Nervous System - Blog Unsri
advertisement

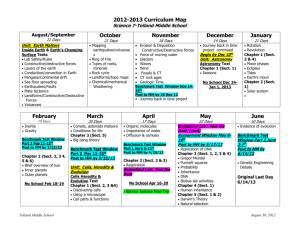
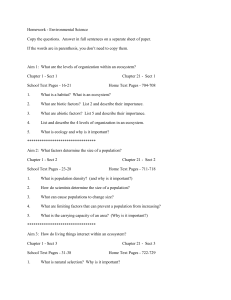
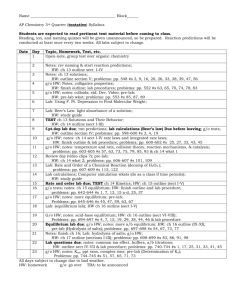
Nervous System dear d34r123@yahoo.co.id KOMUNITAS BLOGGER UNIVERSITAS SRIWIJAYA Clinical Neurology Pathways and tracts - Sensory pathways, prorioception, vibration and crude touch go to the DORSAL COLUMN - Pain, temperature, fine touch cross midline to form SPINOTHALAMIC TRACT - Motor pathways go to the ANTERIOR COLUMN Voluntary command, integrated and delicate skills ran by CORTICOSPINAL TRACT - Flexor and extensor muscle tone and automatic body movement controlled by CORTICOBULLAR TRACT - Coordination of motor activity while maintaining balance and posture is controlled by the CEREBELLAR TRACTS Motor Neuron Lesions - Upper motor neuron lesions (UMNL) o Interruption of corticospinal tract ABOVE the level of lesion o Results in spastic paralysis, hyperreflexia and (+) Babunski’s sign - Lower motor neuron lesions (LMNL) o Interruption of peripheral motor neurons (corticospinal tract) BELOW level of lesion o Results in flaccid paralysis, decreased or no reflexes, muscle atrophy, (-) Babinski’s sign Congenital and Developmental Disorders of The Nervous System Dysraphic disorders Result from incomplete closure of the fetal neural tube o Anencephaly § No brain, most severe o Spina bifida aperta § Complete exposure of the spinal cord o Spina bifida § (1) Meningocele · Only meninges herniate thru abnormally formed vertebral arches with CSF § (2) Meningomyelocele (a.k.a. Spinal bidida cystica) · Herniation of spinal meninges and spinal cord through posterior vertebral defect to form cystlike outpouching § (3) Myelocele · Protrusion of the spinal cord itself § (4) Spina bifida occulta · Mildest form, defective closure of posterior vertebral arches, intact meninges and spinal cord, site marked by a small skin dimple or tuft of hair Conditions Causing Hydrocephalus - Arnold Chiari Malformation o Obstruction of normal CSF circulation leading to hydrocephalus which causes downward displacement of the cerebellum and extension of medulla oblongata through foramen magnum - Dandy-Walker Malformation o Abdnormal cerebellum development leading to occlusion of the foramina of luschka and magendie causing hydrocephalus Phakomatoses Congenital neurological disorders Tuberous sclerosis o Associated with mental retardation and epileptic seizures o Patient exhibits facial nodules, skin patches, hamartomas and cysts in internal organs - Von HippelLindau disease o Hemangioblastoma of the cerebellum, hemangioma of the retina, tendency to develop renal cell carcinoma and pheochromocytoma - Neurofibromatosis o Type 1multiple cutaneous neurofibromas, pigmented skin lesions (café au lait lesions), pigmented foci in the iris (Lisch nodules) o Type 2- bilateral acoustic schwannomas and less commonly meningiomas Acquired Developmental Disorders - Congenital hydrocephalus o Caused by viruses (rubella, CMV, herpes), causes stenosis or atresia in the fetal aqueduct and leads to obstruction of CSF, leads to dilation of lateral ventricles, cranial sutures are not fused yet and get macrocephaly Cerebral Palsy - Manifestations occur around infancy, get movement abnormalities, spastic paralysis, speech impairments and intellectual deficits Vascular Disorders of The Nervous System - Stoke o Transient Ischemic Attack (TIA) § Can be caused by two different sources: · Carotid TIA o Hemisensory loss, dysphasia, monocular visual loss · Vertebraobasilar TIA o Bilateral sudden visual loss, diplopia, ataxia, vertigo, dysphagia § Focal neurological abnormalities of sudden onset and brief duration. § Rapid or sudden loss of focal CNS including retinal function § Lasts minutes not hours, syncope, confusion, dizziness, migranes with aura, MS like lesions, vestibular systemic disorder and hyperventilation - With stroke two different kinds of swelling can occur: · Cytotoxic edema o Accumulation of water in damaged glial cells and neurons · Vasogenic edema o Extracellular fluid accumulation as a result of breakdown of the blood brain barrier - Hypertension o Hypertensive Encephalopathy § Raised intracranial pressure causes headache, vomiting, drowsiness, papilledema - Venous Infarction o Superior Sagittal Sinus Thrombosis § Occurs after childbirth, get dehydration, starvation, clotting disorders all of which cause headaches and seizures o Cavernous Sinus Thrombosis § Causes raised intracranial pressure, occurs in lateral sinus, causes swollen eyelid, CN 2, 4,5,6, nerve palsies, and seizures - Subarachnoid Hemorrhage o Caused by rupture of an aneurysm, congenital weakening of junctions in circle of willis o Main features are minor headaches, diplopia, facial pain, visual loss Trauma To The Nervous System - Concussion o Temporary loss of consciousness and reflexes, depression of vital functions - Contusion (Bruise) o Almost always occur in two distinct sites, include a coup and countercoup lesion o Anatomic changes in brain o May be permanent neurological impairment - Epidural Hematoma o Skull fracture that lacerates the middle meningeal artery o This condition is lethal unless bleeding is stoped - Subdural Hematoma o Repeated bleedings from ruptured bridging veins o Repeated falls or head injuries usually cause this - Subarachnoid Hemorrhage o Bleeding in the subarachnoid space (b/w the subarachnoid space and pia mater) o Medical emergency - Intracerebral Hematoma o Typically seen after bullet wounds or severe head trauma Spinal Conditions - Cord Syndromes o Upper Motor Neuron Lesion § Results in spastic paralysis (persistent spasm and exaggerated tendon reflexes) o Lower Motor Neuron Lesion § Results in flaccid paralysis (weakness or loss of muscle tone) - Brown-Sequard’s Syndrome o Loss of pain and temperature sensation opposite the side of lesion o Tactile sensation remains intact o Paralysis on side of lesion (ipsilateral) - Central Cord Syndromes o lower motor neuron lesion pattern § Weakness in hands § Normal leg functioning o Radicular disease § Bone spurs § Herniated disc § Damage to segments below lesion o DDX: Nerve root or Peripheral Nerve Disorder § Deficit becomes more profound if the lesion is more distal § Profound sensory and motor deficit in one extremity suggests a peripheral nerve lesion rather than a root lesion Headaches Intracranial Hypertension o Headaches occur daily with nausea and vomiting o Mental status changes and papilledema o Request a CT/MRI scan promptly - Meningeal Irritation o Headaches with fever, (+) Brudzinski’s and/or Kernigs sign o Request lumbar tap for CSF analysis - Subarachnoid Hemorrhage o Worst headaches the patients life o Sudden onset of maximal intensity, hx of trauma o Request CT/MRI scan and lumbar tap - Temporal Arteritis (AKA Giant Cell Arteritis) o Severe temporal headaches, night sweats, shoulder and pelvic pain, anorexia o Palpatory tenderness over temple and scalp o Sudden painless loss of vision, usually in one eye o Associated with polymyalgia rheumatica, leads to blindness o Request ESR, CRP, and temporal artery biopsy - Raised Intracranial Pressure o Mass lesion, pain worse waking, patient wakes at night from pain o Pain worse sneezing, straining, bending, lifting, lying down (valsalva) o Pain associated with nausea and vomiting - Benign Intracranial Hypertension o No mass lesion, morning headache, tinnitus, bilateral pappillodema, vomiting, visual disturbances - Meningeal Irritation o Global/occipital headache, vomiting, exacerbation of sx with bright light o Neck stiffness(nuchal rigidity), (+) Kernig’s sign, acute onset (bacterial meningitis) Mental Status Changes - Dementia o Multiple cognitive function loss in the presence of clear consciousness o 50% caused by Alzheimer’s disease - Cortical Dementia o Amnesia, aphasia (language function lost), apraxia (inability to perform purposeful acts), agnosia (inability to smell), delusions o Normal response to questions, attentive, maintain motor control o Sustained depressive syndrome in 30-60% cases - Subcortical Dementia o Seen in Huntington’s disease and AIDS dementia complex o Slow response to thought and action o Reduced activity and inattention, loose motor control o Sustained depressive syndrome in 10-20% Alzheimer’s Dementia o Is a cortical dementia syndrome o Course of illness § (1) Limbic phase · 2-3 years after onset, anosmia, loss of short term memory, depression § (2) Parietal phase · 3-6 years after onset, loss of comprehension, spoken languor is normal, apraxia, agnosia § (3) Late Fontal phase · 6-8 years after onset, motor disturbances, primitive reflexes and seizures, patient cannot walk or move § Post mortem examination · Small atrophic brain, accumulation of neurofibillary tangles in neurons, beta-amyloid protein § Slow and insidious onset, begins with memory loss, progress to language and motor loss - Delirium o Altered consciousness and cognitive impairment, alternation of consciousness (subtle or severe), alertness can vary (drowsy, hypervigilant), subtle cognitive impairments, obvious behavioral impairments DOWNLOAD