Concussion Protocol BASELINE TESTING Pre
advertisement
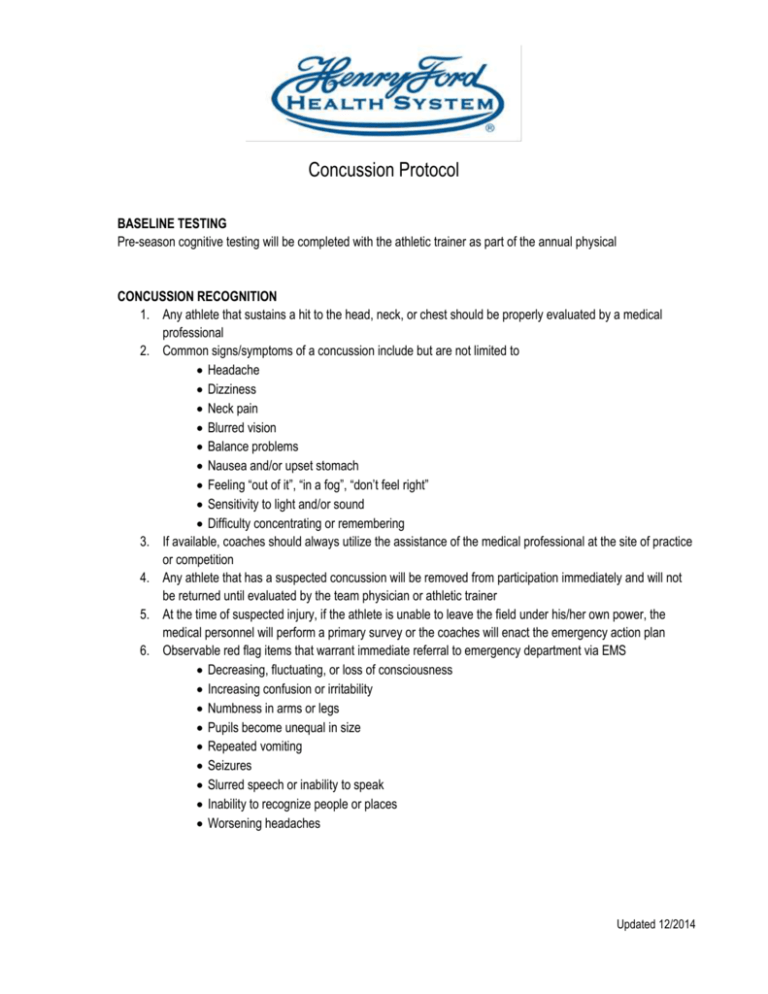
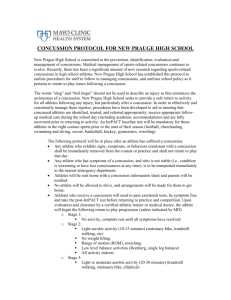
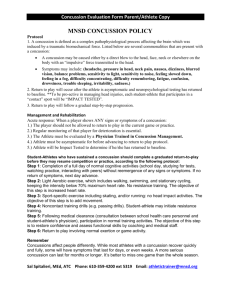
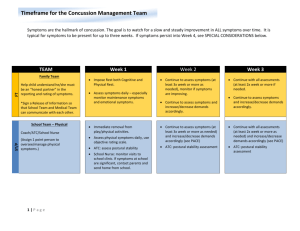
Concussion Protocol BASELINE TESTING Pre-season cognitive testing will be completed with the athletic trainer as part of the annual physical CONCUSSION RECOGNITION 1. Any athlete that sustains a hit to the head, neck, or chest should be properly evaluated by a medical professional 2. Common signs/symptoms of a concussion include but are not limited to Headache Dizziness Neck pain Blurred vision Balance problems Nausea and/or upset stomach Feeling “out of it”, “in a fog”, “don’t feel right” Sensitivity to light and/or sound Difficulty concentrating or remembering 3. If available, coaches should always utilize the assistance of the medical professional at the site of practice or competition 4. Any athlete that has a suspected concussion will be removed from participation immediately and will not be returned until evaluated by the team physician or athletic trainer 5. At the time of suspected injury, if the athlete is unable to leave the field under his/her own power, the medical personnel will perform a primary survey or the coaches will enact the emergency action plan 6. Observable red flag items that warrant immediate referral to emergency department via EMS Decreasing, fluctuating, or loss of consciousness Increasing confusion or irritability Numbness in arms or legs Pupils become unequal in size Repeated vomiting Seizures Slurred speech or inability to speak Inability to recognize people or places Worsening headaches Updated 12/2014 CONCUSSION EVALUATION BY A MEDICAL PROFESSIONAL 1. Athlete self-reported symptoms 2. SCAT 3 (see appendix) and/or ImPACT assessment 3. Balance testing 4. Musculoskeletal examination POST-CONCUSSION MANAGEMENT 1. Once an athlete has been diagnosed with a concussion, he or she will be removed from sport and not allowed to return to activity until cleared by the team physician or athletic trainer, no sooner than the next day 2. Home care - Athletes and their parents/roommates will be provided with a list of signs and symptoms that would indicate a deteriorating condition and warrant immediate referral to the emergency department. The athlete or the designee will be provided with a concussion instruction form (see appendix) 3. Cognitive rest - The goal of cognitive rest is to keep the brain from engaging in mental challenges that will increase symptoms during the post-concussion stage. Cognitive rest if part of a spectrum that ranges from very limited cognitive activity (i.e. absence from school, no use of technology, no social activity, travel) to full cognitive activity (i.e. full school attendance, no technology, social, or travel restrictions). Most concussed patients require some amount of cognitive rest to ensure resolution of symptoms and recovery from concussion The athletic trainer or team physician will work with individual professors and the Counseling and Disability Services department to assist athletes who require major cognitive rest in the classroom Decisions regarding cognitive rest will be based on the severity of each individual case 4. Exertion rest – During the acute recovery period, the athlete will be removed from all physical activity, workouts, conditioning, or from any activity that increases heart rate 5. Medications and diet All concussed athletes should avoid the use of NSAIDs (ibuprofen) or aspirin (Bayer) Acetaminophen (Tylenol) may be used sparingly to ease headaches after a concussion During the sub-acute stage of recovery, the physician may prescribe medications to reduce specific symptoms such as headache, sleep disturbances, or to improve symptom resolution All concussed athletes should avoid alcohol or other recreational substances after a concussion RETURN-TO-PLAY 1. A return to play progression will not start until the athlete no longer reports concussion-related symptoms, has a normal clinical examination, and performs at or above pre-injury level of functioning on all objective concussion assessments 2. The Henry Ford Health System return to play protocol following concussion will be administered and monitored daily by the athletic trainer (see appendix) Updated 12/2014 Concussion Home Instruction Sheet I believe that _________________________________sustained a concussion on _______________________________. To make sure he/she recovers, please follow the important recommendations below: RED FLAG OBSERVATIONS *These signs and symptoms warrant immediate referral to emergency department via EMS Decreasing, fluctuating, or loss of consciousness Increasing confusion or irritability Numbness in arms or legs Pupils become unequal in size Repeated vomiting Seizures Slurred speech or inability to speak Inability to recognize people or places Worsening headaches IT IS OK TO: Go to sleep Use acetaminophen (Tylenol) for headaches Use ice pack on head or neck Eat a light diet Return to school THERE IS NO NEED TO: Check eyes with flashlight Wake up every hour Test reflexes Remain in bed DO NOT: Workout or return to practice Eliminate use of technology (i.e. no computer, texting, video games, and television) Drink alcohol or use recreational substances Eat spicy foods Use NSAIDS (Ibuprofen) or aspirin (Bayer) Recommendations provided by: ________________________________ Date:______________Time:____________ Signature:_____________________________________________________________ Updated 12/2014