Duoloxetine - Wayne Anderson
advertisement

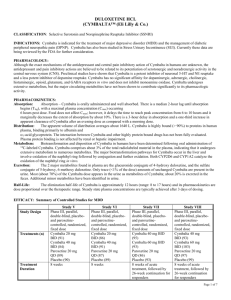
Disclaimer: This is for informational purposes only. This does not replace the instructions you received from Dr. Anderson or any other practitioner, constitute medical treatment, establishment of a patient-physician relationship, constitute any form of recommendation, prescription or medical advice, or imply that the medication is appropriate or FDA approved for any condition. This information may be outdated and is not a complete listing of instructions, doses, uses, or side effects. If this was prescribed to you, you must review this information with your pharmacist and prescriber before starting the medication. Any medication may interfere with the ability to drive, concentrate, or operate machinery; patients must be responsible for their own behavior and should not engage in any dangerous activity if there is any question of impairment. All medications have side effects and drug interactions, some serious, some fatal. Let all of your practitioners and pharmacist know about every substance used. Alcohol, herbals, or illegal drugs are not considered safe with these medications. Assume no medication is safe during pregnancy or while breast feeding. The medication may interfere with birth control. Almost any medication can cause sleepiness, insomnia, dizziness, confusion, hallucinations, anxiety, panic, constipation or diarrhea, headache, chest pain and nausea or vomiting, among others. These could cause physical injury, such as dizziness causing one to fall down stairs. Many reduce blood pressure, which could cause fainting, dizziness, stroke, or other problems. Most medications should NOT be stopped suddenly because of the risk of withdrawal. This is a supplement to the standardized drug information sheets. Drug: DUOLOXETINE Wayne E. Anderson, D.O. A Medical Corporation Chronic Intractable Pain Disorders Headache & Facial Pain Disorders Neurotoxin Therapy FDA-approved uses: The pain of diabetic neuropathy, fibromyalgia, chronic musculoskeletal pain due to chronic osteoarthritis and chronic low back pain. Also, generalized anxiety disorder and major depressive disorder. Common off-label uses: Neuropathic pain and musculoskeletal pain of causes other than the low back or arthritis. Neuropathy and neuropathic pain from causes other than diabetes. Alternatives: Non-medication modalities, pain interventions and other medications that may work in a similar manner. Board Certified Neurology American Board of Psychiatry & Neurology Board Certified Pain Medicine American Board of Psychiatry & Neurology in association with the American Board of Anesthesiology Subspecialty Certified Headache Medicine United Council for Neurological Subspecialties Qualified Medical Evaluator Member of the California Pacific Neuroscience Institute 45 Castro Street Suite 225 San Francisco CA 94114 415.558.8584 tel 415.513.4521 fax www.wayneanderson.net How it works: This medication works by helping to prevent the destruction of two of the nervous system’s important natural chemicals: serotonin and norepinephrine. These neurotransmitters are involved in reducing the perception of pain. Side effects: Please see the standardized drug information sheet for detailed information about risks, side effects, interactions, and other important information. Common side effects include sleepiness, dizziness, nausea and dry mouth are common side effects. Like most medications, the liver helps remove the medication from the body. Therefore, Cymbalta must be used carefully if there is any liver disease. Like most pain medications, Cymbalta should not be used with alcohol. There have been cases of liver problems with the medication and it seems that the liver problems occur more frequently in alcohol users. Cymbalta should not be used with uncontrolled narrow-angle glaucoma. It should not be used with MAO inhibitors. As with all antidepressants and other neuropathic pain medications, there is a potential worsening of depression when the medication is first started. All medications in this class may worsen depression when first started, possibly resulting in suicide. This is rare, but all patients should be aware of the risk and should let the prescribing provider know immediately of any worsening of depression. Common doses: The FDA-approved doses begin at 20-30mg per day and increase to 60mg per day. Many pain patients use 90mg to 120mg per day. Those doses, although helpful, were not evaluated by the FDA. Most patients start with 30mg per day. Some patients start with 20mg per day. Time to effect: The time to effect depends on the use or uses for the medication. Neuropathic pain may improve in a few weeks, but depression may improve in a few months. Financial: Dr. Anderson has never received payment in exchange for prescribing a medication. Dr. Anderson has no financial relationship with the company that manufactures duloxetine. Insurance coverage: Many medications, especially in painful conditions, are off-label as discussed above. Insurance companies do not need to cover medications used off label but typically do provide coverage for most medications that have good scientific evidence. There is no guarantee that any medication will be covered. However, this medication has quite a bit of scientific evidence and most insurance companies do provide coverage. Clinical and Scientific evidence: Some scientific evidence supportive of the use of the medication is listed in this section. Of course, scientific information changes rapidly and the information listed may become outdated or incorrect overnight. Duloxetine is a serotonin and norepinephrine reuptake inhibitor that reduces the body’s destruction of these two natural neurotransmitters. These two neurotransmitters are involved with pain perception. It is FDA approved for fibromyalgia, diabetic neuropathy, a certain type of back pain, and depression. SSNRI medications are considered first-line treatments for fibromyalgia-like neuropathic pain syndromes. The literature suggests that duloxetine may have benefit in other types of chronic pain as well, especially if depression is present along with the pain. References: 1. 2. 3. 4. 5. Buckhardt CS, Goldenberg D, Crofford L, Gerwin R, Gowens S, Jackson K, Kugel P, McCarberg W, Rudin N, Schanberg L, Taylor AG, Taylor J, Turk D. Guideline for the management of fibromyalgia syndrome pain in adults and children. Glenview (IL): American Pain Society (APS); 2005. Also at National Guideline Clearinghouse as Guideline for the management of fibromyalgia syndrome pain in adults and children. Management of fibromyalgia syndrome in adults. National Guideline Clearinghouse, Dept of Health and Human Services. Häuser W, Petzke F, Uçeyler N, Sommer C. Comparative efficacy and acceptability of amitriptyline, duloxetine and milnacipran in fibromyalgia syndrome: a systematic review with meta-analysis. Rheumatology (Oxford). 2010 Nov 14. Lee YC, Chen PP. A review of SSRIs and SNRIs in neuropathic pain. Expert Opin Pharmacother. 2010 Dec;11(17):2813-25. Epub 2010 Jul 19. Kroenke K, Krebs EE, Bair MJ. Pharmacotherapy of chronic pain: a synthesis of recommendations from systematic reviews. Gen Hosp Psychiatry. 2009 May-Jun;31(3):206-19. Epub 2009 Mar 4.