed to assess disruptive behavior among healthcare professionals in the hospital practice environment. This study is in follow-up to a previous qualitative study in which a conceptual model for disruptive behavior was presented. (See Walrath, Dang, & Nyberg, 2010). The design is an appropriate “next step” in researching this subject. Ethical issues No ethical issues apparent or identified. Sample and setting Inclusion and exclusion criteria Selection method (random selection or assignment, convenience Size of n Convenience sample. Total study population N = 5710 in one academic medical center. 3 clinician groups – all levels of clinical and administrative RNs (n = 2759); nurse practitioners, certified nurse midwives, certified RN anesthetists, and physician assistance (n = 470); full time School of Medicine clinical faculty, fellows, and house staff MDs (n = 2481). Nurses and MDs in all practice settings were included; agency RNS, RNs not employed by the department of nursing and School of Medicine clinical faculty and fellows currently not practicing in the study hospital were excluded. Response rate = 27.3% Study was limited to RNs and MDs, and affiliates due to funder’s restrictions. Measurement tools Disruptive Clinician Survey for Hospital Settings Survey items included dichotomous, 4 and 5-point Likert scales, and multiple choice patterns which were answered based on their personal experiences “during the past year”. BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY Data collection 72 The survey was available from October 11-November 1, 2010 on a secured Web-based system. 1559 clinician participants 35.8% (n = 987) RNs 20% (n = 496) MDs 16.2% (n = 76) affiliates Most RNs and affiliates (89.3%) = female; most MDs (60.9%) = male Procedures After IRB approval was obtained, an email was sent to work addresses of study population inviting study participation with a link to Web-based survey. Completion of survey implied informed consent. Participants could complete the survey at work or on their own time. Three email reminders were sent during the three week study period. Data analysis Descriptive, univariate, and bivariate analyses were conducted using IBM SPSS 19. The Levine test for equal variance was nonsignificant. Items with missing values were deleted from the analyses. Findings (discussion of results) and Interpretation of findings : conclusions of what is true , implications of conclusions 84% of respondents reported personally experiencing disruptive behavior during the past year. 73% of respondents reported observing a coworker who was a target of this behavior. RNs experienced a significantly higher frequency of disruptive behaviors and triggers than MDs; 45% of MDs and 37% of RNs reported that their peer’s disruptive behavior affected them most negatively. Disruptive behavior was reported more frequently within the MD staff (45.1% in comparison to 36.5% among RN staff) and the affiliates reported MDs as having the most negative impact. Most prominent trigger for both MDs and RNs was organizational in nature - pressure from high census, volume, and patient flow. 189 incidences of patient harm related to disruptive behavior were reported by study participants. Recommendations based on implications Disruptive behavior is a complex phenomenon with significant implications for staff, patients, and organizations if not addressed. An organizational assessment identifying the full scope of disruptive behaviors is a first step to achieving and sustaining a culture of trust, mutual respect, and collegiality which are BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 73 the hallmarks of a culture of safety. The Johns Hopkins Model for Disruptive Clinician Behavior provides a roadmap for such an assessment (see Walrath, Dang, & Nyberg, 2010) and the survey provides actionable information to address disruptive behavior as a systems issue and can guide development of individual, team, and organizational interventions. Presentation Article in the Journal of Nursing Care Quality Credentials of the researchers Jo M. Walrath, PhD, RN Deborah Dang, PhD, RN, NEA-BC Dorothy Nyberg, MS, RN Assessment of validity of findings. Reasonably sound validity of findings: see overall comments below. Study Reliability: What are the results? What are the statistical answers to the research questions (statistical significance)? An independent-sample t test was performed to compare RNs’ and MDs’ means for each item in the survey. (Affiliates were excluded from the analyses due to small sample size.) RNs reported experiencing a significantly higher frequency of all disruptive behavior items than MDs. The five highest rank-ordered means by role in the Disruptive Behavior subscale were: RN MD n mean (SD) n mean (SD) P Passive aggressive 731 3.03 (1.29) 342 2.65 (1.27) <.001 Conflict 733 3.02 (1.11) 343 2.61 (1.14) <.001 Malicious gossip 725 2.86 (1.28) 342 2.27 (1.14) <.001 Self-centered 730 2.81 (1.21) 344 2.64 (1.23) .03 Inappropriate use of 724 Communication tech. 2.72 (1.62) 344 2.01 (1.26) <.001 BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 74 RNs reported a higher frequency of occurrence for all triggers of disruptive behavior. All subscale items were significant for RNs compared with MDs, except for the item lack of competency. The 5 highest rank-ordered means by role for the Trigger subscale were: Pressure from high 727 census, volume, and patient flow 3.32 (1.24) 339 2.81 (1.37) <.001 Environmental over- 725 load 3.21 (1.37) 338 2.54 (1.38) <.001 Chronic, unresolved 722 system issues 3.14 (1.29) 338 2.71 (1.35) <.001 Personal characteristics 720 2.92 (1.21) 336 2.66 (1.19) .001 Unit/org. culture 724 2.90 (1.34) 340 2.62 (1.36) .001 What is the clinical significance of the results? Disruptive behavior is an organizational problem which undermines a culture of safety. A major finding of this study is that participants reported direct knowledge of actual harm (rather than the perception of harm) to patients as a result of disruptive behavior. Of the 186 reported incidents of harm, 77.2% were rated as temporary (requiring treatment or intervention, or prolonged hospitalization), 10% permanent (wrong procedure or wrong site surgery), and 12.7% requiring life-sustaining interventions (intubation or emergency surgery). Applicability: Similar hierarchical structures and common processes are inherent in all hospital organizations which would allow for generalization outside an academic medical center settings, implying significant potential impact for patients in America as well as globally. Overall Comments on validity and reliability: Based on the rigor of survey instrument development and findings, we can infer reasonable validity and reliability with the following caveats: Due to the perception that the connotations of the term disruptive behavior may predispose how respondents answered, the survey instrument has since been retitled to the more neutral phrasing Survey of Unprofessional Behaviors: Triggers, Responses, Impacts. The findings in this study indicated that clinicians speak up and do not let disruptive behavior get in the way of patient care, an alteration from previous research findings which demonstrated intimidation is a barrier to reporting. However, because of the sensitivity of this item, the authors acknowledge the possibility that participants sacrificed the accuracy of their responses in favor of one that would be perceived as more socially acceptable. BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 75 A response rate of 27.3%, lack of data on non-responders, and potential that responders were victims of disruptive behavior raise into question possible selection bias and representativeness of the results. Survey length and specificity of demographic questions may have contributed to overall response rate and subscale variability due to fatigue while responding and fear of being identified; the survey has since been shortened and specificity of demographic items has been decreased. BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 76 Critical Appraisal of Quantitative Research form Citation: Wilson, B.L. & Phelps, C. (2013). Horizontal hostility: A threat to patient safety. JONA’S Healthcare Law, Ethics, and Regulation, 15(1), 51-57. doi:10.1097/NHL0b013e3182861503 Study purpose or research questions: “The purpose of this study was to survey registered nurses at a 220-bed community hospital in the Southwest to determine to degree of perceived hostility in the workplace, and (if present) to determine to extent that horizontal hostility behaviors from either RN-to-RN or physician-to-RN influenced nurse behaviors directly related to patient care,” (Wilson &Phelps, 2013). Level of evidence: Single observational study Level IV Study validity: Use your research text to guide you in determining bias in the following steps of the research process (Polit and Beck pages 230-231. Validity criteria analysis Mark an x if very serious concerns Problem and purpose statements Theoretical base from lit review and conceptual framework and concept definitions Design Ethical issues Sample and setting Inclusion and exclusion criteria Selection method Your comments re major strengths and weaknesses Problem: Healthcare workers that feel intimidated or bullied are less likely to speak out when they see an error in patient care and are more likely to take part in “workarounds” in order to not deal with bullying individuals. Purpose: 1) To determine the degree of perceived hostility in a 220 bed hospital. 2) To determine to degree of RN-to-RN and physician-toRN hostility 3) Determine how this influences nurse’s behaviors directly related to patient care. The study was modeled on previous studies from the American Association of Critical Care Nurses, “ Lateral Violence in Nursing” and “Seven Crucial Conversations in Healthcare.” Cross sectional survey No ethical issued identified Surveys were given to all five hundred nurses working in a 220-bed hospital during a 2 month period. Exclusions: Registry and travel nurses N=500 BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY (random selection or assignment, convenience Size of n Measurement tools Response rate was 26% Ordered and dichotomous 28 question survey based on a survey in a previous study titled “Lateral Violence in Nursing Survey.” Surveys were given to all who met inclusion criteria. The surveys were to be filled out and returned to locked boxes. Data collection Procedures Data analysis Findings (discussion of results) and Interpretation of findings : conclusions of what is true , implications of conclusions Recommendations based on implications 77 x Respondents: 10 years of experience= 58% baccalaureate degree=58% female = 90% 30-39 years old= 23.3% 40-49 years old= 35.3% 50 and older= 31.5% Surveys were handed out and nurses were asked to return the surveys in a sealed enveloped in high traffic areas as to protect anonymity such as near time clocks or in highly frequented hallways. Surveys were collected twice weekly and reviewed and kept in a locked filing cabinet. They were reviewed and transcribed by a nurse researcher with no affiliation to the hospital and no knowledge of the unit locations. Univariate analysis was performed. No discussion of Levine’s test. 60% (n=78) of respondents had witnessed horizontal hostility in the last month of working. The top answer for who was giver of the horizontal hostility was “a nurse from my unit.” (n=66) followed by a physician (n=53). Of those who answered this question 58% (n=60) stated they spoke with a peer about this problem. 17.3% (n=18) stated they spoke directly to a manager. The top reason people chose to ignore the horizontal hostility was that it would make the situation worse. 1) Educate staff nurses about horizontal hostility and why it exists. 2) Examine your own leadership style 3) set behavior standards and keep employees accountable to them 4) Provide ongoing training to managers and charge nurses 5) Provide nurses with skills to be able to address conflict BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY Presentation Credentials of the researcher Assessment of validity of findings. 78 with peers like conflict management training and assertiveness 6) Give new nurses a shield (provide coaching about deflecting) 7) Give new nurses a chance to bond with one another 8) Offer 2 way feedback for new nurses and their preceptors 9) Practice self-evaluation Article in JONA’S Healthcare Law, Ethics, and Regulation Barbara L. Wilson, PhD, RNC-OB Connie Phelps, MSN, RNC-OB The validity is sound. The study measures what they have set out to measure which is horizontal hostility among nurses. Study Reliability: What are the results? What are the statistical answers to the research questions (statistical significance)? 60% of respondents stated they had seen horizontal hostility in the last month. Of those who had witnessed it, 61% stated it came from a nurse from their own department, 49.5 stated that it came from a physician, 27.1% stated that it came from a charge nurse, and 24.3 stated that it came from an employee from an unspecified department. When asked who they spoke about it with, 57.3% stated they spoke with a co-worker about the incident, while 32.7 stated they did not speak with anyone. 17.3 percent did not speak with anyone. If they did not confront the person, 73.8 % stated it was because they felt it would make the situation worse. The following actions did occur because of horizontal hostility: I have muddled through patient procedures that I felt unsure about, I have used a piece of medical equipment I am unfamiliar with because I did not want to ask for help, I have lifted or ambulated a person that was two assist by myself, I have given medication without getting a physician clarification order, I have interpreted an unreadable error instead of calling for clarification, I have held medication and waited to the next shift to ask questions and verify, and I have carried out an order that I did not feel was in the best interest of my patient but did not clarify it. These results were choosing all that apply. What is the clinical significance of the results? The clinical significance of this study is that it will allow hospitals to see how horizontal hostility is making nurses seek other employment and BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 79 therefore losing staff and costing their facilities money. They may also see that it is a factor in nurses leaving the profession. Applicability: It is applicable to hospitals only. Further studies would need to be done in order assess other areas of horizontal hostility in healthcare that are not in an acute care setting. Studies would have to be repeated in other hospitals of differing sizes and populations. Overall Comments on validity and reliability: The overall validity and reliability was sound. There are still many unanswered questions since many nurses chose to fill out the survey with the option, “I choose not to answer this question.” The results would be more relevant if the data had been more focused without this option for people filling out the survey to choose. BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY Appendix C Matrix 80 BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 81 MATRIX TABLES FOR A QUALITATIVE OR QUANTITATIVE ARTICLE Article, Level of Evidence, PICO(T) Chipps, E., Stelmaschuk, S., Albert, N. M., Bernhard, L., & Holloman, C. (2013). Workplace bullying in the OR: Results of a descriptive study. AORN Journal, 98(5), 479-493. http://dx.doi.org /10.1016/j.aorn. 2013.08.015 Purpose, Framework, Design The study sought to describe the incidence of workplace bullying among perioperative RNs, surgical technologists, and unlicensed perioperative personnel at two academic medical centers and determine (a) whether the demographic variables of gender, ethnicity, Level VIhospital, years of Descriptive experience on the Study unit, years in the profession, and In the job title predict perioperative the experience of setting, what is workplace the prevalence bullying, (b) and what are the whether a predictors of relationship exists workplace between bullying, and is workplace there a bullying and relationship emotional between exhaustion, and bullying (c) whether behavior and bullying is emotional associated with exhaustion, and perceptions of bullying patient safety in behavior and the operating perceptions of room (OR). Measurement Tools Sample & Size Results of Research Comments Negative Acts QuestionnaireRevised (NAQR)- 22 items. Cronbach alpha scores ranging from 0.81 to 0.92 The sample included registered nurses, surgical techs, and unlicensed personnel working in the operating room at two academic Magnet status hospitals. The study found that approximately one-third of participants indicated being targets of workplace bullying; 59% had witnessed coworkers being bullied. Perpetrators of bullying are broken down as follows: Other employees on unit 56%, RNs on their unit 56%, Physicians 44%, RN managers 33%, and Charge RNs 11%. A significant moderate, positive correlation among bullying frequency (rho .56, P < .001), bullying intensity (rho .54, P < .001), and emotional exhaustion exists. There is a moderate, negative The study results provide meaningful information in helping to answer the PICO(T) question posed by the authors. The eight negative acts that were associated with perceived compromises in patient safety support an association between behaviors that undermine a culture of safety in the workplace and a perception that patient safety outcomes are negatively affected. There were no statistics in the study that reflect what patient safety outcomes are affected, but there is simply a perception that they are being affected. The study does not distinguish whether the patients receiving *Nine item Emotional Exhaustion Subscale of the Maslach Burnout Inventory (MBI) Seven point Likert scale 0-6, never to daily, scores split and coded into 0-16-low, 17-26moderate, 27 or more-high. Cronbach alpha score 0.91. *23 additional questions including eight demographic questions, eight questions related to bullying experiences and witnessing bullying behaviors at (N = 167). BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY patient safety? This study used a model of bullying from Hutchinson et al. In this model, “organizational antecedents” must be present for bullying to exist in the work environment. Design used was a cross-sectional survey work, and seven questions about the effect of bullying on near errors, errors, expectations, and safety of patients. Nurse experts, clinical nurse specialists, nurse administrators, and staff nurses reviewed questions for clarity. 82 correlation surgical services among bullying are inpatient or frequency (rho outpatient. The e.31, P < .001), evidence is a bullying Level VIintensity (rho Descriptive study. .29; P < .001), It is useful in and job providing satisfaction. 3% information indicated that regarding bullying affected operating room errors and culture which can perceptions of impact patient hospitalized satisfaction. 6% patients. Due to indicated that the single nature bullying affected of the study, it patient safety. cannot be Eight negative generalized to a acts were larger or different associated with population such perceived as acute care compromises in patients and patient safety further research is outcomes; warranted in impossible order to deadlines (odds generalize these ratio 2.4 [95% particular CI, 1.4-4.0]), research findings. having opinions ignored (odds ratio 2.3 [95% CI, 1.4-3.7]), having false allegations made (odds ratio 2.0 [95% CI 1.23.3]), excessive monitoring of work (odds ratio 2.0 [95% CI, 1.2-3.1]), hints from others that the respondent should quit his or her job (odds BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 83 ratio 1.9, [95% CI, 1.0-3.5]), being reminded of errors or mistakes (odds ratio 1.8 [95% CI, 1.1-3.0]), being humiliated at work (odds ratio 1.8 [95% CI, 1.1-3.0]), and being the target of practical jokes (odds ratio 1.7 [95% CI, 1.12.8]). Flynn, L., Liang, Y., Dickson, G. L., Xie, M., & Suh, D. (2012). Nurses' practice environments, error interception practices, and inpatient medication errors. Journal of Nursing Scholarship, 44 (2), 180-186. doi:10.1111/j.1 5475069.2012.0144 3.x To determine the relationships among characteristics of the nursing practice environment, nurse staffing levels, nurses’ error interception practices, and rate of nonintercepted medication errors in acute care hospitals. Reason’s error theory The Nursing Organization and Level IV- single Outcomes Modelobservational link between the study presence of characteristics in Is there a the environment relationship that support between professional characteristics nursing practice PES-NWI- 30 items of the Practice Environment Scale of the Nursing Work Index-Construct validity and reliability proven through previous and current studies. Four item scale of interception practices Validity and reliability is inferred based on rigor of study methods. Appraisal tool indicated reasonable validity and reliability. Survey participants were registered nurses employed in a position of staff nurse on their unit. Exclusionfloat staff not included. N = 686. Mean response rate was 96%. A supportive practice environment was positively correlated with error interception practices among nurses in the sample of medical-surgical units. Nurse interception practices were inversely associated with medication error rates. Nurses’ interception practices [(−0.19, 0.08, 73.98, −2.48, .015)]. Nursing practice environment [(−0.26, 0.30, 79.95, −0.87, .388)]. The study addresses the issue that if there is a positive, supportive work environment, medication errors are decreased. This does pertain to the PICO(T) question posed in this research. It does not further address how medication interception and errors are affected by a work environment in which behaviors that undermine a culture of patient safety are present. A significant feature of this study is it measures actual patient safety instead of BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY of the nursing practice environment, nurse staffing levels, and nurses’ error interception practices, and rate of nonintercepted medication errors in acute care hospitals? and positive patient outcomes. Laschinger, H. K. (2014). Impact of workplace mistreatment on patient safety risk and nurseassessed patient outcomes. Jour nal of Nursing Administration, 44(5), 284-290. doi:10.1097/NN A.00000000000 00068 The purpose of this study was “to investigate the impact of subtle forms of workplace mistreatment on Canadian nurses’ perceptions of patient safety risk and, ultimately nurse-assessed quality and prevalence of adverse events” (Laschinger, 2014, p. 284). Level IVSingle observational study Does the presence of subtle workplace bullying and incivility affect nurse perceptions of patient safety? 84 perceived patient safety as in other studies Limitations of using incident reports for data collection and the well documented underreporting of medication errors or near misses The study design is single observational. Concept of workplace bullying of Einarsen and Mikkelsen, Construct of workplace incivility of Andersson and Pearson Study DesignCorrelational NAQ-R Negative Acts Questionnaire Revised, Cortina’s Workplace Incivility Scale, 5-point Likert scale for perceptions of the effects of negative interpersonal interactions in the workplace, Sochalski Scale 0-4 rating nurses perceptions of the frequency of common adverse patient outcomes over the past year, Aiken et al 1-4 rating the quality of care of their unit. Cronbach’s a reliability was noted to be InclusionOntario hospital nurses on College of Provincial registry list. Sample size is 641 with a response rate of 52%. Responders were 88.7% women, 60.7 baccalaureate prepared, 69% full time, and 78.3% acute care. Bullying and all sources on incivility were significantly related to nurseassessed quality of care, adverse events, and perceptions of patient safety risk. Patient/family complaints were the individual adverse event most strongly related to bullying and physician and coworker incivility. Nurse assessed patient safety risks are as follows; Patient care quality and physician incivility (B= 0.234, p< .05), Bullying and overall frequency of The data supports a positive correlation between behaviors that undermine a culture of safety and adverse patient safety events. The events in this study are measured by nurse assessment and not by number of occurrences. Adverse events are not broken down into categories but instead labeled patient adverse events and patient care quality. This particular study shows that there is a stronger positive correlation between bullying and patient BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY excellent for the Negative Acts Questionnaire, noted as .89 and .81 for Cortina’s, and reliability/validi ty statements are made regarding Sochalski’s and Aiken’s tools, and more softly for the items related to patient safety risk. Roche, M., Purpose-Rate Diers, D., nurses’ Duffield, C., & perception of Catling-Paull, violence in C. (2010). medical-surgical Violence toward units and relate nurses, the work this to patient environment outcomes. and patient outcomes. The The conceptual Journal of framework 49 item Nursing Work IndexRevised Environmental Complexity Scale 11 question nursing intervention questionnaire about 94 randomly selected medical surgical wards in 21 public hospitals across two states in Australia. ED’s, ICU’s, 85 patient adverse adverse events events (B= than physician 0.241, p< .05), incivility or coPhysician worker incivility incivility and and patient overall adverse events. frequency of There are patient adverse limitations to this events (B= study since cross0.166, p< .05), sectional data was Coworker used and incivility (B= precludes 0.148, p< .05). attribution of Workplace cause and effect mistreatment as among the study related to patient variables. The safety is as low questionnaire follows; response rate and Bullying B= targeted sample 0.328), Physician limit incivility B= generalizability 0.228. and patient outcomes were nurse-assessed not institutional data. This is applicable to the authors’ PICO(T) question as it shows a positive correlation between bullying and incivility and adverse patient outcomes. As ward The study results environments are relevant in becomes less helping to answer stable (fewer the PICO(T) RN’s, increased question. The workload, study shows a unanticipated positive changes in correlation patient status, between various perceived low forms of nurse leadership, workplace BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY Nursing Scholarship, 42(1), 13-22. Doi: 10:1111/j.15475069.2009.0132 1.x Single correlational/ob servational study-Level IV How do nurses’ self-rated perceptions of violence (emotional abuse, threat, or actual violence) on medicalsurgical units affect the nursing working environment and patient outcomes. included concepts of nursing resources, workload, the working environment and patient outcomes without predictions of specific links. Design- Cross sectional collection of data by surveys and primary collection of unit data for 1 week periods interventions that were delayed or not done. Staffing matrix of the institutions PRN-80 Patient acuity scale Correlation analysis was conducted and P values were given. EN, enrolled nurse, registered nurse, autonomy, nurse-doctor relations, leadership, environmental complexity, unanticipated changes in acuity, nursing hours of care required per patient/nurse hours per patient day: p<.05. Pediatrics, Obstetrics, and Psychiatric units were excluded. Random selection used. All nurses on the floor were asked to complete survey including clinical nurse specialists, registered nurses, enrolled nurses, certified nursing assistants, and training nurses were polled. Target sample was 3,099 nurses with an 80.3% response rate. (N = 2,487) RN’s made up 72.3% of respondents. 86 low nurse autonomy, poor relationships with physicians, patients awaiting placement), perceived violence increases. Correlation of Patient Adverse Events per Ward and Nurses Experiencing Physical Violence and Threat of Violence; Patient falls (0.21, 0.19), Medication errors (0.22, 0.22), Delays in medication administration (0.15, 0.10). Out of 947 nurses that reported emotional abuse, 14.7% stated that they had received emotional abuse from a nursing co-worker and 9.8% polled that they had received emotional abuse from more than one source. violence and threats of violence, and adverse patient safety events. The physical and threat of violence in this article is nurse perceived but the actual patient safety outcomes are measured by occurrence through primary data collection. The study was limited by selfreporting of violence and assessment of tasks not done or delayed. Unitlevel primary data collection was limited by a 7-day collection period which may have resulted in missing some instances of falls or medication errors. Patient adverse outcome rates were very low which limited statistical power. Study results lend emphasis regarding a positive correlation between behaviors that undermine a culture of safety BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY Walrath, J. M., Dang, D., & Nyberg, D. (2013). An organizational assessment of disruptive clinician behavior: Findings and implications. Journal of Nursing Care Quality, 28(2), 110-121. doi:10.1097/NC Q.0b013e31827 0d2ba Single Correlational Study –Level IV How does disruptive behavior in a large academic medical center affect (a) type, frequency and scope of clinicians’ personal experience with disruptive behavior and what impact does it have on staff, patients, and the organization (b) The purpose of the study was to understand the complexities of disruptive behavior in a large academic medical center. The objectives were to (a) determine the type, frequency, and scope of clinicians’ personal experiences with disruptive behavior and impact on staff, patients, and the organization; (b) compare disruptive behavior experiences of RNs and MDs; (c) customize interventions for RNs, MDs, interprofessional teams, and the organization to foster culture change and enhance patient safety. Johns Hopkins Model for Disruptive Clinical Behavior, This Disruptive Clinician Survey for Hospital Settings: Survey items included dichotomous, 4 and 5-point Likert scales, and multiple choice patterns which were answered based on their personal experiences “during the past year”. Total study population: Clinicians in one urban academic medical center in the mid-Atlantic region of the United States (N = 5710). Three clinician groups: (a) all levels of clinical and administrativ e RNs (n = 2759); (b) nurse practitioners, certified nurse midwives, certified RN anesthetists, and physician assistants (n = 470); (c) full time School of Medicine clinical faculty, fellows, and house staff MDs (n = 2481). Nurses and MDs in all practice 87 and adverse patient outcomes in acute care settings. 84% of The study results respondents will help answer reported the PICO(T) personally question under experiencing investigation. disruptive This study behavior during continues to show the past year. a positive 73% of correlation respondents between reported disruptive observing a behaviors and coworker who adverse patient was a target of outcomes. This this behavior. particular study RNs experienced shows that a significantly disruptive higher frequency behavior is of disruptive prompted by behaviors and organizational triggers than triggers that can MDs; 45% of then lead to MDs and 37% of negative patient RNs reported outcomes. These that their peer’s results are disruptive mirrored in the behavior affected Roche, Diers, them most Duffield, & negatively. Catling-Paull, Disruptive (2010) article behavior was which indicates reported more that perceptions frequently within of violence were the MD staff related to adverse (45.1% in patient outcomes comparison to through unstable 36.5% among or negative RN staff) and the qualities of the affiliates work reported MDs as environment. The having the most sample size is negative impact. comparatively BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY what are the disruptive behavior experiences of RNs and MDs, and (c) what interventions are there for RNs, MDs, interprofessiona l teams and the organization to foster culture change and enhance patient safety. model explains disruptive behavior using 4 concepts: triggers, disruptive behaviors, responses, and impacts. Disruptive behavior is defined as “personal conduct, whether verbal or physical, that negatively affects or potentially may affect patient care including, but not limited to, conduct that interferes with one’s ability to work with the other members of the healthcare team.” The survey instrument subsequently developed and used in this study was guided by this conceptual model. DesignDescriptive survey-Follow up to previous study. settings were included. Response rate = 27.3%. (N = 1559); 35.8% (n = 987) RNs; 20% (n = 496) MDs; 16.2% (n = 76) affiliates. Most RNs and affiliates (89.3%) = female; most MDs (60.9%) = male. 88 Most prominent large in this study trigger for both although a MDs and RNs response rate of was 27.3%, lack of organizational in data on nonnature - pressure responders, and from high potential that census, volume, responders were and patient flow. victims of 189 incidences disruptive of patient harm behavior raise related to into question disruptive possible selection behavior were bias and reported by representativeness study of the results. participants. Of Generalizability the 189 reported is limited due to incidents of one study setting harm, 77.2% but similar were rated as structures and temporary processes in most (requiring hospitals allows treatment or consideration for intervention, or applicability in prolonged other than hospitalization), academic hospital 10% permanent settings. There is (wrong no further procedure or narrowing of the wrong site categories. surgery), and 12.7% requiring life-sustaining interventions (intubation or emergency surgery). Contrary to previous findings that indicate intimidation is a barrier to reporting, this study indicated that clinicians BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 89 speak-up and do not let disruptive behavior get in the way of patient care or reporting of deterioration; the authors acknowledge the possibility that due to the sensitivity of this item, participants sacrificed the accuracy of their responses in favor of one that would be perceived as more socially acceptable. Wilson, B.L. & Phelps, C. (2013). Horizontal hostility: A threat to patient safety. JONA’S Healthcare Law, Ethics, and Regulation, 15(1), 51-57. doi:10.1097/NH L0b013e318286 1503 Single observational study Level IV In a 220-bed community hospital in the Southwest, what is the Purpose: The purpose of this study is: (a) determine the degree of perceived hostility in a 220 bed hospital; (b) determine the degree of RN-toRN and physician-to-RN hostility; (c) determine how perceived hostility influences nurse’s behaviors directly related to patient care. Design- Cross sectional survey Ordered and dichotomous 28 item survey to determine the level of perceived horizontal hostility (HH) in an acute care Magnetaspiring hospital and nurse actions as a result of that experience. The survey was modeled on contents is a previous study from the American Association of Critical Care entitled “Seven Surveys were given to all five hundred nurses working in a 220-bed hospital during a 2 month period; response rate was 26% (N = 130). Respondents were as follows: 10 years’ experience= 58%, baccalaureate degree= 58%, female = 90%, 30-39 60% (n=78) of respondents reported observing HH at least monthly, with the majority of respondents reporting they witnessed hostile behaviors weekly. The top answer regarding the category of coworker observed exhibiting HH toward another person was “a nurse from my unit” (n=66), followed by a physician (n=53). Of those who answered The research for this article shows that nurses experience horizontal violence in the workplace (60%). The article addresses nurse care behaviors that result because of horizontal violence that could contribute to adverse patient outcomes. Numbers of behaviors potentially compromising patient safety are not provided; options had a BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY degree of perceived hostility in the workplace, and (if present) to what to extent that horizontal hostility behaviors from either RN-toRN or physician-toRN influenced nurse behaviors directly related to patient care? Crucial Conversations in Healthcare” and the survey by Stanley et al. entitled “Lateral Violence in Nursing Survey”. years old= 23.3%, 40-49 years old= 35.3% 50 and older= 31.5%. 90 this question, 58% (n=60) stated they spoke with a peer or coworker about perceived HH; 17.3% (n=18) stated they had addressed the perpetrator directly to fully express their concerns. The most common reason people gave as the reason for failure to confront horizontal hostility was that it would make their work situation worse, followed by fear of retaliation. Respondents reported the following actions because of horizontal hostility: I have muddled through patient procedures that I felt unsure about, I have used a piece of medical equipment I am unfamiliar with because I did not want to ask for help, I have lifted or ambulated a person that was two assist by “select all that apply” instruction on the questionnaire. The sample size is relatively small. This article supports the PICO(T) question under study as it shows how HH can potentially lead to adverse patient events through the effect on nurse care behaviors. A major limitation to this study was the number of respondents who selected the “choose not to answer” option for several of the study variables which significantly limited the kinds of analysis that could be done. For example, because many nurses did not want to identify their unit, adverse events by unit in relation to levels of perceived hostility could not be examined due to insufficient statistical power. Asking for home BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 91 myself, I have given medication without getting a physician clarification order, I have interpreted an unreadable error instead of calling for clarification, I have held medication and waited to the next shift to ask questions and verify, and I have carried out an order that I did not feel was in the best interest of my patient but did not clarify it. unit identification points to a potential study design flaw which should be considered in future research efforts. Comments QUALITATIVE Article, Level of Evidence, PICO(T) Purpose, Framework, Design Walrath, J. M., The purpose of Dang, D., & the study was to Nyberg, D conduct focus (2010). Hospital groups with RNs RNs’ to gain an experiences understanding of with disruptive how RNs describe behavior: A disruptive qualitative clinician behavior study. Journal and its impact of Nursing Care based their Quality, 25(2), observed and 105-116. actual doi:10.1097/NC experiences on Q.0b013e3181c the front lines of Data Collection and Analyzing Sample & Size Results of Research IRB approval and oral consent from participants obtained. A clinical psychologist external to the organization facilitated 90minute focus group sessions, using semi structured interview Purposive convenience sampling of 96 RNs in an acute care hospital within an academic medical center located in the Northeastern United States. The recruitment Participants reported the occurrence of disruptive behaviors in all practice settings and between /among a wide variety of healthcare personnel. 168 different disruptive behaviors were identified and This article assists with answering the PICO(T) question under examination. It further categorizes the disruptive behavior experienced in the workplace. While there is no further information in the study that addresses patient specific outcomes, the study highlights nurses’ BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY 7b58e Single Qualitative Study-Level VI What are RNs’ perceptions regarding the characteristics of clinician disruptive behavior and what is the perceived impact based on their observed and actual experiences in a patient care setting? patient care delivery. questions based on the conceptual Disruptive framework. behavior is a Focus group complex size was from 7 construct and full to 14 RNs. understanding Pseudo names requires were used when examination of describing causes, individual individuals responses, effects involved in on individuals disruptive and organizations, behavior events and perceptions to ensure of harm to confidentiality patients. Because of sensitive the researchers information. found no The sessions conceptual were audioframework that recorded and included these held between interrelated January and concepts in a March 2008. meaningful way, The recorded the researchers sessions were adapted Pearson recorded and colleagues’ verbatim and framework on validated for workplace accuracy incivility and against the developed a original framework for recordings. organizing and Nudist6 describing software disruptive program behavior, which designed for included 4 narrative primary concepts: analysis was triggers, used to manage disruptive the interview behaviors, data and responses, and facilitate the impacts. coding process. Design: Deductive and Descriptive inductive process invited participation through information of the study distributed across the Department of Nursing via posters, internal Web sites, and individual letters to RNs (N = 2467). 32.3% of participants were nurse managers and shift coordinators; 52% were staff nurses; 15.6% were advanced practice nurses. 95% of participants were female. 70.8% were white; 12.5% were Asian; 9% were black; 3.1% were Hispanic/Lati no 92 then synthesized into 21 categories. Within these categories, 3 themes emerged: incivility, psychological aggression, and violence. The 10 most frequently identified categories within these themes were rude/disrespectfu l (= Incivility); engaging in gossip, intimidation/thre ats, passive aggressive behavior, refusal to do one’s job, verbal aggression, power play, condescending language/dress down, professional disregard ( = psychological aggression); and physical violence (= violence). Out of the personal experiences reported, 225 disruptive behavior events were coded. Physicians were identified as instigators in 42% of events; perceptions that patient safety is potentially compromised by disruptive behavior. The study would increase in evidence level if the responses were measured using quantitative methods and be more universal if a larger sample size was used, presenting opportunities in future studies. The information obtained from this research article mimics (corrected spelling) or you can say “is in alignment with information found in other…” the information found in other articles that indicate lateral violence is experienced by a majority of healthcare workers and has a potentially negative impact on patient outcomes. A 3.9% response rate and the potential that participants were victims of disruptive behavior and were ready to share their experiences raises the possibility of selection bias and BEHAVIORS THAT UNDERMINE A CULTURE OF SAFETY qualitative study – no specified tradition processes were used to ode the data. Two members of the research team independently assigned codes to text segments of the transcribed interviews. After reaching consensus on the codes through comparison and discussion, the full research team was convened to review, identify patterns, and synthesize the initial codes into broader categories were further synthesized into major themes and organized according to the four primary concepts in the conceptual framework. 93 nurses in 29% of events; support personnel in 27% of events; and management in 2% of events. Triggers, RN responses, and impacts on the RN, patient, and the nurse practice setting were also identified. Distraction from patient care, physical and emotional distress, and priority conflicts between patient care and operational needs were described by the participants. Concerns regarding a decrease in quality care, increased risk to patient safety, care delivery delays, and disrupted working relationships were also described. may not represent the experiences in other hospital settings. Despite the limitations, the study provides insight into the disruptive behavior construct and provides direction for future inquiry of disruptive behavior in acute care settings. The authors subsequently followed up this study with a quantitative study (see Walrath, Dang, and Nyberg 2013)