Total Knee Replacement Brochure
advertisement

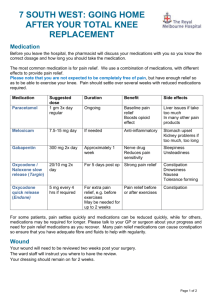
TOTAL KNEE REPLACEMENT Pre Admission Clinic to Hospital Discharge A Total Knee Replacement (TKR) is a procedure which replaces all or part of the knee joint with an artificial device (prosthesis). The goal of the surgery is to relieve your knee pain and allow you to do normal activities like walking more easily. What is a Total Knee Replacement? A total knee replacement replaces the rough joint surfaces. It consists of up to four parts, which are usually fixed with special cement. The end of the thigh bone is made of metal and shaped to provide a groove where the knee cap can sit. The end of the shin bone is usually made up An arthritic knee and a total knee replacement Source: American Academy of Orthopaedic of two parts – a metal tray that is fitted onto Surgeons www.orthoinfo.aaos.org the bone and a plastic spacer in the middle that takes most of the weight. Often the underside of the knee cap is also replaced by a smooth piece of plastic (patellar resurfacing) What sort of anaesthetic will I have? The anaesthetist will discuss with you which type of anaesthetic is best for you (general or spinal anaesthesia) at the Pre-admission Clinic appointment and then again on the day of your surgery. Any questions regarding your anaesthetic can be asked prior to your surgery. Smoking: It is important you stop smoking at least two weeks before surgery. Smoking increases surgical and anaesthetic risk and impairs healing. You are strongly advised to quit. Stopping smoking is not easy but help and support are available which will increase your chances of success. Call Quit line on 137848 for advice and information about these resources. What kind of pain relief will I need? The method of pain relief to be used for you will be decided by your surgeon and anaesthetist as part of the Pre-Admission Clinic assessments, then again on the day of your operation. A combination of tablets (paracetamol, anti-inflammatory, a strong opioid based analgesic and a nerve drug) and injectable medications (local anaesthetic, opioid) will be started just before your operation and continue for up to 10 days after your surgery. You will be reviewed by the pain team on the ward following the operation. During your hospital stay please report to the staff if your pain is not being adequately managed or if you are experiencing side effects of medications including nausea, constipation and dizziness. What will happen when my surgery has been completed? Day of Surgery Following the operation you will be transferred to the Post Anaesthetic Care Unit where you will be monitored You will then be transferred to the Orthopaedic Ward (7SW) when your condition is stable Intra venous fluids and antibiotics will be administered through a Cannula (drip) Antibiotics Oxygen via nasal Cannula Sit on edge of bed or sit out of bed with assistance from the nursing staff as able Day 1 following surgery X-ray of the operated knee to check the position of the implant Blood test The crepe dressing will be removed. Your will have a small dressing over the wound. Wash / shower with assistance from nursing staff Dress in day clothes Sit out of bed for all meals Walk with the physiotherapist using a walking frame or crutches. Nursing staff will assist you to walk to the toilet Commence exercises with the physiotherapist / allied health assistant. Aim to perform exercises 3 times per day. Cold pack may be applied to the knee to reduce swelling and pain Day 2 following surgery Shower (with assistance from nursing staff if required) Dress in day clothes Sit out of bed for all meals Exercises will be reviewed by the physiotherapist. Walk with the physiotherapist and nursing staff Trial steps if you need to use steps at your discharge accommodation Day 3 Dress in day clothes Walk independently with crutches or a frame Walk up and down steps safely (if required to access home) Complete exercise program independently Discharge home or transfer to our Royal Park Campus Rehabilitation Ward Do not place pillows under your knee. This can cause stiffness to your knee. What if I am unwell prior to my surgery? If you are unwell prior to the surgery please contact the Orthopaedic Liaison nurse on 9342 4081. This includes: Chest infection Temperatures higher than 38.5°, fever, sweating, shivering or chills Redness around the knee that is spreading Cuts or grazes near the knee Insect bites Diarrhoea or vomiting the week prior to surgery Contact Pre surgery If you have any queries about your operation prior to your surgery, please contact John Gardiner (Orthopaedic Liaison Nurse): 9342 4081 Post Surgery Orthopaedic ward: contact 9342 7000, asked to be put through to ward 7SW If you have not been provided appointments for follow up in the clinic, please call Bernarda Cavka (Joint Replacement Clinic): 9342 7440 Access Unit| iPolicy Number| Tobi Wilson| February 2016