Naloxone Fact Sheet
advertisement

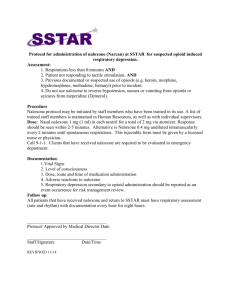
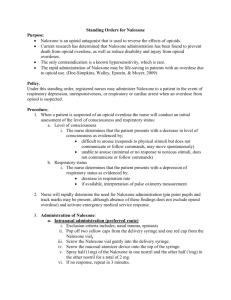
Salvation Army Southern Australia Territory Alcohol and Other Drugs Unit Fact Sheet: Naloxone Naloxone Opioids are a group of drugs that are derived from opium such as heroin or morphine and include synthetic and semisynthetic pharmaceutical drugs such as oxycodone. They depress the central nervous system (CNS), and reduce the rate of respiration. In the case of an overdose, respiration can cease completely which can lead to permanent brain injury, other major organ damage and if untreated, opioid overdose can lead to cardiac arrest and death. Whilst heroin related overdoses have decreased since the late 1990’s the number of fatal overdoses occurring due to pharmaceutical opioids such as oxycodone and slow release morphine products has increased. Deaths from opioid drugs in Australia are rising steadily. Opioid drug overdoses increased 95.8% between 2007 and 2010. The number prescriptions for opioid painkillers have also increased over a 15 year period. The increase has been threefold to 7 million a year. At least three Australians die every day from overdoses. Overdoses outnumbered road fatalities in Australia in 2011. According to the Australian Bureau of Statistics overdose deaths totalled 1,383, while road deaths, which have been steadily declining, ended the year at 1,323. In Victoria prescription drug-related deaths now outnumber those caused on the road. Prescription drugs are present in most overdose deaths. Death and/or disability caused by heroin or pharmaceutical opioids overdose are preventable by administering a dose of Naloxone. Naloxone is a drug known more commonly by the trade name of Narcan® . Naloxone is a full pure opioid antagonist that reverses the effects of natural, synthetic and semi-synthetic opioids including codeine, heroin, methadone, morphine and oxycodone. Naloxone Hydrochloride has no other action than to reduce the effect of heroin and other opioids. It has been used to safely reverse the effects of opioid intoxication in hospital and pre-hospital emergency situations for decades. It has no psychoactive effect thus does not cause intoxication, is not a drug of dependence, and therefore, is not a drug which is likely to be diverted or misused. Naloxone comes in a liquid form for either for injection or for inhalation. It can also be administered via a nasal spray device which converts the naloxone liquid into a fine mist, disabling concerns regarding possible needle-stick injuries. At present, intranasal preparations of naloxone are not licensed in Australia, although application by nasal spray has been trialled in Victoria by paramedics where it was found to be effective and safe. In Australia Naloxone is currently used by medical personnel such as paramedics and emergency room personnel. Although Naloxone is currently only available on prescription in Australia, international evidence shows that non-medical personnel can be trained to safely administer Naloxone, thus preventing death and/or disability. Naloxone has been available from pharmacies as an over-the-counter medication in Italy since 1995 and therefore is available for peer administration. Accruing international evidence since 2000 suggests the distribution of Naloxone to opioid users, their peers and family members can occur with very few, if any, adverse effects and/or negative consequences. In the USA as of December 2008 there were 52 peer-Naloxone distribution programs operating across 17 states and in the UK it is also now available to non-medical people through pilot programs. Legal protection has been extended to nonmedical personnel who administer it in the United Kingdom and parts of the United States. At present in Australia, naloxone can only be provided to members of the general public via medical prescription. These issues have been discussed for more than a decade in Australia. In the longer term, naloxone could be ‘rescheduled’ to make it available as an ‘over-the-counter, pharmacist involved’ purchase in pharmacies; this has been the case in Italy for many years. The sustained mortality among opioid users highlights that current overdose prevention strategies are not sufficient. Treatment programs, such as Opioid Substitution Therapy (Pharmacotherpay), are not primarily aimed at overdose prevention, although they do decrease many of harm associated with drug use. Abstinence-based treatments (eg detox) reduces tolerance to opiods and increases the risk of overdose if use resumes. Distributing naloxone to people who come into contact with opioid users helps preserve life and maintain future treatment options. On 16 December 2011, the Australian Capital Territory (ACT) Government announced that Australia’s first program to provide naloxone to trained potential overdose witnesses would commence in 2012. It will be independently evaluated. Under the ACT program, naloxone is being provided under prescription and 200 people will be trained in overdose related risk factors, recognising opioid overdose and responding to opioid overdose (including resuscitation techniques, calling for an ambulance and the administration of naloxone). At a recent forum held by the Burnet Institute, it was clarified that there are no legal, financial or technical barriers in Victoria to the implementation of peer programs training people in the use of the life-saving opiate overdose reversal drug Naloxone. As a result the City of Yarra which has one of the highest overdoses rates in the state, is calling as a matter of urgency for Naloxone to be distributed to drug users , their peers, families , friends and anyone else who may potentially witness and overdose and who can potentially save the life of another.’ In order to facilitate the introduction of Naloxone the Yarra Drug and Health Forum is set to develop a strategy for the implementation of a Naloxone Distribution Program in the City of Yarra and is calling for others in the AOD sector to advocate and/or support their call for a distribution program. Advocates of this include: Alcohol and Other Drugs Council of Australia Anex – Australian Association Harm Reduction Australian Drug Foundation Australian Medical Association (Vic) Australian Research Centre in Sex, Health and Society Burnett Insitute AVIL – Australian Intravenous Injecting League City of Yarra Family Drug Help and the Family Drug Helpline Victorian Alcohol And Drug Association (VAADA) Law Enforcement Against Prohibition Australia. National Drug Research Institute Public Health Association of Australia UnitingCare ReGen Moreland Hall University of New South Wales Drug Policy - Modelling Program Canberra Alliance for Harm Minimisation and Advocacy (CAHMA) Expanding Naloxone Availability in the ACT (ENAACT) Committee References http://www.overdoseday.com/facts-stats/ http://www.anex.org.au/what-we-do/current-interests/access-to-naloxone/ Anex (2012), Australian Drug Policy: Lifesavers - accessto naloxone to reduce opioid overdose-related deaths and morbidity. Anex, Melbourne, Australia. http://www.atoda.org.au/wp-content/uploads/The_heroin_reversal_drug_naloxone_FIN2.pdf Paul Dietze and Simon Lenton The case for the wider distribution of naloxone in Australia December 2010 http://www.atoda.org.au/policy/naloxone/ Expanding Naloxone Availability in the ACT Stancliff S, Mathews B, Rath C. Building Capacity in Overdose Prevention. Symposium: Increasing community access to naloxone to prevent opioid overdose deaths: lessons for Australia held at the National Conference of the Australasian Professional Society on Alcohol and other Drugs (APSAD) 2010; 2010 1 December 2010; Canberra, 28 November -1 December. Dean R, Negus S, Bilsky E. Opioid Receptors and Antagonists: From Bench to Clinic. New Jersey: Humana Press, 2010. Lenton SR, Dietze PM, Degenhardt L, Darke S, Butler TG. Now is the time to take steps to allow peer access to naloxone for heroin overdose in Australia. Drug Alcohol Rev 2009;28(6):583-5. Darke S, Hall W. The distribution of naloxone to heroin users. Addiction 1997;92(9):1195-9. Fry C, Dietze P, Crofts N. Naloxone distribution: remembering hepatitis C transmission as an issue. Addiction 2000;95(12):1865-6. Lenton SR, Hargreaves KM. Should we conduct a trial of distributing naloxone to heroin users for peer administration to prevent fatal overdose? Med J Aust 2000;173(5):260-3. Lenton SR, Dietze PM, Degenhardt L, Darke S, Butler TG. Naloxone for administration by peers in cases of heroin overdose. Med J Aust 2009;191(8):469. Darke S, Zador D. Fatal heroin "overdose": A review. Addiction 1996;91(12):1765-72. Darke S, Zador D, Sunjic S. Toxicological findings and circumstances of heroin-related deaths in south-western Sydney, 1995, NDARC Technical Report No. 40. Sydney: National Drug nd Alcohol Research Centre, 1997.