ONLINE APPENDIX Aortic Valve Area Calculation in Aortic Stenosis
advertisement
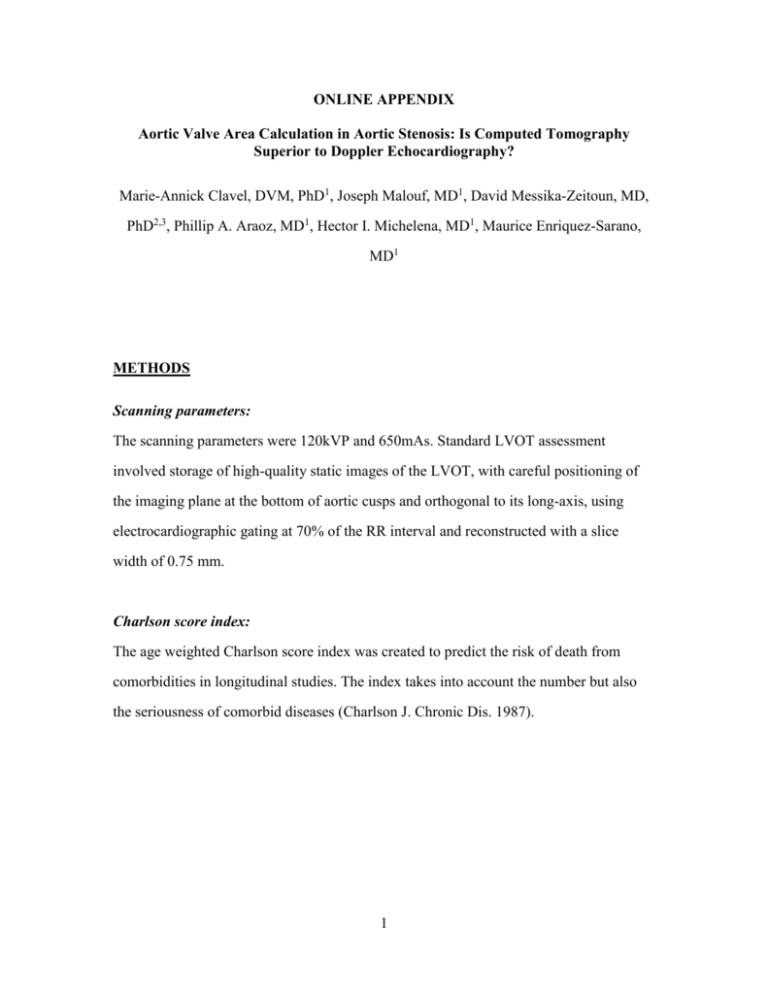
ONLINE APPENDIX Aortic Valve Area Calculation in Aortic Stenosis: Is Computed Tomography Superior to Doppler Echocardiography? Marie-Annick Clavel, DVM, PhD1, Joseph Malouf, MD1, David Messika-Zeitoun, MD, PhD2,3, Phillip A. Araoz, MD1, Hector I. Michelena, MD1, Maurice Enriquez-Sarano, MD1 METHODS Scanning parameters: The scanning parameters were 120kVP and 650mAs. Standard LVOT assessment involved storage of high-quality static images of the LVOT, with careful positioning of the imaging plane at the bottom of aortic cusps and orthogonal to its long-axis, using electrocardiographic gating at 70% of the RR interval and reconstructed with a slice width of 0.75 mm. Charlson score index: The age weighted Charlson score index was created to predict the risk of death from comorbidities in longitudinal studies. The index takes into account the number but also the seriousness of comorbid diseases (Charlson J. Chronic Dis. 1987). 1 End-point: Online Table 1: Summary of end-points, follow-up measurements and events. Time Endpoint start End (whichever comes first) AVR Death End FU Event noted Event Excluded event Death only Death after AVR AVR 378 Pt-yr 55 Not counted as event Measured Time Events Survival under medical management Diagnosis Total Mortality Diagnosis Death End FU Death only No death excluded AVR 826 Pt-yr 90 Death or AVR Diagnosis AVR Death End-FU Death AVR Death after AVR (AVR counted as the earlier event) -- 378 Pt-yr 201 2 RESULTS Echocardiographic and Dynamic MDCT measurements of LVOT/Annulus and AVA In patients in whom dynamic MDCT measurements were available (n=135), the correlation between phasic measurements of LVOTArea by MDCT was excellent (r=0.90; p<0.0001). These LVOTArea measures by MDCT showed reasonable correlations with the area calculated by echocardiography (both r≥0.71; all p<0.0001). However, LVOTArea by echo (3.86±0.71 cm2) was smaller (all p<0.001) than LVOTArea by CT. Dynamic 4D-MDCT showed slight variations in phasic measurement of LVOT eccentricity with less eccentricity in systole (eccentricity index: 0.83±0.07 vs. 0.77±0.09; p<0.001). The phasic differences reached significance (p<0.001) but the higher measurement in systole was minimal in magnitude (4.74±0.98 vs. 4.46±0.95 cm2). Fig.SM1 shows correlation and agreement between the different technics used to calculate AVA. Fig.SM2 shows correlation and agreement between AVAEcho and AVACT in the whole cohort. Relationship between Mean Gradient and Indexed AVACT or Indexed AVAEcho The correlation between mean gradient and Indexed AVA was better (Wolfe-p=0.001) for Indexed AVAEcho (r=-0.65; p<0.0001) than Indexed AVACT (r=-0.60; p<0.0001). Spline curve analysis and threshold definition: The definition of threshold for excess mortality was done with the use of spline curve of mortality (y-axis: relative risk of mortality within the series; y-axis: AVA Echo or CT – Fig. 6). The interception between the spline curve itself and the relative risk of 1 (mean risk for the series) was the best cut-off value to define excess mortality. Interestingly, this intercept was for AVAEcho of 1cm2, which also is the cut point used in the guidelines and was for AVACT of 1.2 cm2. A second threshold of 0.8 cm2 for AVAEcho and 1cm2 for AVACT represent the intersection between the lowest 95% confidence interval of the spline curves and the relative risk of 1. This 3 second threshold was also analyzed due to the intense controversy on appropriate AVA thresholds to define excess mortality in aortic stenosis. Discordance in AS severity grading by AVACT or AVAEcho Our series comprised 205 patients with preserved LV ejection fraction (≥50%). Among those, 27 (13%) had a low ΔP despite tight AVA by echocardiography (AVAEcho≤1cm2). For AVACT, using the threshold for tight AVA of AVACT≤1.2 cm2 defined in the survival analysis (see below), low ΔP affected 25 (12%) patients, a proportion identical (p=0.75) to that defined by AVAEcho≤1cm2. The eccentricity index by MDCT did not affect the concordance Mean GradientAVAEcho and was equivalent (p=0.50) between patients with discordant AS severity echocardiographic grading (0.80±0.07) vs. those with concordant moderate (0.80±0.07) or severe (0.80±0.08) AS. Thus, in all subsets and with any threshold, AVACT did not improve the concordance of AS severity grading. 4 Impact of AVAEcho and AVACT on survival in AS: Net reclassification index In order to assess the potential superiority of AVACT we calculated the net reclassification index (NRI) at 1 year using AVACT instead of AVAEcho. Among our patients, 13 (5%) were classified as non-severe AS with AVAEcho and were reclassified as severe AS with the use of AVACT, while 21 (8%) were classified as severe AS with AVAEcho and were reclassified as non-severe AS with the use of AVA-CT. Online Table 2: Classification of AS severity according to AVAEcho and AVACT in deceased and alive patients at 1 year: 62 Deceased patients at 1 year: AVAEcho>1.0cm2 AVAEcho≤1.0cm2 AVACT>1.2cm2 4 8 AVACT≤1.2cm2 1 49 AVAEcho>1.0cm2 AVAEcho≤1.0cm2 AVACT>1.2cm2 54 8 AVACT≤1.2cm2 6 37 105 Alive patients at 1 year: Thus the NRI at 1 year was -9%, that representing a “worsening” of classification, while didn’t reach statistical significance (p=0.81) with regards to survival prediction. Online Figure 1: Correlations (Panels A, C, E and G) and agreements (Bland-Altman plot; Panels B, D, F and H) between the Echocardiography and Multi-detector Computed 5 Tomography for estimation of aortic valve area in the subset of 135 patients with all measurements. Online Figure 2: Correlation (Panel A) and agreement (Bland-Altman plot; Panel B) between the Echocardiography and Multi-detector Computed Tomography for estimation of aortic valve area in the whole cohort (n=269) Online Figure 3: Correlations between mean gradient and indexed aortic valve area in the whole cohort. Indexed AVA was calculated by Doppler-echocardiography (Indexed AVAEcho: Panel A), MDCT with LVOT measurement (Indexed AVACT: Panel B). 6 Online Figure 1 7 8 9 Online Figure 2 10 Online Figure 3 11