OCULAR ALLERGIC DISEASE
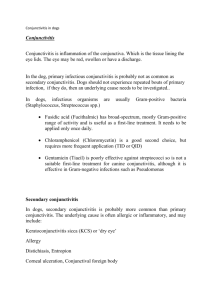
advertisement

INDEPENDENT WORK DEPARTMENT : OPHTALMOLOGY DEPARTMENT CHIEF : BILOLOV E. 2013 OCULAR ALLERGIC DISEASE GROUP : 515 PERFORM BY: AKHMEDOV SHOXRUKH CHECKED BY: SAIDA MAMAJONOVA TASHKENT 2013 OCULAR ALLERGIC DISEASE PURPOSE OF REVIEW: This review will focus on recent advances in our understanding of the pathogenesis of allergic eye diseases. Common findings in acute allergic conjunctivitis (seasonal and perennial) and chronic allergic conjunctivitis vernal keratoconjunctivitis atopic keratoconjunctivitis giant papillary conjunctivitis include evidence of mast cell activation and eosinophil attraction and activation. Cytokine levels found in tears, conjunctival impression cytology and biopsy specimens, and serum have been evaluated as markers of disease, and as targets of therapeutic intervention. RECENT FINDINGS: Human conjunctival epithelial cells respond to tumor necrosis factor alpha, interleukin-1 beta, and interferon-gamma individually and in combination. Intracellular adhesion molecule-1 expression is upregulated by interleukin-1 beta and tumor necrosis factor alpha. Conjunctival epithelial cells release interleukin-8 in response to interleukin-1 beta and tumor necrosis factor alpha but not interferon-gamma. Supernatants from activated mast cells cause increased adhesion of eosinophils to conjunctival epithelium. Tear levels of tumor necrosis factor alpha were elevated in vernal keratoconjunctivitis patients compared with normal controls. T cell lines from chronic allergic eye disease patients showed inconsistent production of cytokines in atopic and vernal keratoconjunctivitis and low levels in giant papillary conjunctivitis. Vernal keratoconjunctivitis patients have differing levels of eosinophil cationic protein in their serum if they were serum specific immunoglobulin E positive compared to serum specific immunoglobulin E negative patients. Definition Allergic conjunctivitis Allergic conjunctivitis, also called "allergic rhinoconjunctivitis," is the most common allergic eye disorder. The condition is usually seasonal and is associated with hay fever. The main cause is pollens, although indoor allergens such as dust mites, molds, and dander from household pets such as cats and dogs may affect the eyes year-round. Typical complaints include itching, redness, tearing, burning, watery discharge, and eyelid swelling. To a large degree, the acute (initial) symptoms appear related to histamine release. The treatments of choice are topical antihistamine drops such as olopatadine (Patanol), decongestants, and the newer mast-cell stabilizer medications. Topical steroids should be used only if prescribed by a doctor for severe reactions and on a short-term basis because of the potential for side effects. In general, oral antihistamines like loratadine (Claritin) or cetirizine (Zyrtec) are the least effective option, but they are often used for treating allergic rhinitis together with allergic conjunctivitis. Rubbing itchy eyes is a natural response. However, rubbing usually worsens the allergic reaction due to the physical impact on the mast cells, which causes them to release more mediators of the immune response. Translation: Do not rub your eyes! Conjunctivitis with atopic dermatitis Commonly called "atopic keratoconjunctivitis," this condition is a notorious cause of severe eye changes, particularly in young adults. Atopic keratoconjunctivitis implies inflammation of both the conjunctiva and cornea. "Kerato" means pertaining to the cornea. This form of conjunctivitis usually affects adolescent boys (three times more frequently than girls) and is more common in those who had atopic dermatitis in early childhood. The condition is characterized by intensely itchy, red areas that appear on the eyelids. A heavy discharge from the eyes can occur, and the skin of the eyelid may show scales and crusts. In severe cases, the eyes become sensitive to light, and the eyelids noticeably thicken. If managed poorly, there can be permanent scarring of the cornea due to chronic rubbing and scratching of the eyes. This scarring can cause visual changes. The triggers for atopic keratoconjunctivitis appear to be similar to those of atopic dermatitis. A search for common food allergies, such as eggs, peanuts, milk, soy, wheat, or fish is important. Airborne allergens, particularly dust mites and pet dander, have been overlooked as a significant contributing factor and should be evaluated and controlled. The hallmark of treatment for allergic conjunctivitis is the use of potent antihistamines (similar to those used in atopic dermatitis) to subdue the itching. Topical antihistamines, mast-cell stabilizers, and the short-term use of oral steroids are all beneficial for relief of the itching. Occasionally, an infection of the area (usually with staphylococcus, commonly referred to as "staph") worsens the symptoms, and antibiotic treatment may help control the itching. Allergy shots are useful in selected cases. Allergy alert Atopic keratoconjunctivitis can lead to cataract formation in up to 10% of cases. In rare cases, blindness can occur. Vernal keratoconjunctivitis Vernal keratoconjunctivitis is an uncommon condition that tends to occur in preadolescent boys (3:1 male to female ratio) and is usually outgrown during the late teens or early adulthood. (Vernal is another term for "spring.") Vernal keratoconjunctivitis usually appears in the late spring and particularly occurs in rural areas where dry, dusty, windy, and warm conditions prevail. The eyes become intensely itchy, sensitive to light, and the lids feel uncomfortable and droopy. The eyes produce a "stringy" discharge and, when examined, the surface under the upper eyelids appears "cobblestoned." A closer examination of the eye reveals severe inflammation due to the vast number of mast cells and accumulated eosinophils (a type of white blood cell involved in the allergic response), producing so-called called "Trantas dots." Improper treatment of vernal keratoconjunctivitis can lead to permanent visual impairment. The most effective treatment appears to be a short-term course of low-dose topical steroids. Topical mast-cell stabilizers and topical antihistamines can also be beneficial. Wraparound sunglasses are helpful to protect the eyes against wind and dust. Allergic conjunctivitis is a broad group of allergic conditions involving inflammation of the conjunctiva. The commoner conditions are mild and do not affect the cornea. The rarer diseases involve the cornea and can be sight-threatening. Classification 1. Seasonal, intermittent, IgE-mediated allergic conjunctivitis (SAC) 2. Perennial, persistent, IgE-mediated allergic conjunctivitis (PAC) These common IgE mediated diseases are related to seasonal or perennial allergens. They are characterized by symptoms of ocular itching, watering and redness, and signs of hyperaemia and oedema of the tarsal conjunctival surfaces. There is frequently an association with allergic rhinitis. SAC is intermittent in nature, and, in temperate regions, follows exposure to pollen allergens in sensitized individuals. PAC is a mild, persistent form of allergic conjunctivitis resulting from continuing exposure to persistent allergens such as house dust mites. Vernal keratoconjunctivitis (VKC) This is a severe inflammatory disease which may be intermittent or, less frequently, persistent. VKC is, in about 60% of cases, associated with IgE-dependent hypersensitivity. The symptoms are ocular watering, stickiness, itching, and difficulty with opening the eyes on awaking. If the cornea is involved, pain, blurred vision and photophobia are experienced. The signs are giant papillary hyperplasia of the upper tarsal conjunctival surfaces, erosion of the corneal epithelium and inflammation at the limbus (click for photograph). Atopic keratoconjunctivitis (AKC) This is a severe disease which is associated with atopic eczema. The condition is lifelong, starting in the third of fourth decade. IgE-mediated mechanisms may be implicated. The symptoms are perpetual ocular itching, soreness, impaired vision and a sensation of dryness (click for photograph). Signs include chronic lid margin infection, chronic cicatrising conjunctivitis, eczema of the eyelids, tear abnormality, and progressive scarring and vascularization of the cornea. Giant papillary conjunctivitis (GPC) This disease, also known as foreign body associated papillary conjunctivitis, results from trauma caused by contact lens edges, ocular protheses or post-operative sutures. It may also evolve from spontaneous lid eversion resulting in conjunctival rubbing against the pillow, the so-called floppy eyelid syndrome. Upper subtarsal papillae, not always giant in size (> 1mm), is the hallmark sign of the disease. There is no evidence that generally IgE-sensitized individuals are at greater risk of developing the disease. The cornea is rarely involved. Causes Seasonal, intermittent, IgE-mediated allergic conjunctivitis Seasonal, intermittent, allergic conjunctivitis is triggered by the same allergens responsible for intermittent allergic rhinitis. In the Northern Hemisphere these are tree pollens in April/May, grass pollens in June/July, and mold spores and weed pollens in July/August. Perennial, persistent, IgE-mediated allergic conjunctivitis Perennial, persistent, allergic conjunctivitis is triggered by house dust mites, molds and animal allergens, which may be present year round, although the symptoms do show some seasonal variation. In the Southern Hemisphere the pollen season can be all year round, depending on the region. Vernal keratoconjunctivitis The majority of cases of VKC are intermittent and can occur during the high pollen season, although persistent cases do occur in warm subtropical or desert climates. Published reports of the association with IgE-mediated atopic disease vary between 15% to 60%. While there is a relationship between the condition and positive skin tests, the relationship is not necessarily causal. Atopic keratoconjunctivitis AKC is a perennial disease which, when associated with the IgE-mediated subgroup of atopic eczema, may be exacerbated by contact with specific allergens such as house dust mites, mold spores, animal danders and rarely foods. Giant papillary conjunctivitis Giant Papillary Conjunctivitis occurs in the presence of foreign bodies in the eye, such as contact lenses or ocular prostheses. Papillae develop on the upper tarsal conjunctiva along the line of contact with the source of mechanical trauma, e.g., the lens edge. The upper eyelid may be traumatized with each blink of the eye, which occurs between 10,000 and 12,000 times daily, and the area of trauma may serve as an entrance for antigen possibly derived from altered proteins or chemicals in contact lens solutions, although no single causative allergen has been identified in this condition to date. Diagnosis of Allergic Conjunctivitis Clinical examination and investigations Appearance of the everted eyelid. This may be performed by using a long thin object, such as a cotton bud, as a fulcrum at the top of the tarsal plate, while the eyelashes are pulled forward and up. Conjunctival scrapings for eosinophils may be helpful Skin prick/puncture tests or specific IgE tests to identify causative allergens Clinical history Typical symptoms 80% of patients are under 30 years of age Strong personal or family history of IgE-mediated diseases Recurrent intermittent or persistent symptoms Mediators of IgE-related reactions in allergic conjunctivitis Histamine: Itching, redness, oedema Prostaglandins: Sensitized nerves, enhanced pain, oedema and redness Leukotrienes: Chemotaxis, oedema and vascular permeability Chemotactic factors: Recruitment of eosinophils and neutrophils leading to tissue destruction Differential diagnoses of allergic conjunctivitis include Atopic blepharitis Bacterial conjunctivitis Chlamydial conjunctivitis Corneal abrasion or ulceration Dry eye Episcleritis Epithelial microcysts and vacuoles Staphylococcal marginal keratitis Superficial punctate keratitis Tight lens syndrome Viral conjunctivitis or keratitis Ocular itching is a cardinal symptom of allergic eye disease and in the absence of itching an alternative diagnosis should be suspected. Epidemiology SAC SAC may occur alone or as a component of seasonal/intermittent allergic rhinitis (hay fever). Both SAC and PAC are primarily diseases of young adults, and there is a slightly higher prevalence in males. VKC VKC is a disease of childhood and early adolescence. Genetic factors and atopic status may be involved in the development of the disease, although many patients have no familial or personal history of atopy, and may have negative allergy diagnostic tests. Thus, like atopic eczema it might represent a syndrome with allergic and non-allergic subgroups. Males are more frequently affected than females, with a ratio of 3:1. The disease usually begins before the age of 10 years and remits at the time of puberty, although the age of affected individuals ranges from 3 to 25 years of age. VKC may progress to atopic keratoconjunctivitis. VKC occurs more frequently in warm climates and subtropical areas, in particular the Mediterranean area, central Africa, India and South America. It is also reported in Australia, China, Japan and North America. The incidence of the disease in cooler climates in Northern Europe is thought to reflect migration of susceptible individuals, and it is thought that both genetic and environmental factors contribute to the development of the disease. AKC AKC first occurs in the late teens or early twenties with a peak incidence between the ages of 30 – 50 years. It is more frequent in men and occurs in up to 25% of patients with atopic eczema. There is usually a personal or family history of atopic disease. GPC GPC associated with contact lens use reflects the age of contact lens wearers and thus rarely occurs in children or the elderly. However when associated with post-surgical mechanical trauma, such as exposed sutures, it is more prevalent in older age groups. There is no gender predominance. Prevention Allergen avoidance can lead to significant improvement in symptoms of SAC and PAC. In GPC, the use of disposable contact lenses may be helpful if lens deposits are causing symptoms, and changing to daily use of disposable lenses can eliminate the condition entirely. Treatment Recommendations for the treatment of seasonal, intermittent, and perennial, persistent allergic conjunctivitis are available on the GLORIA area of this website. Treatment of the rarer, more severe forms of allergic conjunctivitis requires the use of topical corticosteroids and should be managed by an ophthalmologist. Prolonged use of topical steroids in the eye can lead to secondary bacterial infection, intra-ocular hypertension, glaucoma and cataract, and thus regular monitoring is essential. To print out WAO's pocket chart on treatment of allergic rhinitis and allergic conjunctivitis, click here. VKC Cromones and other mast cell stabilisers may be prescribed alone, or in addition to topical steroid therapy. Mucolytic drops (acetylcisteine 5% or 10%) may be used to control the symptoms caused by abnormal mucus. AKC In addition to topical corticosteroid therapy, treatment of the infected lid margins with topical or systemic antibiotic may help to reduce symptoms. Cromones and other mast cell stabilizers may be of value. Treatment of eye lid eczema with steroid ointments may be of value. GPC The condition, fit and cleaning schedule of contact lenses or prosthesis should be reviewed. Opticrom or similar drugs may be used if required. Topical steroids should not be used for contact lens wearers, but may be given for prosthesis wearers, where no risk to damage of the eye can occur. SUMMARY: Recent findings continue to expand our basic knowledge of mechanisms and differences between seasonal and perennial allergic conjunctivitis and atopic and vernal keratoconjunctivitis. Understanding the complex interactions and cross talk between cells, cytokines and other mediators is relevant for new therapeutic approaches directed at specific disease entities.