like to - My Illinois State
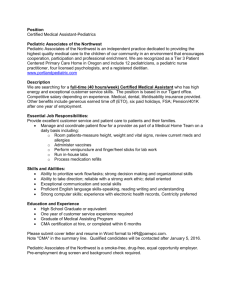
advertisement

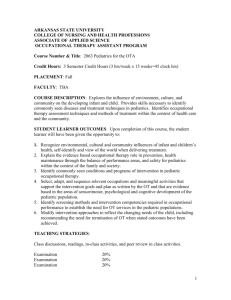
Pediatric assessment 1 MENNONITE COLLEGE OF NURSING AT ILLINOIS STATE UNIVERSITY Diagnostic Reasoning for Advanced Practice Nursing 431 Assessing Children: Infancy through Adolescence Difference between pediatric and adult examination With Pediatric assessment the approach to the patient and the sequence of the exam differ according to the child’s age and developmental level Types of visits: Complete (head-to-toe) o New to the practice o Regular health maintenance visits o School physicals o Sports physicals Focused – concentrates on chief complaint and includes a focused history Child development Predictable pathway governed by maturing brain o Cephalocaudal – head to foot development; examples are brain/head development earlier coordination than in arms and legs; head larger relative to rest of body o Proximodistal – central to peripheral development; examples are brain/spinal cord in trunk develop before arms and legs; motor control of trunk and head before arms and legs Characterized development as normal or abnormal based on achievement of age-specific milestones Affected by physical, social, and environmental factors, as well as diseases o Chronic illness o Child abuse o Poverty Child’s developmental level affects how you conduct the medical history and physical examination Focus on Pediatric Health Promotion: Key Components Age-appropriate developmental achievement of the child o Physical o Motor (gross and fine motor skills) o Cognitive o Emotional o Social Health supervision visits (periodic assessment of medical and oral health) Integration of physical exam findings with health lifestyles Immunizations – see CDC site for latest recommendations Screening procedures o Growth parameters o Developmental screenings (DDST) – early detection/intervention o B/P, vision, hearing o High-risk patients; testing for lead poisoning, TB exposure, anemia, cholesterol, UTIs and STDs Anticipatory guidance Pediatric assessment History Approach the family and child Family-centered approach Address the parent & child’s concerns Realistic recognition of limitations in self, patient, time, and environment Effective planned use of time Communication skills Boost self-esteem of child Enhance sense of parents confidence Consider the family as partners in problem solving o Explore family’s value system o Use the families resources o Respect family’s agenda and solutions o Respect family needs, expectations, concerns and resource limitations Be open-ended Be non-judgmental Make advise finite, practical, and concrete Have FUN with the child and family Gathering Information/History (see Bright Futures website for visit templates at http://brightfutures.aap.org/tool_and_resource_kit.html) Parent or guardian needs to accompany the child to the visit unless documentation from responsible party that indicates another adult has permission to make health care decisions! A. Chief Complaint - reason for visit B. History of Present Illness: OLDCART C. Past Medical History (pregnancy, birth, newborn→ current age, illness, accident, preventative care) a. Perinatal i. Mother’s general health during pregnancy; 1. Complications of pregnancy - bleeding, falls, swelling of hands and feet, high blood pressure, unusual weight gain, substance abuse, medications during pregnancy 2. Ultrasound results or genetic testing results 3. Emotional status, during pregnancy and post-partum ii. Pregnancy history; Para, Gravida, Abortions, Miscarriages iii. Planned pregnancy? iv. Father’s attitude b. Labor & Delivery i. Date, Place of birth ii. Complications iii. Anesthesia used iv. Type of delivery c. Newborn (first 28 days) i. Gestation ii. Weight iii. Length iv. Apgars v. Nutrition vi. Sleep 2 Pediatric assessment vii. viii. ix. x. xi. xii. xiii. xiv. d. Infant i. 3 Elimination Growth and development Hospitalizations; ER or Urgent care visits Surgeries Illness Immunizations Allergies Medications Key areas – nutrition, sleep, elimination, dentition, illness, hospitalization, surgery, accidents, immunizations, growth and development, allergies, medications, habits ii. Informant is the parent or guardian e. School-age i. Key additional areas – family, friends, school, activities ii. Interview parent and child f. Adolescent – Key principles of interviewing i. Adolescent is primary informant, interview alone ii. Discuss findings and recommendations with parents iii. Confidentiality must be ensured, explain to adolescent and parent that unless serious problems emerge that is a threat to teen’s life or health, interview with adolescent will be strictly confidential iv. Use HEADSS interview approach (Home, Education, Activities, Drugs, Sex, and Suicide) D. Family History (developmental, personal and social) a. Composition of household b. Health of family members; heart problems, cancer, developmental delays, learning problems, genetic disorders, asthma, allergies, seizure disorders, hypertension, sickle cell anemia, blindness, endocrine disorders, kidney disorders, birth defects, infant deaths c. Marital status, educational background, and occupation of parents d. Outcomes of any previous pregnancies e. Availability and nature of support for the family E. Social History a. Living situation – including sleeping arrangement b. Who is in the home and any smoking, use of alcohol, firearms, safety issues, etc? c. Who is the primary care giver and other care givers - daycare F. Review of Systems a. All systems - age appropriate questions and much shorter b. Focus will vary a bit by age, should include nutrition, elimination, sleep, behavior, physical activity, growth & development, school, and home Areas of Physical examination • Physical development – Assessed in depth at each visit • Cognitive development – Assessed generally at each visit • Social and emotional development – Assessed generally at each visit – Observe parent-child interaction – evidence of mutuality and reciprocity – Behavioral assessment Pediatric assessment 4 Stages of Development • Newborn (birth) • Infancy (0 to 12 months) • Early childhood (1 to 4 years) • Middle childhood (5 to 10 years) • Adolescence (11 to 20 years) – Early – Middle – Late Vital Signs Throughout Development (important to know normal ranges and evaluate each visit) • Height – at birth & every visit – plot on growth chart • Weight – at birth & every visit – plot on growth chart – Calculate BMI (body mass index) at every visit & plot on growth chart • Head circumference – birth to 36 months & plot on growth chart • Blood pressure – start measuring at age 2, unless CVD • Pulse – higher in infancy; slows down with aging • Respiratory rate – higher in infancy; slows down with aging • Temperature – < 2 months of age: rectal temperature – > = 2 months of age: tympanic temperature Newborn Assessment • General assessment – Apgar score • Sequence of examination: – Careful observation of activity – Head, neck, heart, lungs, abdomen, genitourinary system – Lower extremities, back – Ears, mouth – Eyes whenever they open spontaneously • Skin (throughout the exam) o Vernix caseosa: present at birth o Lanugo: shed within the first few weeks of life o Meconium staining o Texture o Color – cyanosis, jaundice, pink, pale o Lesions Secondary to trauma - forceps marks, subcutaneous fat necrosis, sucking blisters, scalp Vascular – nevus simplex, port wine nevus, strawberry hemangioma, cavernous hemangioma Infectious lesions – Candida diaper dermatitis, Herpes • Head and Neck o Head and face shape, circumference, symmetry; molding, caput succedaneum (edema crosses suture lines), cephalhematoma o Suture lines, anterior and posterior fontanelles o Neck mobility, torticollis, length, webbing o Dislocation of clavicle • Nose and Mouth o Nasal patency, discharge, sneezing, flaring, flattened nasal bridge Pediatric assessment • • • • • • • • • 5 o Palate intact, uvula midline, frenulum of tongue and upper lip, Epstein pearls, thrush (candidiasis) o Reflexes; gag, sucking, rooting o Vigorous cry, receding chin Ears and auditory o Symmetry, shape, position o Preauricular sinus, preauricular skin tag, poorly formed helix, malformed ear, low placed ears o Startle reflex to noises Eyes o Red light reflex, nasolacrimal duct patency o Blink reflex, rudimentary fixation on objects and ability to follow to midline o Epicanthal folds, nystagmus or strabismus, scleral hemorrhages Chest and Lungs o AP and lateral diameters equal, pectus excavatum (funnel chest), pectus carinatum (pigeon chest) o Breasts – enlargement, secretion, supernumerary nipples o Respirations primarily abdominal, cough reflex Heart o Apex – 4th to 5th intercostal space, lateral to left sternal border o S2 slightly sharper and higher in pitch than S1 o Check for murmurs and coarctation of aorta (check pulses) Abdomen o Cylindrical shape - abdominal masses, hepatosplenomegaly, diastasis recti o Liver palpable 2-3 cm below right costal margin o Kidney palpable 1-2 cm above umbilicus o Umbilical cord (AVA), umbilical hernia GU o Male – testes palpable in scrotum, penis, smegma, urethral opening at tip of glans penis, hypospadias, inguinal hernia, hydrocele o Female – labia majoria and clitoris usually edematous, vernix caseosa between labia, patency of vagina, ambiguous o Urinates in 24 hours o Anus patent, anal wink, meconium within 36 hours Neuromuscular o Spine intact, no openings or masses o Check for hip dislocation o Reflexes; Moro and Plantar (up going toes until about 18 months) Extremities o 10 fingers and toes, ROM, symmetry, pulses, syndactyly (webbing/fused toes), polydactyly (extra digits) Reflexes o Blinking, pupillary, doll’s eyes o Sneeze, Glabellar (touch middle of forehead and eyes close) o Sucking, gag, rooting, extrusion, yawn, cough o Grasp, plantar, ankle clonus, Moro, startle, Perez, tonic neck, Galant, step, crawling, placing Pediatric assessment 6 General Assessment of a child (as appropriate for developmental stage) • General appearance - facies, posture, hygiene, nutrition, behavior, development, state of awareness • Skin, hair, nails, lymph nodes, head, neck, trachea, thyroid, carotid arteries • Eyes – Palpebral slant, Epicanthal fold, lids, pupils, lens, fundus, corneal light reflex, cover test, alternate cover test, peripheral vision, color vision-Ishihara or Hardy-Reand Rittler test • Ears – o Until age 3 insert speculum between 3 and 9 o’clock position in a downward and forward slant, pull pinna down and back to the 6 and 9 o’clock range o Over age 3 pull pinna up and back toward a 10 o’clock position o Rinne test o Weber test • Nose, mouth, throat. Lungs • Heart o Aortic area – 2nd ICS right sternum o Pulmonic area – 2nd ICS left sternum o Erb point – 2nd and 3rd left ICS sternum o Tricuspid area – 5th right and left ICS sternum o Mitral area – 5th ICS, left MCL • Abdomen, genitalia • Back and extremities o Assess gait o Genu valgum (knock-knees) from 18 months to 4 years of age o Genu varum (bowleg) o Pes planus (flat foot) – normal finding in infancy, may be a result of muscular weakness in older child o Pes valgus – eversion of entire foot, sole rests on ground o Pes varus – inversion of entire foot, sole rests on ground o Metatarsus valgus – eversion of forefoot, heel remains straight (toeing out or duck walk) o Talipes valgus – eversion (turning outward of foot, inner side of foot rests on ground) o Talipes varus – inversion (turning inward of foot, outer side of foot rests on ground) o Talipes equines – extension or plantar flexion of foot, ball and toes rest on ground, commonly occurs with talipes varus (most common club foot deformity) o Talipes calcareous – dorsal flexion of foot, heel rest on ground • Neuro o Mental status o Cranial nerves o Motor function (finger-nose-finger, heel-to-shin, Romberg test, touch tip of finger to thumb) o Reflexes o Sensory – vision and hearing Infancy: 28 days to 12 months • Most rapid rate of growth – Birth weight triples, height increases by 50% by the end of year one • Sequence of examination – Perform non-disturbing maneuvers early – Perform potentially distressing maneuvers near the end; e.g., ears, mouth, and abdomen – If quiet listen to heart, lungs, abdomen, then reflexes; perform traumatic procedure and Moro reflex last Pediatric assessment • • • • • • • Tips for Examining an Infant – Use a reassuring voice throughout the examination – Let the child see and touch the examination tools you will be using – Avoid asking permission to examine a body part because you will do the examination anyway; instead, ask the child which body part he or she would like to have examined first – Examine the child in the parent’s lap around 4-6 months – Allow the parent to undress the child; leave in diaper – If unable to console the child, allow a short break – Make a game out of the examination Head – Inspect for symmetry, shape, circumference (look from above) – Palpate: o Anterior fontanelle – closes between 4 and 26 months of age o Posterior fontanelle – closes by 2 months of age Eyes: – Inspect sclera, pupils, irises, extraocular movements, and presence of red reflex Ears: – Inspect position, shape, landmarks, patency of ear canal Acoustic blink reflex Nose and paranasal sinuses: – Infants are obligate nasal breathers for first the 2 months of life – Only the ethmoid sinuses are present at birth – Inspect for position of nasal septum Mouth/pharynx: – Inspect mucosa, tongue, gums, palate, uvula, tonsils, and posterior pharynx – Palpate gums and teeth o Teeth: 6 to 26 months of age, 1 tooth per month o Central and lateral incisors erupt first, molars last – Reflexes – gag, sucking, rooting Neck: – Inspect for masses – Palpate for presence of adenopathy: unusual in infancy 7 Pediatric assessment 8 Question A mother presents to the pediatrician concerned that her 8-month-old child is not developing appropriately. She bases this concern on the fact that the posterior fontanelle closed 6 months ago, but the anterior fontanelle is still open and soft. Your response to this concern is based on which fact? a. The anterior fontanelle closes between 4 to 26 months of age b. Both fontanelles should close within 2 to 4 months of each other c. The posterior fontanelle has closed early d. None of the above are true Answer – • • • • • • • • Thorax: – Inspect respiratory rate, color, nasal component of breathing, and listen for audible breath sounds – Palpate tactile fremitus if infant is crying or making noise – Percussion is not helpful in infants o Thorax is more rounded in infants than in older children and adults Lungs - auscultation: – Generally, sounds are louder and harsher – Distinguish between upper and lower airway sounds o Upper airway: loud, symmetric transmission throughout the chest - loudest as stethoscope is moved upward; coarse during inspiratory phase o Lower airway: loudest over site of pathology; asymmetric; often has an expiratory phase Heart – Inspect for cyanosis – Palpate: o Peripheral pulses, especially brachial o PMI is not always palpable; 1 interspace higher than in adults o Thrills – Auscultate: o S1, S2 (split is normal but fuse together as single sound during deep expiration) o S3 is frequently heard and is normal o Murmurs – functional murmurs vs. pathologic o Mitral area – 3rd to 4th ICS and lateral to left MCL Breasts – Inspect – Palpate for masses Male genitalia – Inspect – Palpate for descent of testes into scrotal sac Female genitalia – Inspect Abdomen – Inspect – umbilical cord remnant is gone by 2 weeks of age – Auscultate bowel sounds – Palpate - liver edge 1-2 cm below costal margin is normal; palpable spleen tip is normal – Rectal – generally not done Musculoskeletal – Inspect the spine – Palpate the clavicle, hips, legs, and feet Pediatric assessment Barlow’s and Ortolani’s test – identifies unstable hip that lies in the reduced position and can be passively dislocated (see handout) o Bowlegged growth to age 18 months is normal Nervous system – Inspect motor tone – Palpate motor tone through passive ROM of major joints – Normal reflexes o Newborn: Palmar grasp, plantar grasp, Moro reflex, asymmetric tonic neck reflex, positive support reflex, anal reflex, positive plantar o Infancy: Triceps, brachioradialis, and abdominal reflexes present starting at age 6 months o • Early Childhood (1 to 4 years): Physical Examination Features • Rate of growth slows to 50% of that of infancy • Tips for examination sequence: – Toddler o Start with the child seated or standing by the parent o Inspect the body through play o Introduce equipment slowly o Have parents remove outer clothing o Praise for cooperative behavior o Ask the parent for assistance if restraint is needed o First examine the eyes, palpate neck, percuss/auscultate o Move child to supine position – examine abdomen, musculoskeletal, nervous system; examine genitalia last o End the examination with the patient upright; look at the throat and ears – Preschooler o Prefer standing or sitting o Proceed head-to-toe o Request self-undressing o Demonstrate equipment o Give choices when possible; expect cooperation • General appearance – facies, posture, hygiene, nutrition, behavior, development, state of awareness • Early Childhood: Unique Physical Examination Features – Vital signs: o Measure blood pressure starting at age 2 – Neck: o Palpate for lymph nodes; adenopathy is common – Eyes: o Cover and uncover test for position and alignment of eyes – Ears: o Visualization of tympanic membrane is the greatest challenge – Nose/sinuses: o Maxillary sinuses present by age 4 – Heart o Brachial pulses still easier to feel than radial 9 Pediatric assessment – – – 10 Abdomen o Protuberant abdomen still normal o Liver span 1-2 cm below costal margin is still normal o Spleen edge 1-2 cm below costal margin is normal o Use the scratch test to palpate for the liver size Male genitalia: o Testes undescended in scrotal sac by age 1 is abnormal and need to refer Musculoskeletal system: o Inspect spine for scoliosis in any child who can stand Question You enter the room of a 2-year-old female who is visibly upset and afraid of being at the clinic. To facilitate the examination, which of the following actions would be most appropriate? a. Leave the room and return when the child is calm b. Have the parent leave the room since his or her presence is making the “acting out” worse c. Ask the child’s permission to examine a body part d. Examine the child in the parent’s lap Answer – Middle Childhood (5 to 10 years): Physical Examination Unique Features • Tips for examinations – Prefer sitting – Proceed head-to-toe as with adults – Request self-undressing; give gown to wear – Teach about body functions • Nose and paranasal sinuses – Sphenoid sinuses present by age 8 – Frontal sinuses present by age 6-7 • Tonsils – Peak growth is between ages 8-16 years • Breasts – Development in girls is the first sign of puberty; may start as early as age 6 • Musculoskeletal system – Inspect legs and feet – Inspect spine for scoliosis Adolescence: Unique Features • Tips on examination – Offer privacy; give a gown – Emphasize normalcy of development – Examine genitalia as any body part, may leave until end • Assessments – Height, weight, blood pressure, pulse – Vision screen – Hearing screen – Skin – Teeth, gums – Neck – thyromegaly or adenopathy – Abdomen – hepatosplenomegaly – Tanner staging (below) Pediatric assessment • 11 – Breast and testes self-examination – Pelvic exam – Scoliosis screen Puberty – Reproductive physiology • Males may produce sperm before first ejaculation • Males usually are fertile by age 14-15 years • Males are able to cause pregnancy at any time after they begin producing sperm, but have diminished fertility the first 1-2 years • Females may not produce eggs (ovulate) for 1-2 years after menarche • It is impossible to predict which females will be fertile soon after menarche and which may take months to years to become fertile, although earlier menarche is associated with earlier ovulation • Pregnancy is possible whenever there is intercourse • Pregnancy is most likely when intercourse occurs halfway between menstrual periods • The earlier a boy or girl enters puberty, the earlier he/she is likely to be fertile – Major physical events • Gonads and reproductive organs mature and secondary sex characteristics develop (breasts, pubic hair, facial hair, testes, penis, scrotum) • Skeletal growth increases, then slows before finally ceasing (growth spurt) • Alterations of body composition as well as the altered distribution of fat • Increased strength and endurance • Maturation of the anatomic and biochemical factors which coordinate and initiate these processes – Major outcomes o Adult size, shape and appearance o Clear physical distinction between sexes o Ability to reproduce – Features o Sequence of changes is very similar for all persons o May be a wide variation in tempo (when it starts and how long it takes) o Physical changes (secondary sex characteristics, fertility, changes in endocrine glands, brain and body composition) reflex underlying hormonal changes – Typical ages of pubertal events o Start Boys: 11-12 years (range 9-14 years) – testicular growth and pubic hair Girls: 10-11 years (range 8-13 years) – breast development and pubic hair o Growth spurt Boys: 14 years (range 12-16 years) Girls: 12-13 years (range 10-14 years) o Spermarche/menarche Boys: 13-14 years (range 12-16 years) – first ejaculation Girls: 12-13 years (range 10-16 years) – first menstrual period o Length Boys: 3-4 years Girls: 4-5 year – Typical sequence of events o Boys Growth of testicles Pediatric assessment o Girls o o o o o o 12 Pubic hair appears Growth of penis, scrotum Axillary hair 1st ejaculation, growth spurt, facial hair - may occur simultaneously Adult height Breast buds appear or in ½ of girls pubic hair Pubic hair appears and/or growth spurt Pubic hair matures Breast mature Axillary hair Menarche Average age is 12-13 years – signals the end of rapid growth phase Usually occurs 2-3 years after breast development begins Growth rate usually slowing down before menarche Bleeding usually not regular in amount or number of days for first 1-2 years Menarche may be delayed by poor health, intense exercise (athletes), low body weight (anorexics), emotional stress, and poor nutrition o Adult height Pediatric assessment 13 Pediatric assessment • 14 Common concerns about puberty – Beginning late – discuss normal variations or underlying cause – Beginning early – discuss normal variations (more common in girls) and associated stress – Partial early o Premature thelarche – isolated breast development o Premature adrenarche – isolated pubic hair development – Unexpected events o Breast asymmetry in girls o Gynecomastia – breast tissue development in boys (if unilateral check tests due to increase testicular cancer rate) o Excessive or insufficient body hair o Nipple discharge (check prolactin level) – Expected events o Acne o Body odor o Spontaneous erections o Nocturnal emissions o Masturbation o Sexual urges – Typical concerns o “I’m not normal.” o “I don’t look like my friends.” o “I’m too tall, too fat, etc.”