View/Open - Sacramento
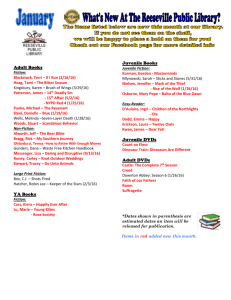
advertisement

CHILDHOOD HEAD INJURY AS IT RELATES TO VIOLENT CRIMINAL BEHAVIOR: KNOWLEDGE AND TREATMENT A Project Presented to the faculty of the Department of Criminal Justice California State University, Sacramento Submitted in partial satisfaction of the requirements for the degree of MASTER OF SCIENCE in Criminal Justice by Veronica Lynn Piazza SUMMER 2013 CHILDHOOD HEAD INJURY AS IT RELATES TO VIOLENT CRIMINAL BEHAVIOR: KNOWLEDGE AND TREATMENT A Project by Veronica Lynn Piazza Approved by: __________________________________, Committee Chair David H. Swim, D.P.A. ____________________________ Date ii Student: Veronica Lynn Piazza I certify that this student has met the requirements for format contained in the University format manual, and that this project is suitable for shelving in the Library and credit is to be awarded for the project. __________________________, Graduate Coordinator Yvette Farmer, Ph.D. Division of Criminal Justice iii ___________________ Date Abstract of CHILDHOOD HEAD INJURY AS IT RELATES TO VIOLENT CRIMINAL BEHAVIOR: KNOWLEDGE AND TREATMENT by Veronica Lynn Piazza Statement of Problem Children suffer from head injury and traumatic brain injury due to the many sports and activities in which they participate, which in many cases causes severe impairment or death. The problem is that when juveniles are arrested, the criminal justice system is unaware of whether the juveniles have suffered such injury or the significance of the inquiry. Juveniles are being adjudicated for offenses they may not be able to prevent due to changes in impulse control, such as vehicle theft or robbery, and they are being referred to treatment programs that may not be able to address the juveniles’ actual problems. These juveniles subsequently do not successfully complete said treatment and are passed through the criminal justice system as persistent offenders. The purpose of this project is to provide information about the symptoms and consequences of head and brain injury, to review and examine current assessment tools for questions about head injury, and to provide an assessment tool and protocol that can be used by probation departments to gather the appropriate information regarding the iv juvenile, the alleged offense, and the possible dispositional alternatives. This information will aid probation officers in developing the most accurate case plan for injured juveniles and referring them to the appropriate evidenced-based treatment program. Sources of Data This project reviewed literature in the medical, psychological, and criminal justice fields that analyzed and discussed head injury. This project also encompasses information based on this researcher’s experience, expertise, and training as a Deputy Probation Officer to further the understanding of the need to provide accurate and thorough information in the criminal justice field. Information was also reviewed regarding adult patients suffering from TBI, as research on TBI amongst youth is quite limited. However, the information serves to show the detrimental effects of head and brain injury on an individual, which would be worse for a juvenile, as their brains are still growing and developing. This project provided information on three different assessment tools, and examined them for any assessment of head injury. The assessment tool and protocol developed in this project were based on the information reviewed in the literature. Conclusions Reached Three of the current assessment tools used by probation departments around the United States do not assess for head injury or traumatic brain injury. Therefore, a great many juveniles are being adjudicated and held liable for actions they may not be able to control, are being exposed to potential harm in general population housing units, are v being perceived as persistent, and are not receiving the proper rehabilitative services. If probation departments were aware of the seriousness and impact of head or brain injury, they might be able to make the proper dispositional recommendations in the juveniles’ cases, refer the juveniles and their families to the proper rehabilitative and treatment agencies, and better serve the clientele they supervise. These tasks will be that much easier with the implementation of the Assessment of Head Injury Tool (AHIT) and protocol. This instrument will aid probation officers in more thoroughly assessing the juveniles that enter their detention facilities, and help them determine who may be suffering from a TBI, how to refer them for treatment, and how to report the information. _______________________, Committee Chair David H. Swim, D.P.A. _______________________ Date vi DEDICATION Dear sweet mother, Jac’lene Yvonne Rowe, you have always been my heart, my soul, my teacher, my mentor, my inspiration, and my best friend! Without you, there would be no me! When I placed my first college graduation cap on your head, it was to symbolize your accomplishment in raising your daughter. As you sit in heaven looking down on me wearing my second, please know that it symbolizes your success in passing the torch that lights the womanhood and motherhood inside me aflame! You continuously encouraged me to get my Masters, and now I have. I dedicate this project to you, Momma! I never gave up because of you, and I never will. I thank God for you and will miss you all the days of this life! By the Grace of God, you will live in my heart and mind forever! Rest in Perfect Peace! Bunches Mom! I would also like to dedicate this project to my two wonderful babies, Leilani Jac’lene Piazza and Brian Piazza Jr., who spent many days in class with Mommy. You two are the love of my life! You are the air that I breathe and the reason I live! This achievement will symbolize the strength and dedication that lies deep inside you both. Always know that Mommy did it, and you will too! Never give up on yourselves or your dreams, and know that Mommy will always be here to support you both, as Grammy was for me! Mommy loves you both! Yours Always, Veronica Lynn Piazza vii ACKNOWLEDGEMENTS Education has always been a priority in my life, and as such, accomplishing my educational goals was never a real struggle. However, during the course of the Graduate Program, I lost my mother and maternal grandmother in one week. This was devastating, and the loss of concentration was uncontrollable. I realized my mother’s spirit was still encouraging me to continue my education through the encouragement and support of two great women, Donna Vasiliou, the Administrative Support Coordinator II in the Division of Criminal Justice, and Dr. Yvette Farmer, Associate Professor and Graduate Program Coordinator in the Division of Criminal Justice. I could not have made it through this program and the losses in my life without the Grace of God working through these two wonderful women. From the bottom of my heart, I want to thank God and the both of them for their continued support and guidance. I will always have a special place in my heart for you both. Also, I want to thank all of my family, especially my sister, Stephanie DennieSmith, and friends for their continued support, encouragement, and willingness to babysit whenever I needed them. Pursuing higher education as a full-time working mother of two is definitely not easy, so I greatly appreciate my family and friends stepping in to help! Thank you so very much! Love, Veronica Lynn Piazza viii TABLE OF CONTENTS Page Dedication…………………………………………………………………………..vii Acknowledgements……………………………………………………………….. viii Chapter 1. INTRODUCTION……………………………………………………………......1 Statement of the Problem………….………………………………………….1 Purpose of the Project ………………………………………………………..5 Summary…………………..………………………………………………….6 2. REVIEW OF LITERATURE…………………………………………………... .7 Introduction………………………………………………………… …….....7 Neurological Consequences………………………………………………….7 Current Causes of Traumatic Brain Injury…………………….……………15 Treatment of Brain Injury ………………………………………………......22 Behavioral Changes……..……………………………………………….… 34 Conclusion: Knowledge, Assessment, and Treatment….…………………...38 Summary………………………………………….………………………....40 3. PROJECT OVERVIEW………………………………………………………...41 Introduction…………………………………………………………….…....41 Purpose and Intent………………………………………………………......42 ix Risk Assessments……………………….....………………………………..43 Detention Risk Assessment Instrument….………………...……………….44 Analysis of DRAI…………………………………………………………...52 Youth Assessment and Screening Instrument……………………………....54 Analysis of YASI…………………………………………………………...58 Positive Achievement Change Tool………………………………………...59 Analysis of PACT…………………………………………………………...62 Summary…………………………………………………………………….64 4. ASSESSMENT TOOL AND PROTOCOL………………………………….....67 Researcher’s Proposal……………………………………………………….67 Assessment of Head Injury Tool…………………………………….……...69 Protocol…………………………………………………………….……......71 Implementation Concerns and Summary……………….……………..........74 5. CONCLUSION…………………………………………………………...…......77 Appendix A. Codification Key…………………...………………..…..........81 Appendix B. Assessment Analysis……………...…………………………..82 References…………………………………………………………………..83 x 1 Chapter 1 Introduction Statement of the Problem Injury to the head may damage the scalp, skull or brain, and the most important consequence of head trauma is traumatic brain injury (TBI) (Miura, Fujiki, Shibata, & Ishikawa, 2005, p. 662). Head injury may occur either as a closed head injury or as a penetrating head injury, and both may cause damage that ranges from mild to profound (Miller, 1999, p.158; Miura et al., 2005, p. 662). Closed head injuries are nonpenetrating injuries that usually result from incidents such as road traffic accidents, assault, work, and sporting injuries and are a common form of brain damage in young adults (Miller, 1999, p.158; Miura et al., 2005, p. 662). A penetrating head injury is a brain injury that occurs when an object penetrates the skull or the skull is fractured, and bone fragments, foreign material, or dirt can get into the brain, damage the brain tissue, and cause infection (Miller, 1999, p.158; Miura et al., 2005, p. 662). Head injuries where there is a loss of consciousness for a long period of time, minutes or hours, can have great psychological consequences (Miller, 1999, p. 158). Damage to the frontal lobe portion of the brain can be a major concern, as the frontal lobe is considered our emotional control center and where our personality resides (Kolb & Milner, 1981, p. 507). There is no other part of the brain where lesions, or injury, can cause such a wide variety of symptoms (Kolb & Milner, 1981, p. 507). Cognitive functioning such as memory, attention, and speed of information processing can occur with brain injury, along with changes in personality (Miller, 1999, p. 157). Such changes in personality include the 2 lack of foresight, tact and concern, inability to plan ahead and judge the consequences of an action, an easily attained feeling of well-being, disinhibition, irritability, and a tendency to become verbally and physically aggressive (Miller, 1999, p. 158). It has been suggested that irritability and aggression could be a possible link with violent offending (Miller, 1999, p. 158). These changes in personality and behavior are what cause the major difficulty in successfully rehabilitating individuals with head injuries (Miller, 1999, p. 158). Two more features are significant in individuals with head injury. The first is significant head injuries are most commonly found in young adult males of lower socioeconomic status (Miller, 1999, p. 159). Second, there is an association between substance abuse and both head injury and offending (Miller, 1999, p. 159). Children are usually at more of a risk for head injury, as they engage in more physical activities such as sports and playing in general (Miller, 1999, p. 159). TBI is a leading cause of death and disability in children under the age of 15 (Miller, 1999, p. 159). Children that sustain a moderate or severe TBI in early childhood or infancy are more susceptible to having significant and ongoing cognitive impairments (Sonnenberg, Dupuis, & Rumney 2010, p. 1003). Evidence shows that elementary school children are at a higher risk of poorer social problems following TBI than teenagers (Sonnenberg et al., 2010, p. 1003). The brains of small children are at an earlier stage of development, as opposed to those of teenagers (Sonnenberg et al., 2010, p. 1004). Children suffering from severe TBI have more issues with social problem-solving and are said to be less socially competent and lonelier than children with injuries not involving the brain, and these social problems 3 persist over time (Sonnenberg et al., 2010, p. 1004). However, social problems with childhood TBI are not as understood as what is known for adult TBI (Sonnenberg et al., 2010, p. 1004). Research is quite limited on the effects of TBI in general, especially as it relates to criminal conduct, but it is extremely limited with respect to children (Sonnenberg et al., 2010, p. 1006). This limitation has led to professionals in the criminal justice system not knowing about TBI, let alone knowing how to treat the population of juveniles suffering from head injury. The Probation Department in Sacramento County, according to this researcher’s employment with said agency, has in recent years, implemented many programs to assist juveniles in institutions and the community with many different issues, and most of the programs have mental health components. Since little research has been done on the relationship between head injury and criminal behavior, professionals are not aware of the consequences of TBI, and questions are not asked regarding the presence of head injury, these programs do not focus on the specific and extraordinary needs of the juveniles. Professionals simply determine these juveniles to be the most aggressive and persistent. However, there may be factors that preclude these individuals from participating in the everyday form of treatment. As it stands, people with traumatic brain injuries face several challenges when trying to obtain treatment from substance abuse providers (Sonnenberg et al., 2010, p. 1006). Cognitive impairments may affect their learning style, which causes difficulty in participating in training and group interventions (Sonnenberg et al., 2010, p 1006). Problems with memory are usually perceived to be 4 resistance to treatment, and damage to the frontal part of the brain affects thinking skills, which leads to socially inappropriate behavior (Sonnenberg et al., 2010, p. 1006). There is an association between those within society who most often suffer head injury and those who most commonly participate in criminal activities, including those linked to violence (Miller, 1999, p. 159). Three major pieces of evidence exist. First, general neuropsychological studies of the consequences of head injury suggest changes that might precipitate offending (Miller, 1999, p. 159). Second, there are a small number of follow-up studies of the victims of head injury, which have recorded such things as arrests and convictions (Miller, 1999, p. 159). Third, there are a series of investigations of samples of violent offenders in prisons or special psychiatric facilities, which have attempted to estimate the frequency of brain injury (Miller, 1999, p. 160). This project will examine three assessment tools utilized by probation departments in the United States and determine if the tools address TBI amongst youth entering detention facilities. This project will also provide guidance in implementing possible treatment for TBI. Do local probation departments assess their clients for brain injury at the intake level? This question will be the basis of this project. This project will contribute to the rehabilitative efforts of the Probation Department in Sacramento County, as well as other criminal justice agencies. If these agencies become aware of such head trauma and/or brain injury, proper diagnosis and treatment can begin, as well as the proper classification and housing placement of juveniles in the detention facilities. This project will also provide an assessment tool that can be used by said probation departments as the basis for deciding which juveniles should be detained 5 in their detention facilities, where those detained juveniles should be housed, and the selection of treatment options in their future case plans. Most therapies used today, especially those based on evidence-based practices, are based on research that indicates these therapies are effective. They may be that much more effective if all is known about the behavior of the individual undergoing treatment. This project will provide evidence, through previous research stated in the literature review, that juveniles who have suffered head and brain injury, have also suffered a change in brain function, and in most cases, an inability to control those brain functions. Hopefully, attention will be given to this issue for the protection of injured juveniles, as well as the proper disposition of their cases and placement into evidence-based treatment. Purpose of the Project The purpose of this project is to examine the significance of assessing youth entering detention facilities for head injury, to inform probation officials about the issues that surround head and brain injury, and to develop an assessment tool for said officials to follow during their investigation. Probation officials should be notified of this information, as they are usually the first criminal justice agency, after arrest, to fully investigate cited or detained juveniles and their families. The assessment tool will promote the thorough examination of the circumstances surrounding the alleged violation of law and the overall behavior of the juvenile. Through this tool, the probation officer will be able to determine if a juvenile would benefit most from a clinical interview and diagnosis, possibly before continuing with the criminal process. The juvenile intake probation officer will guide the juvenile through the questions of the assessment tool and 6 note the answers to the questions. If an interview with the parents of the juvenile is possible, the juvenile intake probation officer will also guide the parents through the questions of the assessment tool and note their answers. If an initial interview is not possible with the parents, the assigned juvenile court probation officer will be responsible for contacting the parents and guiding them through the questions of the assessment tool and logging the answers. The focus for these officers will be to obtain as much information about the juvenile as possible to provide the best and most appropriate dispositional recommendation to the Court. Summary This chapter defined head injury and discussed some of the consequences of head injury and damage to the brain. Traumatic brain injury, being the most serious consequence of said injury was discussed, along with who is most at risk for injury. Children are at most risk, as they participate in activities that can result in injury. The purpose of this project is to examine the importance of head or brain injury assessment at the juvenile intake level, to enlighten probation officials about this information, and to provide guidelines to aiding those professionals in assessing for TBI. Chapter 2 will provide information on what is known about TBI. 7 Chapter 2 Review of Literature Introduction There are many social factors that contribute to the commission of violent acts, but there are other factors that may be beyond the control of the individual. Biological factors are possibly the most controversial factors that contribute to the commission of violent acts, and brain damage is one such factor that can occur due to head injury (Farrington, 1982, p. 10). The effects of head injury can be serious and life changing, as damage can occur to the brain, altering the thought process and behavior of the affected individual, as indicated in the previous chapter (Farrington, 1982, p. 10). Research is quite limited and no conclusions have yet been made linking violent behavior with head injury. However, research has been conducted on the brain functioning of individuals that were accused of violent acts and individuals that have suffered severe head trauma. Neurological consequences of said injury, such as low impulse control and the inability to control behavior in social situations will be discussed in the following review of the literature. The behavioral changes of individuals that suffer from head injury will also be reviewed, as well as possible treatment options. Neurological Consequences Since 1835, there have been case studies that have reported the onset of antisocial personality traits after injury to the frontal lobe of the brain (Brower & Price, 2001, p. 720). These personality traits typically involve damage to the orbitofrontal cortex of the brain, which causes a low level of impulse control, dangerously aggressive outbursts, 8 inappropriate verbal language, and decreased social sensitivity (Brower & Price, 2001, p. 720). The orbitofrontal syndrome is also called pseudopsychopathy, as it is similar to psychopathy, which is a type of personality disorder that is related to violence and criminal behavior (Brower & Price, 2001, p. 721). Another related syndrome is acquired sociopathy, which describes adults suffering from ventromedial prefrontal brain injury and who exhibit decreased functioning in judgment, decision-making in social environments, and decision-making regarding the consequences of their actions (Brower & Price, 2001, p. 721). In studying veterans of war that suffered head trauma, Brower and Price (2001) found a relationship amongst frontal lobe lesions on the brain and aggressive or antisocial behavior, but actual violent crime was rare (p. 721). A consistent relationship was found between orbitofrontal brain lesions and subsequent antisocial behavior (Blumer & Benson, 1975, p. 160). Five patients out of a sample of 144 British World War II veterans committed crimes, and all five had damage to the frontal lobe portion of their brains (Brower & Price, 2001, p. 721). The Vietnam Head Injury Study found that patients with brain lesions to their frontal lobes exhibited more aggressive and violent behavior, as opposed to patients with non-frontal head injury and the control group that had no head injury at all (Grafman, Schwab, & Warden, 1996, p. 1235). Out of the patients participating in this study with frontal lobe injury, 14% engaged in fights or damaged property, compared to 4% of the control group that had no head injury (Brower & Price, 2001, p. 721). The Vietnam Head Injury Study, using a brain CAT scan, found a compelling association between an elevated level of aggression and focal mediofrontal 9 and orbitofrontal injury (Brower & Price, 2001, p. 721). This study, along with other neuropsychological studies, supports the relation between the malfunction of the prefrontal executive portion of the brain and the high level of unsociable and aggressive behavior (Brower & Price, 2001, p. 722). The frontal lobe of the brain is involved in fine motor skills, problem solving, spontaneity, memory, language, initiation, judgment, impulse control, and social and sexual behavior; and it is extremely vulnerable to injury due to its location at the front of the head (Levin et al., 1987, p. 707). MRI studies have shown that the frontal area is the most common region of injury following mild to moderate traumatic brain injury (Levin et al., 1987, p. 707). Low frontal lobe function has been used to explain the actions and behaviors of accused and convicted violent offenders, and clinical observations of prefrontal network functioning suggests that damage to the frontal lobe may contribute to criminal behavior, especially violent criminal behavior (Brower & Price, 2001, p. 722). As stated, loss of consciousness over a period of time after a head injury can have major neurological consequences (Brooks, 1984; Richardson, 1990). Sonnenberg et al. (2010) conducted a study of children that suffered a TBI under the age of six years old (p. 1004). The children that were younger at the time of injury suffered socially, and their thinking abilities at the age of eight were significantly delayed compared to children that suffered injury later in life (Sonnenberg et al., 2010, p. 1004). In essence, the minds of children are always growing as they learn new things. Once the brain is injured, this growth can significantly decrease. Sonnenberg et al. (2010) concluded that social 10 impairments continued over time in the injured children, as their social deficits persisted (p. 1006). Studying the most serious and violent offenders gives the most compelling information regarding the correlation between head injury and offending, and Gibbens, Pond, and Stafford-Clark (1959) were the first to suggest such a correlation (p. 108). They performed a study of 72 extremely psychopathic offenders and 59 control offenders over an eight-year period after they were released from custody (p.110). It was stated that 29 members of the psychopathic group reportedly suffered a head injury at some point in their lives, and had many more added convictions during the eight-year time frame, which included violent offenses (Gibbens et al., 1959, p. 111). Three more studies were conducted on murderers, maximum-security mentally ill offenders, and males sentenced to death as juveniles, and a significant number of these offenders had previously suffered head injuries of sufficient severity (Blake et al., 1995, p. 1645; Lewis, Pincus, Feldman, Jackson, & Bard, 1986, p. 839; Martell, 1992, p. 880). Violent offenders may exhibit neurological malfunction or a history of TBI early in life, and they are also more likely to report such injury, especially in court proceedings to justify their behavior. However, the mere fact that their symptoms are being left untreated explains why they may have offended so violently or at all (Dinn, Gansler, Moczynski, & Fulwiler, 2009, p. 117). These individuals may not realize or comprehend the fact that they may have a serious brain dysfunction, and therefore do not seek treatment or assistance in controlling their behavior (Matthes & Caples, 2013, p. 126). It should be noted, however, research does not indicate that head injury will automatically result in 11 delinquent and/or violent behavior (Leon-Carrion & Ramos, 2002, p. 208). A large proportion of individuals who do suffer head trauma do not become violent (LeonCarrion & Ramos, 2002, p. 208). Head injury may lead to violent behavior in those individuals that are already at risk for such behavior due to their environment and family history, and brain malfunction due to head injury decreases the ability to deal with stressful situations, decision-making skills, and self-control (Leon-Carrion & Ramos, 2002, p. 209). The knowledge regarding brain mechanisms that are associated with the predisposition to violence is growing due to brain imaging research (Raine et al., 2001, p. 111). However, according to these authors, there are three significant issues regarding the knowledge of these brain mechanisms. First, information regarding the brain functioning of seriously violent adults that are not committed to an institution is unknown (Raine et al., 2001, p.112). Second, there are no studies published to assist with the understanding of why some people who have suffered severe physical abuse as young children do not commit serious violent acts (Raine et al., 2001, p.112). Third, violent offenders have not yet been studied using a process called functional magnetic resonance imaging (fMRI) (Raine et al., 2001, p.112). Raine et al. (2001) focused their article on the brain functioning of severely abused violent offenders, as physical child abuse and violence are related (Tarter et al., 1984; Lewis et al., 1986, p. 839). Henry and Moffitt (1997) and Raine (1993) found that, in two prior reviews using brain imaging, the majority of studies exhibited either frontal or temporal lobe deficits in violent individuals. In a few recent studies, researchers found reduced brain functioning (glucose 12 metabolism) in both medial temporal and prefrontal regions of the brain amongst individuals that have committed violent acts (Volkow et al., 1995; Raine et al., 1997; Raine et al., 2001, p. 112). However, these studies were conducted on individuals that were committed to institutions such as psychiatric hospitals and prisons, and many of these individuals suffered from schizophrenia (Raine et al., 2001, p. 112). It is difficult to study or determine a possible link between individuals that have suffered severe abuse and committed violent acts when the individuals also suffer from another mental illness. Past research has also stated two different findings regarding violent and antisocial individuals, which is that they have deficits in the right hemisphere of the brain or the left hemisphere (Moffitt, 1990; Pine et al., 1997; Raine, 1993; Raine et al., 2001, p. 112; Tarter et al., 1985; Volavka, 1995). The purpose of the Raine et al. (2001) study was to explore why some severely abused children go on to commit violent acts and some do not, and whether those that do not commit such offenses have better functioning in another part of the brain or just have no biological predisposition to violence as that of most abused violent offenders (p.113). In exploring this purpose, the authors also wanted to address the limitations of previous studies that included individuals with schizophrenia and the use of on-going activities that excessively favored the right hemisphere of the brain (Buchsbaum et al., 1990; Raine et al., 1997; Raine et al., 2001, p.113). Raine et al. (2001) recruited participants in their study about the decrease of right hemisphere activation in severely abused and violent offenders and hired them from temporary employment agencies in Los Angeles, California, as it was stated these individuals commit many violent acts (p. 113). Individuals were excluded if they were 13 20 years old and younger or 46 and older, were not English-speakers, suffered from a psychotic disease and epilepsy, had poor vision, feared small environments, or had metal devices implanted in their bodies, and this left a sample of 23 individuals (Raine et al., 2001, p.114). The history of serious violence, an act that caused bodily injury/trauma or was life-threatening, and a history of severe physical childhood abuse (elementary school age) was retrieved from self-report interviews (Raine et al., 2001, p.114). The 23 individuals were broken up into four groups by the degree of serious violent offending and severe physical abuse. The groups consisted of a group with no abuse or violence, a group exhibiting violence, a group that had been abused, and a group that had been abused and exhibited violence (Raine et al., 2001, p.115). The participants were given a memorization activity using sight and words, an activity to recall memory, a questionnaire measuring cognitive functioning during an activity, and a questionnaire measuring approaches to completing activities (Raine et al., 2001, p.115). A 1.5-T Philips MRI system was used to obtain pictures of the participant’s brains as they performed the tasks (Raine et al., 2001, p.115). The data were uploaded into SPSS and analyzed (Raine et al., 2001, p. 118). The major finding of the Raine et al. (2001) study was that seriously violent individuals that suffered severe childhood abuse exhibited lower functioning in the right hemisphere of their brains during the visual/verbal working memory task (p.124). These authors also found that severely abused individuals, whether they were violent or not, exhibited cortical activation to the working memory task, which was in the left hemisphere of the brain (Raine et al., 2001, p. 124). Third, the authors found that the 14 severely abused individuals that did not become violent exhibited good right hemisphere (temporal) functioning of their brains, but poor left hemisphere (temporal) functioning (p.124). Low functioning in the right hemisphere of the brain may possibly lead people to commit violent acts, as this area of the brain deals with emotion and can make these individuals have no feeling when it comes to the distress felt by victims (Raine et al., 2001, p. 124). In essence, these individuals will not feel compassion or be aroused by the suffering of their victims or victims in general, which can lead to continued criminal behavior. This idea of low arousal is believed to be the reason why these individuals seek attention and more excitement (Raine et al., 2001, p. 124). In conclusion, one can conceive that menacing criminal behavior is related to right hemisphere brain disturbance at a young age, along with damage to the left hemisphere of the brain later on in life, and these findings suggest that individuals that have been severely physically abused early on in their lives may have left temporal brain dysfunction because of said abuse (Raine et al., 2001, p.124). The major limitation of the Raine et al. study (2001) is the fact that the researchers used self-reported information, which can be fabricated or altered by the individual offering the information, while previous studies used information from official records and studied individuals already committed to institutions for their violent acts (p. 124). According to Antonucci et al. (2006), the combination of multiple biological factors is assumed to control aggressive behavior on a neurobiological basis (p. 214). These factors are lesions on the brain, neurophysiological malfunction, and neurochemical systems (Antonucci et al., 2006, p. 214). When a person loses control of 15 their ability to make sound decisions, along with the failure of meeting social, scholastic, and employment expectations, the dorsolateral prefrontal cortex of the brain malfunctions and creates a tendency for violence (Antonucci et al., 2006. p. 214, Brower & Price, 2001; Giancola, 1995). These dysfunctions can be impulsivity, difficulty in considering alternatives, and the inability to produce courses of action (Antonucci et al., 2006, p. 214). Impulsivity is a critical aspect that controls the relationship between orbitofrontal cortex malfunction and aggressive behavior (Brower & Price, 2001, p. 722). The frontal lobe is involved in and necessary for the ability to reason in social situations (Antonucci et al., 2006, p. 215). Volavka (1999) posed the view that violence can occur two ways, one being through a genetic prefrontal problem surrounding impulsivity, and the second being raised in an abnormal and deviant atmosphere, which can cause violence through a lack of temporal lobe volume (p. 214). Current Causes of Traumatic Brain Injury The following sections will discuss ways that individuals in current times are acquiring traumatic brain injuries. In recent years, attention has been focused on head injuries acquired while playing football. Also, the current wars in Iraq and Afghanistan have prompted research due to the number of head injuries reported. Studying head injuries in professional football contributes to the understanding of what could happen while children are participating in the sport at young ages. As stated above, children are prone to acquiring a TBI, as they participate in more activities, such as sports. If adults are suffering major brain damage from repeated concussions, then a child, with a growing brain, would probably suffer a worse fate while participating in the sport of football. 16 These children could then have significant changes in their behavior, which could lead to criminality. Studying the current military head injuries just allows for further understanding of the basic issues and causes of TBI amongst young adults. Research on childhood TBI is quite limited, but studying TBI in adults allows for the basic understanding of the changes in the brain after injury. Football Injury. Sports-related head injuries have recently received a great deal of attention due to the number of suicides committed by retired and current football players, as well as the lawsuits entered against the National Football League (N.F.L.) and the National Collegiate Athletic Association (N.C.A.A.) (Nocera, 2012, p. A23). All contact sports are of concern due to the risk of injury, but attention has been focused on the game of football and the number of concussions football players suffer in the course of their careers (Nocera, 2012, p. A23). Repeated concussions, or mild traumatic brain injury (mTBI), are related to depression and cognitive dysfunction, which are symptoms of a disease in the brain called Chronic Traumatic Encephalopathy (C.T.E.) (Nocera, 2012, p. A23). Research conducted by Kevin Guskiewicz, professor at the University of North Carolina, about the damage that can occur to football players after multiple concussions was used to encourage the N.F.L. to find a way to make “the kickoff” play in the game safer (Nocera, 2012, p. A23). The “kickoff” is said to be the most dangerous play in the game where the most serious injuries occur due to the momentum gained by the defensive team running from downfield, and in response to these injuries, the N.F.L. moved the kickoff line from the 30-yard line to the 35-yard line for the 2011 season 17 (Battista, 2012, p. SP1). This simple change dropped kickoff injuries by 40% in that season compared to the previous seasons (Battista, 2012, p. SP1). C.T.E. is a disease of the brain that accelerates in its deterioration and is found in people with excessive brain injury, such as athletes (McKee et al., 2009, p. 720). Concussions and severe blows to the head are examples of such excessive brain injury, which is interesting when thinking about how many times football players hit each other on the head or helmet in celebration of a successful play (McKee et al., 2009, p. 720). In 1928, Martland announced the concept of C.T.E. with the use of the description, “punchdrunk” relative to a person being repeatedly hit in the head (Martland, 1928, p. 1103; McKee et al., 2009, p. 710). This term was originally introduced for professional boxers; however, C.T.E. has recently been confirmed in athletes that have retired from their sports, especially football players with a history of concussions (McKee et al., 2009, p. 720). This head trauma activates the deterioration of the tissue in the brain and causes advanced growth of a protein in the brain called tau (McKee et al., 2009, p. 720). This activation can occur years after the head trauma or years after the football player has discontinued playing (McKee et al., 2009, p. 720). Once tau builds up in the brain, it forms in clusters in places where it is not normally stored, which causes dysfunction in the brain (Zeigler, 2012, p. 1). At onset of C.T.E., the player can have symptoms such as attention deficits, problems concentrating, memory loss, confusion, dizzy spells and headaches (McKee et al., 2009, p. 710). As the disease progresses, the player can experience more symptoms, such as impaired judgment, dementia, and the lack of intuitiveness (McKee et al., 2009, 18 p.710). Severe C.T.E. can cause the advanced decrease of movement of the muscles, an unsteady walk, deafness, trembling, and loss of equilibrium (McKee et al., 2009, p. 711). There are three stages of scientific degeneration, and the first deals with psychotic symptoms and emotional disturbances (Mckee et al., 2009, p. 711). The second stage is characterized by loss of memory, initial signs of Parkinson disease, imbalance in social situations, and unpredictable behavior (McKee et al., 2009, p. 711). The third and final stage is characterized by mental impairments that lead to dementia and possible actual Parkinsonism, along with walking and verbal irregularities (McKee et al., 2009, p. 711). The seriousness of C.T.E. is gauged by how long the football player performed the sport and how many concussions, known or otherwise, he has suffered (McKee et al., 2009, p. 711). This disease continuously progresses even after more than ten years have passed after the original injury occurred or after injurious activity is discontinued, and this fact is one of the main aspects of C.T.E. (McKee et al., 2009, p. 719). It is unknown, however, whether one concussion can jump start the onset of C.T.E. or if it takes recurring concussions (McKee et al., 2009, p. 711). In 2009, there were 51 cases of C.T.E. that were confirmed, and the majority of those cases were athletes (39 boxers, 5 football players, 1 wrestler, and 1 soccer player) (McKee et al., 2009, p. 711). All of the five football players abruptly died between the ages of 36 and 50, which was earlier than the boxers with confirmed C.T.E. (McKee et al., 2009, p. 711). Interestingly, all five football players were lineman, offensive and defensive, and their symptoms ranged from depression and episodes of paranoia to violent outbursts, which resulted in three suicides, one fatality after a high-speed chase 19 with police, and one gunshot wound to the chest (Omalu et al., 2005, p. 129; Omalu et al., 2006, p. 1087). The latter was 45 years old when he died and had a long career playing football, beginning in high school and ending with his retirement from the N.F.L. (McKee et al., 2009, p. 712). He suffered 11 concussions throughout college and professional football, but only one of the concussions was confirmed (McKee et al., 2009, p. 712). This fact is interesting, but not uncommon. Players want to get back in the game, and team staff members do not force the players to sit out in observation, so symptoms after the concussion go unrealized and unreported (McKee et al., 2009, p. 713). Dr. Robert Cantu, co-director of the Boston University Center, stated in the New York Times that previously in the N.F.L., team doctors missed the signs and warnings of concussions, so players without a recognized history of concussion could have still suffered such injury (Nocera, 2012, p. A23). Confirmed concussions are not the only concern, it is all of the constant pounding and brain trauma that occurs in the game of football that worry researchers and medical staff (Nocera, 2012, p. A23). In the spring of 2012, a very famous N.F.L. linebacker that retired in 2006 and was diagnosed with C.T.E., committed suicide by shooting himself in the chest (Pilon & Belson, 2013, B13). This well-known player became the main player associated with C.T.E., as he was diagnosed with the disease, and his death plagued the N.F.L., with research studies surfacing that exhibit the potential lasting effects of blows to the head received on the playing field (Pilon & Belson, 2013, B13). This player’s family allowed his brain to be studied after his death, and small amounts of the tau protein were found in many areas of his brain, which indicates that this player was suffering and may not have 20 really known why (Pilon & Belson, 2013, B13). Unfortunately, it can only be determined that a person has C.T.E. by studying their brain after their death (Pilon & Belson, 2013, B13). Among the 34 brains of formal football players in the N.F.L. that were examined, 33 were confirmed to have had C.T.E. (Pilon & Belson, 2013, B13). In Nocera’s article in the New York Times, Should Kids Play Football? (2012), it was stated that the brains of children are still growing and are more fragile (p. A23). There is still a great deal of information about C.T.E. and the effects of the game of football as it relates to said disease that is unknown, but this should be all the more reason why parents should think about allowing their children to play (Nocera, 2012, A23). Guskiewicz is one researcher that feels the proper techniques of blocking should be taught to the children to keep them safer and protect their heads (Nocera, 2012, A23). This way, as they progress to the high school levels and beyond of football, they will be more educated about the game and a little more protected (Nocera, 2012, A23). It was also stated that maybe children should play flag football until they reach the age of 14, which would give their vulnerable brains more of a chance to develop (Nocera, 2012, A23). Fortunately, it is known that repeated concussions can cause C.T.E., but at this point, it is not known how much trauma can occur before the development of this disease begins amongst football players (Nocera, 2012, A23). Therefore, the question of whether children should play football cannot scientifically be answered at this point. Military Injury. The continued issues in Iraq and Afghanistan over the past several years have generated a new class of United States soldier that is suffering from head trauma, resulting in brain injury (Carlson et al., 2011, p103). Falling and vehicle 21 accidents usually result in the majority of TBI cases, but since Operation Enduring Freedom and Operation Iraqi freedom have been underway, blast injury has been another cause of TBI (Carlson et al., 2011, p. 103). Blast injury is due to explosions and forces that cause the head to hit something, or for an object to hit or penetrate the head (DePalma et al., 2005, p.1335). Approximately 23 percent of the soldiers serving in the above operations have suffered a TBI, and in most cases, the injury was mild (Carlson et al., 2011, p. 103; Miller et al., 2013, p. 31). Six months is the usual amount of time the majority of individuals suffering from a mild TBI take to recover; however, there are many patients that continue to deal with physical and emotional symptoms, not to mention issues regarding their conduct, after that initial six months (Carlson et al., 2011, p. 104; McCrea, 2007; McCrea et al., 2009, p. 1369; Miller et al., 2013, p. 31; Ruff, 2005, p. 6). The amount of pain and suffering a person endures from a mild TBI after six months post-injury has not been thoroughly studied, but the severity of the injury is believed to be the reason why symptoms last so long (Miller et al., 2013, p. 31). Most of the information on this topic comes from studying sports injuries, and different findings have been discovered. Some studies showed that symptoms did not increase with football players sustaining two TBIs as opposed to one (Miller et al., 2013, p. 32). However, another study discovered that football players that suffered multiple concussions in one season, had an increased amount of symptoms, as opposed to players that suffered just one concussion (Collins et al., 1999, p. 968; Miller et al., 2013, p. 32). Miller et al. (2013) suggested football players may fear getting removed from the game 22 and are probably less likely to make their post-concussive symptoms known (p. 36). The symptoms soldiers have after sustaining the TBI are related to other serious issues that are common for soldiers such as PTSD (Miller et al., 2013, p. 36). War veterans from Iraq and Afghanistan reported having constant post-injury symptoms, PTSD, and severe pain occurring altogether Miller et al., 2013, p. 36). To study this concept relative to soldiers, Miller et al., (2013) gave questionnaires to 2,337 soldiers that were active in the United States Army from 1999 to 2000, and were mostly paratroopers (p. 32). It was discovered that having a history of just one mild TBI could determine if a soldier would have more symptoms after his injury (Miller et al., 2013, p.36). Medical staff should make every effort to obtain the patient’s previous medical history. Also, it was discovered that post-injury symptoms were worse for soldiers that suffered more than one TBI (Miller et al., 2013, p. 37). Treatment of Brain Injury Treatment of brain injury begins and is centered on two separate time frames, which are primary brain injury and secondary brain injury (Haddad & Arabi, 2012, p. 12). The primary brain injury deals with the trauma to the brain tissue and blood vessels during the incident (Haddad & Arabi, 2012, p. 12). Secondary brain injury can occur during the hours and days following initial injury and can occur as an intracranial, extracranial, or systemic injury (Haddad & Arabi, 2012, p. 12). Hematomas, infection, hypertension, calcium ion toxicity, and seizures are examples of intracranial and extracranial injury, whereas hypotension, hypertension, hypoxemia, anemia, hypoglycemia, fever, and hypothermia are examples of systemic brain injury (Haddad & 23 Arabi, 2012, p. 12). Interestingly, the initial (primary) injury or head trauma only causes some of the damage to the brain, and this injury cannot be reversed, but secondary injury can be avoided and possibly treated (Haddad & Arabi, 2012, p. 13). During the critical time after the primary injury, stabilization and continuous monitoring is imperative to avoid any further damage to brain tissue and functioning (Haddad & Arabi, 2012, p. 13). Being that the extreme damage to the brain cannot be repaired, the primary goal of treatment of brain injury is to attempt to restore as much brain functioning as possible (Haddad & Arabi, 2012, p. 13). Unfortunately, TBI causes about 52,000 deaths each year in the United States and is one of the leading causes of death and impairment amongst youth (Harrison-Felix et al., 2012, p. E69). Research on TBI among children is quite limited, as is information on treatment of adolescents suffering from TBI. The following information on treatment is used for youth and to understand exactly the best way to treat youth. To determine how long a person suffering from a TBI will live or what type of treatment or care is needed, the rates and causes of death need to be completely explored and figured out (HarrisonFelix et al., 2012, p. E69). According to a study in 2004 regarding rate of death and how long a brain injured individual would live, it was found that the rate of death of TBI patients was twice that of individuals dying from other causes (Harrison-Felix et al., 2004, p. 50). Also, the life span of the injured person was reduced by seven years (Harrison-Felix et al., 2004, p. 50). It appears that most of these deaths, resulting from seizures, septicemia, pneumonia, and respiratory conditions, occur early on after the injury, but the rate of death lessens over time (McMillan et al., 2011, p. 932). There is 24 also a strong relationship between increased disability and reliance on others for care and death rates and how ill a TBI patient becomes (Baguley et al., 2012, p. 42). It appears that people suffering from a TBI, especially one that is more severe, may feel more depressed about how sick they are and how they have to rely on family and friends to just complete simple everyday tasks, which in turn hinders their recovery. Harrison-Felix et al. (2012) indicated that how the injury occurred, type of injury, demographic information, drug abuse, medical status, whether insurance was an issue, and recovery process were all causes of a shortened life span after TBI (p. E70). In their 2012 analysis, these authors found, out of 8,573 people treated for TBI, a 9.8% rate of death, coupled with an average time of 3.5 years from the time their injury occurred to their demise (p. E71). Interestingly, 23% of the deceased individuals lost their battle during the rehabilitation phase of recovery, which is up to one year after they were injured (Harrison-Felix et al., 2012, p. E71). The patients that died were said to have been older and acquired TBI from falling down, which resulted in a longer time spent in the hospital (Harrison-Felix et al., 2012, p. E71). It is much harder to recover when a patient is older and other health concerns weigh in to the equation. This group of patients, along with patients injured during a violent situation, had a much higher risk of dying after injury than patients suffering a TBI from a vehicle accident (Harrison-Felix et al., 2012, p. E73). Interestingly, circulatory conditions, such as heart disease, were also a cause of a great deal of deaths among TBI patients in recovery, as well as extrinsic or outside causes of injury such as accidental poisonings and vehicular injuries (Harrison-Felix et al., 2012, 25 p. E75). Respiratory problems, such as pneumonia, were the next largest group of deaths that occurred during recovery of TBI (Harrison-Felix et al., 2012, p. E75). Patients suffering from TBI were 33 times more likely to pass away from seizure related deaths than people with no injury, which is not surprising due to the cognitive injury (HarrisonFelix et al., 2012, p. E75). TBI patients were also 13 times more likely to expire from fluid inhaled into the lungs, 10 times more likely from wound infection, poisoning, or falling, six times more likely from pneumonia, four times more likely from outside forces or homicide, three times from emotional, behavioral, or nervous disorders, two times from suicide, and finally 1.3 times from blood circulation disorders (Harrison-Felix et al., 2012, p. E75). Many of these causes of death require continued investigation in order to be able to treat TBI patients in the recovery stage. Seizure-related deaths after TBI have been a persistent problem; however, there still appears to be a lack of knowledge about why such severe seizures occur and how to prevent them post-injury (Harrison-Felix et al., 2012, p. E77). It is also unknown how fluid is inhaled into the lungs, which causes aspiration pneumonia (Harrison-Felix et al., 2012, p. E78). It was believed that there was possibly a degenerative weakening in the nervous system that enabled the intake of fluid, which also left these patients in a severe disabled state (Harrison-Felix et al., 2012, p. E78). Most importantly, dangerous behavior, hostility, hindered comprehension, a change in awareness and understanding, and drug abuse can cause some TBI patients to commit murderous acts, which ultimately infringes on the lives of others (Harrison-Felix et al., 2012, p. E78). The change in aggression and the inability to control one’s impulses 26 after TBI is of extreme concern, but needs more research (Harrison-Felix et al., 2012, p. E78). It should be apparent that more development of treatment options needs to occur to keep individuals from hurting others merely because they cannot control their emotions and actions due to those emotions. Currently, the main treatment for TBI symptoms is the use of medication such as sedative-hypnotic chemicals, which help a person sleep and deal with tension and anxiousness, and antidepressants (Zollman et. al., 2012, p. 135). However, these drugs have side effects that can cause more symptoms with regard to the TBI such as memory loss, drowsiness during the daytime, psychological problems, seizures, and sleeplessness (Flanagan, 2007, p.68; Larson & Zollman, 2010, p. 62; Zollman et al., 2012, p. 136). These medications can also negatively affect the patient’s ability to successfully participate in a restoration program, as well as decrease the ability for molding and recovery of the brain, which is a long-term effect (Zollman et al., 2012, p. 136). Ultimately, medications can exacerbate the damage of TBI, and cause added symptoms that confuse the diagnosis and treatment providers. Zollman et al., (2012) studied acupuncture as a means to treat insomnia, which is only one symptom of TBI, as it has been an effective treatment for patients suffering from other illnesses such as stroke, and has little to no side effects or that can worsen the TBI (p. 136). Insomnia is an enormous problem for those suffering from a TBI (30%80%), and can remain so from one day to many years post-injury (Zollman et al., 2012, p. 135). Insomnia is a difficulty in falling asleep and staying asleep for more than 30 minutes at a time at least three times throughout the week, which hinders the patient’s 27 effectiveness during the day (Zollman et al., 2012, p. 135). Insomnia can be an extreme problem for youth with school and the many activities in which they participate. This disruption in the patients’ sleeping ability is due to the damage to the brain occurring during the initial injury, as well as the events that occurred post-injury (Thaxton & Patel, 2007, p.559). Acupuncture is a treatment that uses the method of piercing the patient’s skin with hard, but thin, metal needles, and this process can be administered by human or machine (Zollman et al., 2012, p. 136). Acupuncture can be seen as a form of sedation and relaxation, as it activates the body’s nervous system so that hormones and chemicals can be released in the brain, muscles, and spinal cord to regulate the body (Zollman et al., 2012, p. 136). In their study, Zollman et al. (2012) recruited 24 participants that suffered a TBI five years or less prior to the study, and they all wrestled with insomnia (p. 136). Participants were separated into a group that underwent acupuncture treatment and a control group. Those in the treatment group were gradually released off of their medication in the first week of treatment, but had no differences in the amount of time they were able to sleep when compared to the control group (Zollman et al., 2012, p.140). However, those in the treatment group experienced an improved feeling about the quality of their sleep, which is in line with the belief that an altered perception of sleep and sleep time is what maintains the sleeplessness (Zollman, et al., 2012, p. 140). If a treatment can improve the patients’ feelings about their sleeping pattern and quality, then the insomnia can cease, which is what occurred in the Zollman et al. (2012) study. This improved feeling of sleep lasted for one month after the acupuncture treatment, and the 28 control group did not experience this change in perception with their medication (Zollman et al., 2012, p. 141). The results of this study also showed improvement in brain function with the acupuncture treatment; however, the reason was unknown since the amount of sleep was unchanged and the same as the control group (Zollman et al., 2012, p. 141). Therefore, it was believed that acupuncture had a positive effect on insomnia and brain functioning in individuals suffering from a TBI (Zollman et al., 2012, p. 141). Another form of treatment used with people suffering from severe TBI is deception. Severely injured individuals can suffer major changes in personality, mental state, and conduct, which can cause aggressive fits of temper (Matthes & Caples, 2013, p. 126). These changes occur with juveniles as well and can be due to the mental deterioration caused by the injury, as well as the fact that the injured person is unaware of the deterioration and damage they have suffered (Matthes & Caples, 2013, p. 126). This behavior can become a problem for treatment and rehabilitation providers, even with the utilization of medication, because the injured person is not convinced there is a problem that warrants therapy (Matthes & Caples, 2013, p. 126). Matthes and Caples (2013) discussed an adult male in his late 30’s that suffered a severe TBI due to falling from a moving vehicle approximately four years prior to the study, and was in a coma for more than one month (p. 126). When he healed from his physical injuries, he was sent home with serious mental and behavioral problems (Matthes & Caples, 2013, p. 126). He was a high school graduate with no learning problems, husband, and father, but was now on disability and needed care all day long for 29 his own well-being (Matthes & Caples, 2013, p. 126). He continued therapy on an outpatient basis, but did not know basic things such as how many months were in a year and his age (Matthes & Caples, 2013, p. 126). He also had verbal and visual impairments and was eventually placed in an adult treatment facility for patients with TBI because his wife feared for the safety of their children due to his aggressive fits of temper; however, he was removed from this program for the same behavior and attacking a staff member (Matthes & Caples, 2013, p. 126). This patient began having more problems and deterioration in the brain, as well as changes in walking and standing, so he underwent surgery and inpatient rehabilitative care to protect him from falling and suffering further injury (Matthes & Caples, 2013, p. 127). His rehabilitation and therapy continued to suffer due to his aggression and uncontrolled denial of disability, so his wife and therapists agreed to make the patient believe he would now be working at the rehabilitation center helping staff, but only if he completed his therapy every day, took his medicine, and was not threatening or assaultive (Matthes & Caples, 2013, p. 128). The patient previously indicated to therapists that he wanted to go home and take care of his family and save money for his children, so therapists told him that if he did what he was supposed to and remained professional on the “job”, he would receive his salary, which was supplied by his wife (Matthes & Caples, 2013, p. 128). The patient agreed and asked for the money to be placed in a bank account for him (Matthes & Caples, 2013, p. 128). This deception brought up many ethical issues about misleading patients with cognitive deficits and not building trust between medical staff and the patient (Matthes & 30 Caples, 2013, p. 128). However, deception can be justified and acceptable when all other therapies have been tried and have failed, especially when trying to get past their understanding of nothing being wrong with them in order to medically treat them and keep them safe (Matthes & Caples, 2013, p. 129). In this instance, consent was given by his wife, and the patient’s cognitive injuries were so profound that he was not allowing treatment and recovery to occur because of his inability to believe he had a disability (Matthes & Caples, 2013, p. 129). His condition was worsening, so a creative approach was the best option. Deception worked in regard to this patient, as his behavior improved because he felt he was actually working instead of being a patient (Matthes & Caples, 2013, p. 129). The idea of his employment continued in the next rehabilitation facility, and his condition continued to improve, while risk and harm to the patient and caregivers was decreased (Matthes & Caples, 2013, p. 129). Treatment of C.T.E. Causes. Unfortunately, this disease has not been studied in great detail, as the brain tissue of affected individuals is only available to study after the individual is deceased, as previously stated. There is still much to learn about C.T.E., and there are still many questions that need to be answered before the pathology of this disease can be understood such as: How many concussions cause C.T.E.? How severe do the concussions have to be? How many years after the concussion does C.T.E. develop? (Zeigler, 2012, p. 2). The sole duty of the Center for the Study of Traumatic Encephalopathy (CSTE) is to conduct the necessary research to determine and understand the pathology of this disease, and once the disease is further understood, protocols to prevent and treat C.T.E. can be established (Zeigler, 2012, p. 2). At this point, it is 31 known that head or brain trauma can cause C.T.E., so prevention efforts have begun by giving proper diagnoses, paying closer attention to the athletes that have suffered concussions, and following the recommendations set for when the athlete can return to play (Zeigler, 2012, p. 3). Presently, it is recommended that an athlete that has sustained a concussion be subjected to a progressive increase in activity following the injury, which will begin with a minimum level of exercise and end with full activity (Zeigler, 2012, p. 3). The athlete cannot have any symptoms of the concussion while he or she is at rest to be able to proceed through the post-injury exercise phase (Zeigler, 2012, p. 3). The minimum amount of time for this exercise phase is five days, but can last as long as the athlete needs to properly recover from the concussion (Zeigler, 2012, p. 3). These guidelines do not allow for the affected athlete to continue playing the same day as his injury, which has been the common practice in football for many years. The athletes want to finish the game and strive to attain the victory by any means necessary, especially professional athletes that have their careers to consider. While ongoing research is conducted regarding C.T.E., several bills have been passed to protect young athletes from head trauma and concussions. California, New York, and Massachusetts are three states where such bills were presented (Zeigler, 2012, p. 3). These bills do not allow the athlete to return to the game on the same day as his concussion, but mandate that he receives medical clearance before returning to play. The bills also provide information and training for team staff, parents, and athletes regarding the negative consequences and outcomes of not properly dealing with the concussion (Zeigler, 2012, p. 3; Abel, 2010). 32 Treatment of Military Causes. The issue of TBI amongst the soldiers in Operation Enduring Freedom and Operation Iraqi Freedom has sparked a great deal of interest in the recovery and rehabilitation of brain injured veterans. Health care providers for the Department of Defense and the United States Veterans Health Administration have focused the most attention on diagnosing mild TBI early so that appropriate care can be administered at the initial stages of injury (Carlson et al., 2011, p. 104). One of the issues with diagnosis and effective treatment of soldiers is the confusion of the symptoms for mild TBI and Posttraumatic Stress Disorder (PTSD) (Bryant, 2001, p. 932; Carlson et al., 2011, p. 104; Stein & McAllister, 2009, p. 768). PTSD is a disorder based on worry, fear, and tension that forces an individual to relive, try to avoid, or become extremely provoked due to experiencing a traumatic event (Carlson et al., 2011, p. 104). PTSD amongst soldiers that fought in the war in Iraq was reported at a rate of 1.4% to 31%, but for soldiers immersed in more war action, the rates were more constant at 10% to 17% (Carlson et al., 2011, p. 104; Sundin et al., 2010, p. 368). Intense worrying, sleeplessness, problems with cognitive and memorization skills, annoyance, rage, and assaultive behavior are all possible outcomes of PTSD, as well as mild TBI, which caused controversy with regard to the extent of their uniqueness (Carlson et al., 2011, p. 104). The individual would have to remember the triggering event in order to have PTSD, but in extreme cases of TBI, the individuals could have no memory of said event (Bryant, 2001, p. 935; Bryant & Hopwood, 2006, p. 19; Carlson et al., 2011, p. 104). Evidence shows that individuals suffering from TBI can also exhibit symptoms of PTSD from remembering their injuring traumatic event or as a consequence of another 33 event in their lives (Carlson et al., 2011, p. 104). Although there are numerous ways to treat PTSD, such as with medicine and/or counseling, one of the best has been through cognitive-behavioral therapy (CBT), which is also true for TBI (Carlson et al., 2011, p. 104; Foa et al., 2008, np). However, there are symptoms of TBI that can interfere with the injured individual’s participation and the effectiveness of treatment through evidencebased practices, such as disadvantages in brain function, pain, and the inability to control his impulses (Carlson et al., 2011, p. 104; Bryant & Hopwood, 2006, p. 19). Carlson et al. (2011) reviewed a study involving 24 civilian males and females that analyzed the success of CBT with patients suffering from traumatic stress and TBI (p. 110). The individuals participating in the study experienced severe motor vehicle crashes or assaults and were separated into a supportive-therapy group or a CBT group (Carlson et al., 2011, p. 110). The supportive-therapy consisted of skills to assist the individuals in learning to effectively deal with their problems and to become familiar with the changes in their brain functioning (Carlson et al., 2011, p. 110). The CBT consisted of brain function awareness, as well as loosening and resting of the muscles, rearrangement of emotions, the introduction of made up traumatic event scenarios, and the display of provoked responses the injured patients have been avoiding since injury (Carlson et al., 2011, p. 110). With the CBT group, as studied right after treatment, the prevalence of PTSD was less after treatment than that of the supportive-therapy group, and these results remained true six months after treatment (Carlson et al., 2011, p. 110). In essence, CBT reduces and prevents PTSD symptoms in individuals that have suffered TBI, which is a significant finding in the efforts to treat said injury (Carlson et al., 2011, p. 110). It 34 appears that teaching people about their injury, the changes the brain makes, exposing them to trauma, and re- teaching them how to deal with that trauma, improves their symptoms and recovery almost immediately (Carlson et al., 2011, p. 110). PTSD is a significant issue with individuals that have experienced TBI, and amongst United States soldiers that have experienced war, with rates of 10% to 40% (Carlson et al., 2011, p. 111). The best way of screening for TBI is through clinical interview; therefore, it is imperative that clinicians, especially when screening veterans, pay close attention to the extreme chance that these soldiers may also suffer from PTSD (Carlson et al., 2011, p. 111). Recently, there have been many veterans returning from Operations Enduring Freedom and Iraqi Freedom with TBI and a high preponderance of PTSD (Carlson et al., 2011, p. 111). With the current length and state of war amongst United States soldiers, it is imperative that further studies occur regarding the relationship between TBI and PTSD to further develop treatment and recovery of brain-injured individuals (Carlson et al., 2011, p. 112). The development of social relationships and the ability to obtain and keep employment by injured individuals hinges on the evaluation of rehabilitative efforts in this area (Carlson et al., 2011, p. 112). It is very difficult to treat an individual for TBI when they suffer from other symptoms and issues that are unknown to clinicians (Carlson et al., 2011, p. 112). Behavioral Changes Four follow-up investigations were conducted on head injury victims that reported information on offending. One of the investigations, by Brooks et al. (1986), compared relatives’ reports at five years with similar information obtained at one year after head injury (p. 35 765). At both time frames, about two thirds of the relatives reported their family member exhibited irritability and had a bad temper (Miller, 1999, p. 160). Threats of physical violence, actual physical violence, and trouble with the law, on behalf of the injured family member, increased after five years (Miller, 1999, p. 160). Kreutzer et al. (1991) surveyed 74 cases with a past head injury that were examined again approximately six years after their injury (p. 178). There was a significant decrease in arrests after injury; however, the people in this investigation were extreme alcohol and drug abusers, which is a significant limitation of this study (Miller, 1999, p. 161). Alcohol and drug abuse has also been reported to have a connection with offending, and since these cases decreased their use of said substances, their rate of arrests declined (Miller, 1999, p. 161). Hall et al. (1994) conducted an investigation using a six-month and two-year follow-up period. Approximately 50% of the injured individuals were reported by their caregivers to have irritability at both time frames, but their outbursts increased (Miller, 1999, p. 162). It appears that their aggressive behavior increased over time after head injury (Miller, 1999, p. 162). Additionally, as stated in the investigation by Hall et al. (1994), the level of arrests and incarceration increased in the injured individuals (p 880). The final investigation was conducted by Kreutzer et al. (1991), and they were interested in the relationship between substance abuse, crime, and aggression after injury (p. 180). These authors’ sample consisted of 327 cases, with a follow-up period of approximately two years (p.180). Kreutzer et al. (1991) found that there was also a decline in arrests and convictions at the two-year mark, which was also believed to be due to a decline in alcohol use (p.185). The findings of these investigations were mixed, but this was 36 believed to be due to the way the investigations were conducted (Kreutzer et al., 1991, p. 186). Delinquent children engage in even more at-risk behavior, such as fighting and gang activity, that can result in serious injury. Perron and Howard (2008) conducted a study and interviewed 720 residents at 27 facilities within the Missouri Division of Youth Services, and these residents were assessed for TBI where they were unconscious for more than 20 minutes, screened for substance abuse and psychiatric symptoms, and assessed for antisocial traits or behaviors (p.250). The results reported 18.3% of the residents stated they previously suffered a TBI, and these residents were more likely to: be boys, have received a mental diagnosis, report an earlier onset of criminal behavior or substance abuse, previously commit crimes, exhibit suicidal behavior, not be able to control their impulses, be unafraid, be victimized, and have a tendency to let others control their actions (Perron & Howard, 2008, p. 250). These authors concluded that youth that have suffered traumatic brain injuries were at a greater risk for depression, anxiety, antisocial behavior, and substance abuse (p. 250). Aggression can lead to altercations in life, which may result in physical acts that break the law (Dooley, Anderson, Hemphill, & Ohan, 2008, p. 837). Physical aggression in childhood can strongly predict adolescent violent delinquency, which may only be true for a small number of children (Dooley et al., 2008, p. 837). The presence of aggression after injury can hinder the injured individual and lead to adversity with friends, in education, and in the workplace, especially for children with TBI (Dooley et al., 2008, p. 837). 37 Dinn, Gansler, Moczynski, and Fulwiler (2009) indicated that a large number of closed head injury patients showed aggressive behavior during the initial post-injury period, and frontal lobe injuries were related to aggression (p. 120). Violent TBI patients had scarring in the front portion of their brains, and Dinn et al. (2009) found that this type of damage made individuals receive higher scores on aggression tests than those individuals with no scarring (p. 121). The Aspen Neurobehavioral Conference consensus was that violence can result from brain problems, and research has discovered a high incidence of head injury histories in the criminal population (Leon-Carrion & Ramos, 2002, p. 210). It has also been reported that due to injury to the frontal lobe, violent behavior has resulted from the behavioral deficits, and people with frontal lesions showed violent and aggressive behavior more frequently than people that suffered injuries to other parts of their brain (Leon-Carrion & Ramos, 2002, p. 210). Frequent violent and aggressive behavior was also noted in patients with mediofrontal brain injury (LeonCarrion & Ramos, 2002, p. 211). According to Luiselli, Arons, Marchese, Potoczny-Gray, and Rossi (2000), juveniles suffering from a TBI may also be prone to criminal behavior due to having deteriorated control of their impulses, reasoning and examination skills, and comprehension skills, which are all consequences of extreme brain trauma (p. 648). These authors developed their claims from a survey that was given to juveniles critically affected by TBI and participating in an educational program within the community that focused on the restoration of brain function (p. 648). The differences in TBI amongst the juvenile delinquent youth were contrasted with youth who were affected with TBI but did 38 not exhibit criminal behavior (Luiselli et al., 2000, p. 648). Over the course of three years, 69 juveniles participated in the survey, and the majority lived in group homes in the community, while the others resided at home with their families (Luiselli et al., 2000, p. 648). The crimes the juveniles committed post-injury were alcohol and drug abuse, arson, sexual offenses, cruelty to animals, theft, and vehicular homicide (Luiselli et al., 2000, p. 649). About one third (9% female and 90% male) of the juveniles participating in this survey committed one or more criminal acts (Luiselli et al., 2000, p. 651). In those that did not commit criminal offenses, 25.5% were girls and 74.4% were boys (Luiselli et al., 2000, p. 651). The post-injury criminal offenses occurred between the ages of 13 and 18, and there were no significant differences between the offending and non-offending groups with regards to type of TBI sustained (Luiselli et al., 2000, p. 651). Luiselli et al. (2000) found that criminal behavior is common amongst juveniles that have suffered a TBI (p. 652). However, these findings definitely indicate that more research is needed on why some juveniles with TBI commit crimes and others do not. One interesting outcome of this survey was that the offending juveniles continued to offend even though they were participating in the community-based program and receiving assistance, which indicated that some may have needed a more secure environment where the impact of treatment could have been more beneficial (Luiselli et al., 2000, p. 654). Conclusion: Knowledge, Assessment, and Treatment All of the information discussed in this review of literature can be used to understand TBI amongst adults and juveniles. As previously stated, research on TBI amongst juveniles is extremely limited, even though children are at great risk of head 39 injury due to the many activities in which they participate. C.T.E. is definitely a disease that can affect juveniles that have played football or other contact sports since they were a small children. Youth that are suffering from severe TBI can definitely suffer from PTSD and the same symptoms as the adults discussed above. Therefore, the information and treatments discussed above can aid medical professionals, as well as probation officers assigned to detention centers, in helping youth understand and manage the symptoms of their TBI. For those youth that are found to be suffering from TBI, but cannot be released from custody pending court due to the severity of their crimes, such as murder, acupuncture and deception could very well be used, with parent permission, to treat and protect the youth, as well as gain their compliance. There are an increasing amount of juvenile offenders entering the criminal justice system with mental health concerns, possibly related to an unknown previous head trauma. Unfortunately, there is a lack of knowledge about the effects of head injury, brain damage, and specifically, damage to the frontal lobe, as it relates to criminal behavior. Due to this fact, professionals in the system do not fully know how to treat this population of juveniles suffering from head injury, and they eventually become persistent adult offenders. It is extremely difficult to combat crime, but it is impossible when all contributing factors are unknown. As discussed in this chapter, TBI can cause so many cognitive impairments that can lead to aggressive and/or violent behavior, and it is imperative that the system helps these individuals discover the serious nature of their injury, understand their injury, and begin the process of rehabilitation. These offenders may, and most 40 likely have, slipped through the cracks of the justice system as incorrigible or resistant to change, but their behavior may not necessarily be intentional. Fortunately, our criminal justice system is moving toward a more evidence based practice model, and there is a growing desire to uncover any criminogenic needs that may contribute to negative behavior. Summary In Chapter Two, this researcher discussed some of the neurological consequences of TBI, the different areas of society where an individual can acquire a TBI (sports and military), some of the ways to treat individuals with TBI, and the behavioral changes that can occur after injury. The research in this chapter indicated there is a problem with TBI, especially with youth, and there is evidence to warrant a closer look at why some individuals behave criminally and violently. The research also indicated there are some evidence-based ways to treat TBI. The ART program is one such evidence-based program that would succeed in being the catalyst in the effort to educate the world on the significant effects of head injury and frontal lobe damage. Research shows that some of the individuals that commit violent criminal offenses may also have frontal lobe damage. Determining who may be suffering from frontal lobe damage and treating them prior to the onset of suicidal, violent, and criminal behavior, is the focus of the treatment discussed in this section. 41 Chapter 3 Project Overview Introduction This researcher is employed as a Deputy Probation Officer and has been for 17 years, while assigned to juvenile institutions, community-based programs, juvenile court, juvenile and adult field units, as well as adult intake. In these assignments, this researcher supervised juveniles housed in detention facilities, investigated and prepared court reports, presented cases before the Judge in the courtroom, and supervised and monitored juveniles and adults after adjudication and sentencing. These assignments have afforded this researcher the opportunity to be trained to verbally and physically supervise individuals involved in the criminal justice system, to investigate crimes and violations of probation, and to write reports to the Court. The following information is based on said experience and training. The first criminal justice agency to receive juvenile offenders from law enforcement officials and guide them through the delinquency process after arrest is the Probation Department. The Probation Department assesses the juvenile for detention or release, investigates the crime, investigates the juvenile’s conduct in the home, community, and school, and prepares a report and dispositional recommendation to the Court. The information that is gathered will be used and considered throughout the delinquency process and beyond by other criminal justice agencies; therefore, it is imperative that this information is as complete, thorough, and accurate as possible. The disposition in the case and the juvenile offender’s life could be forever altered by the 42 decisions made during the delinquency process, so every effort should be made to discover reasons why a juvenile has entered the criminal justice system and what criminogenic needs should be addressed. It is extremely difficult to determine if a juvenile needs to be in custody or just needs therapy if specific information about their home life, social life, and health is unknown due to having no knowledge of the importance of certain questions. Head trauma and TBI have received a great deal of attention lately due to sports-related news and research. However, these types of injuries have been occurring, especially with youth in sports and motor vehicle accidents, for years, as stated in Chapter Two of this project. Chapter Two discussed and showed that TBI can have a lasting effect on the injured, as well as their family and friends. Cognitive functions that were once controlled may no longer be, such as the ability to control one’s impulses and to appropriately respond to social situations. Multiple TBI’s can also impact an individual and cause severe damage. A juvenile that is being processed into a detention facility may have suffered such injury and may not be able to successfully be housed on a general population living unit. Also, a juvenile that may have a history of concussion, may not be able to sustain another blow to the head. Understanding these issues could mean a probation department escapes lawsuit and a juvenile escapes being labeled as a persistent offender. Purpose and Intent The purpose of this research is to explore the consequences and treatment of TBI and to evaluate whether three different assessment tools that are being utilized by local 43 probation departments within the United States assess for TBI. This researcher will also develop an assessment tool and protocol that can be used by said departments in determining who may be suffering from TBI, whether they need a clinical evaluation, and what the treatment goals will be in their case plan. It is the intent of this researcher to inform local probation departments about the issues, concerns, deficits, and treatment needs surrounding TBI, so that they will understand the importance of knowing whether the juveniles in their care and custody have suffered such injury. This researcher will be reviewing and analyzing currently used assessment tools for any assessment questions that relate to TBI. Risk Assessments Risk assessments were created to help guide practitioners, such as probation officers, in making decisions regarding the custody, disposition, and treatment of the juveniles that enter the criminal justice system based on the likelihood the juvenile will not appear in court, will misbehave in custody, or will recidivate (Brumbaugh, HardisonWalters, & Winterfield, 2010, p. 6). These assessments vary across the United States and are based on different principles, as they are created to fit the needs of each agency and jurisdiction. This researcher will discuss and review three widely used risk assessments to determine if they allow for the assessment of juveniles for head injury or TBI. These three risk assessments are the Detention Risk Assessment Instrument, the Youth Assessment and Screening Instrument, and the Positive Achievement Change Tool, which are all used by probation departments throughout the United States. All of the assessments chosen for review are used differently, and that is why they were selected. 44 The Detention Risk Assessment Instrument is solely based on determining the juveniles risk to re-offend prior to appearing in court (Brumbaugh et. al., 2010, p. 3). The Youth Assessment and Screening Instrument is risk-based, but mostly strength-based, as it analyzes positive and negative behaviors and protective factors to decide which treatment services would be most successful (Brumbaugh et. al., 2010, p. 8). The Positive Achievement Change Tool is treatment-focused, and is used in determining case disposition, which considers whether the juvenile would benefit from probation, what form of probation, and what treatment options are appropriate (Brumbaugh et. al., 2010, p. 3). Detention Risk Assessment Instrument In 1993, a juvenile detention reform began, and the Juvenile Detention Alternatives Initiative (JDAI) was introduced by the Annie E. Casey Foundation, which allowed for grants to be given to states and other agencies that chose to participate in the reform (Steinhart, 2006, p. 5). The mission of the JDAI was to decrease the number of children held in detention facilities that did not need a secured environment, limit the amount of children detained and enhance the conditions of the facilities, inspire the growth of options to secure detention, and dissuade the juveniles from not appearing in court and committing new offenses (Steinhart, 2006, p. 5). The probation department in Sacramento was one such agency awarded a grant under JDAI at the beginning of the reform, and as a result, had to forego using certain security equipment inside the detention facility, such as pepper spray. Risk screening, assessing whether secure detention is necessary, at the detention intake level is the basic and most important way 45 of executing the JDAI mission (Steinhart, 2006, p. 5). Some jurisdictions in the United States allow law enforcement officials to implement the risk screening in the field or call in to the detention facility to complete the screening over the phone (Steinhart, 2006, p. 5). The detention risk assessment instrument (RAI) is the fundamental tool of risk screening, and is a listing of written rules that govern how each juvenile entering the detention facility will be rated (Steinhart, 2006, p. 5). The final risk score will be used by the intake officer to determine if a juvenile should remain in secure detention, be released home pending court, or be placed on a program of non-secure detention pending court, such as home supervision or electronic monitoring (Steinhart, 2006, p. 5). All RAIs are based on points under JDAI, but each jurisdiction within the United States systematically develops their own RAI to best satisfy the needs of their agency (Steinhart, 2006, p. 5). The RAIs under JDAI have achieved their goals, in that decisions to detain or release juveniles at the detention intake level have been standardized, overcrowding in the detention facilities has been reduced, and agencies participating in JDAI have lowered their culpability and expenses (Steinhart, 2006, p. 5). Prior to the JDAI, the detention facility environments in many jurisdictions were acceptable, and some were unfathomable, which resulted in the maltreatment and impairment of many detained juveniles, not to mention the loss of these juveniles due to the taking of their own lives (Steinhart, 2006, p. 7). Conditions in many facilities were a definite issue at the beginning of the reform, but a more important issue, was the overcrowding in most of the facilities run by government agencies (Steinhart, 2006, p. 7). 46 RAI’s were developed to control the amount of juveniles detained in these facilities using rules that were more concentrated than the laws of detention set forth by state, city, and county laws (Steinhart, 2006, p. 7). These more focused rules would guide the intake staff in determining which youth did not pose a threat to themselves or the community and which youth did pose such threats (Steinhart, 2006, p. 7). Liability issues arise when low-risk youth are placed in secure-detention and are subjected to the abuses of more criminally sophisticated youth. There were three basic fundamentals that guided the formulation of the RAIs, and they were objectivity, uniformity, and concentration on risk (Steinhart, 2006, p. 7). The decision to detain or release a juvenile should be based on the alleged offense and the juvenile’s prior criminal history, not on the intake officer’s opinion, and the screening questions should be uniform and consistent so that they are used fairly for each juvenile being screened (Steinhart, 2006, p. 7). The screening questions being used should only be based on the risk of the juvenile to re-offend or not appear in court as ordered, and not on the subjectivity of the intake officer (Steinhart, 2006, p. 7). Officers can occasionally base their detention decisions on the attitude of the juvenile or the way the juvenile dresses or carries himself, which is often times dictated by the officers training and experience, but these reasons are not concrete, not based on risk, and cannot be equally utilized. Many states, such as Florida, New Mexico, and Virginia, began to see the accomplishments of the JDAI and changed their juvenile laws to order the detention risk screening to be administered at the intake level (Steinhart, 2006, p. 8). 47 While the RAI under the JDAI measures the risk to the safety of the community and the risk of the minor appearing in court for his detention hearing, it absolutely does not measure the risk the juvenile poses to himself (Steinhart, 2006, p. 10). Historically, the danger the juvenile posed to himself was often used as a reason to securely detain a juvenile, but this reason was heavily used and abused (Steinhart, 2006, p. 10). The law enforcement official or intake officer had the discretion of detaining the juvenile for whatever reason and using the idea that he was a danger to himself, such as the juvenile was out of control in the home, and the parent needed space, or the juvenile was uncooperative with officials (Steinhart, 2006, p. 10). The officer could feel the juvenile had a mental issue or was intoxicated due to his behavior, so the juvenile was detained pending court. However, these personal and/or medical reasons cannot sufficiently be measured in a detention risk screening instrument, and housing a beyond low-risk juvenile in a secured facility to punish him can make the probation department liable for any harm the juvenile suffers (Steinhart, 2006, p. 10). RAIs are based on time, as they were developed to advise intake officers on the decision to hold a juvenile in custody or not from the time of receiving the juvenile from law enforcement until they appear in court for a detention hearing and subsequent dispositional hearing (Steinhart, 2006, p. 10). After the case is adjudicated and a disposition rendered, the RAI is no longer in effect, as the Court determines whether the juvenile will remain in custody, be released, or participate in an alternative detention program (Steinhart, 2006, p. 12). The RAI only covers this time period due to the fact that this is when the greatest concern is placed on whether the juvenile will appear in 48 court to answer to the crimes alleged, and the intake officer is the person responsible for ensuring he will appear based on his accepting custody of the juvenile from law enforcement and his custody decision. Once the case is disposed of, the Court will take on the responsibility of making a custody decision. As previously stated, the jurisdictions that were awarded grants through the JDAI use risk screening instruments that are point-based, and each question on the instrument is attributed a certain number of points (Steinhart, 2006, p. 9). The total risk screening score is placed onto a point scale that will reveal a decision on whether the juvenile should be detained, released, or given an alternative to detention (Steinhart, 2006, p. 9). If a juvenile has a score that is over a certain level, he is deemed high-risk and will be eligible for secured detention (Steinhart, 2006, p. 9). Conversely, if a juvenile’s score is lower than the designated level, he is determined to be low-risk and must be released; however, the scores can be overridden by a supervisor (Steinhart, 2006, p. 9). There are many jurisdictions that have a middle level of scores, and if a juvenile scores in that range, he is released to a form of alternative detention that is not secure, such as electronic monitoring (Steinhart, 2006, p. 9). The point-based model was not always the only approach for a detention risk screening instrument, as there were instruments that did not use points or calculate risk scores (Steinhart, 2006, p. 9). Instruments that did not use points used matrix scales with questions that only required yes or no answers, and if there were one or more yes answers, the juvenile would be suitable for secure detention (Steinhart, 2006, p. 9). Questions that could appear on these assessment tools were: Is the alleged offense a 49 felony? Is the juvenile currently on probation? Does the juvenile have a history of abscond behavior from custody (Steinhart, 2006, p. 9)? However, within the JDAI, these non-point instruments were discarded as validation studies stated that point-scale detention screening instruments were more adjustable, precise, practical, and more in line with the goals of the JDAI (Steinhart, 2006, p. 9). Essentially, the RAI is a tool that brings reliability, organization, and consistency to the detention decision making process, which does not totally discount the discretion of the intake officer to override the tool if the alleged crime or behavior of the juvenile warrants such action (Steinhart, 2006, p. 9). The Detention Risk Assessment Instrument (DRAI) is a fair and impartial riskbased tool that is based on the JDAI, and provides information to intake officers regarding detention and release recommendations (Sacramento County Probation Manual [SCPM], 2012). The DRAI is also a point-based tool, as designed by the JDAI. The DRAI is used across the country by many different jurisdictions, though tailored for their purposes, as previously stated. The following DRAI is what is used in many jurisdictions in California, and it is completed on all juveniles pending charges and admitted to the detention facility, with the exceptions noted in the DRAI instructions under “Automatic Hold”, which are: - Present offense Criminal history Legal status – Probation or Parole Warrant history History of escape from secured custody Most serious pending charge Prior commitments Aggravating factors Mitigating factors 50 The juvenile will automatically be held in custody if he was arrested due to a warrant for his arrest, as only “no bail” warrants are issued for juveniles. Juveniles are not eligible for bail, unless being tried as adults. A person with a “no bail” warrant has to remain in custody until he appears before the Judge. In this instance, a detention decision is not necessary. The juvenile could also be held in custody automatically due to the severity of the arresting offense, such as murder. The intake officer adds points to any of the sections above where there is history (SCPM, 2012). Points will be added due to the severity of the present offense, whether the juvenile has a prior criminal history, is on active probation, has had previous warrants for his arrest, and/or has previously escaped from custody (SCPM, 2012). Under mitigating factors, intake officers would ask about good community ties, and the juvenile would have good community ties if they had three or more of the following: -Stable Living Address -Educational Stability -Supportive Family -Active Connection to Adult(s) -Participating in Treatment and/or Counseling -Active in a Religious Organization -Participation in Organized Sports within last 12 months -Volunteers -Active in Pro-social Clubs, Sports, Organizations, Community, or Cultural Groups The intake officer will add points if the juvenile does not have a stable home environment, not attending school regularly, no family ties, and does not participate in any of the pro-social activities listed above (SCPM, 2012). The total number of points will dictate to the officer whether the juvenile should be securely detained, released to his parents, or placed on a program of alternative detention outside of the facility pending 51 court (SCPM, 2012). There is an override option that states the intake officer does not have to accept custody of the juvenile after arrest until the juvenile is medically cleared, which is for the safety and security of the juvenile (SCPM, 2012). The DRAI further dictates that the intake officer would also advise the parent(s) that the officer will interview the juvenile, after the Miranda admonishment (SCPM, 2012). The information gathered will be used in the intake report that is submitted to the Court at the Detention Hearing (SCPM, 2012). This report encompasses family background information and school history that is provided by the parent(s). The only time a probation officer in Sacramento County, California, can speak to the juvenile prior to an attorney being assigned is at the intake level. Therefore, obtaining a statement and/or information from the juvenile at this time is paramount. The statement should only be about the current situation, family life and behavior, and the alleged offense (SCPM, 2012). The intake officer should ask the juvenile about his living situation, which includes who resides in the home, sibling information if any, behavior of the juvenile in the home, whether he follows the parents’ rules, and any history of running away from home (SCPM, 2012). The intake officer should also ask the parent(s) about the physical and mental health of the juvenile, which includes any drug and alcohol abuse, gang membership or affiliation, whether they suffer from any medical or mental health conditions, are taking any prescribed medication, participating in counseling, and whether the juvenile has ever been the victim of any sexual, physical, or emotional abuse (SCPM, 2012). 52 The intake officer should also ask about school progress, any school discipline, whether the juvenile is or has been a special education student, and whether the juvenile has an Individualized Education Plan (IEP) at the school (SCPM, 2012). The intake officer should also ask if the juvenile participates in any extra-curricular activities such as sports, and if there is anything the parent(s) want the Court to know (SCPM, 2012). Finally, the intake report should also list available resources to assist the juvenile (SCPM, 2012). Analysis of DRAI The DRAI standardizes the process of detaining youth in juvenile detention facilities and limits the amount of youth detained. In this researcher’s experience as a Deputy Probation Officer, juvenile detention facilities have been overcrowded across the country for many years, which often adds to chaos in the facilities. The DRAI was designed to address standardization and overcrowding. The probation department in which this researcher is employed is one agency that uses and has benefitted from the DRAI. Youth are detained based on the points acquired during the DRAI and not any other reason. The juvenile’s attitude and risk of harm to him- or herself are not used as reasons to detain since they are not criteria used in the DRAI. Juveniles that score low on the DRAI, are not detained, unless the score is overridden, and alternatives to detention are used, such as electronic monitoring. Thus, overcrowding in the detention center has been eliminated. The DRAI collects information from the juvenile or parent that can be used by other probation officers, law enforcement, and the court. The DRAI collects information 53 about the juvenile’s criminal history, family life, education, community ties, and extracurricular activities, which gives the probation officer some insight to whether the juvenile needs to be detained or released. This information is very important at the intake level, as the officers need to know if the juvenile will ultimately appear in court for his or her detention hearing and any subsequent hearings. However, this information can aid staff inside the detention center in understanding the juvenile’s behavior and his or her classification. This information can also be used by the juvenile court probation officer in preparation of the court report to be submitted to the judge. It is vital to know whether the juvenile has a stable home life, participates in activities outside of the home, and has access to any community resources. If there are problems in the home, releasing the juvenile to his or her parents while awaiting the detention hearing may not be in his or her best interest. Also, if the juvenile is participating in activities in the community, s/he may be that much more eager to appear for court, so as to not be detained and unable to further participate. Unfortunately, the DRAI cannot be used as the only form of assessment for a probation department. The DRAI does not calculate risk to re-offend, assess for criminogenic needs, and does not suggest treatment options, as do other assessment tools. The DRAI was developed to only address the issue of detention after arrest and pending court, which subsequently solves issues of overcrowding and unfair practices of detaining youth based on subjective reasoning. Another tool would be needed to aid probation officers and the court in determining what problems need to be addressed with the 54 juvenile and his or her family, upon adjudication, that might be contributing to the juvenile’s criminal behavior. One of the contributing factors could be head trauma; however, the DRAI does not assess for head trauma or injury. There are many areas of the DRAI that can be expanded to obtain possible information about a history of concussion, head injury, and/or TBI, such as when asking about sports participation, medical and mental health, behavior in the home, prescribed medication, and whether the juvenile participates in any treatment or counseling. The questions about education could also be expanded to include questions about head trauma, more specifically for those juveniles that have special education needs and an active Individualized Education Plan (IEP). However, the DRAI does not guide the intake officers or alert them to specifically ask about head injury, concussion, or TBI. Youth Assessment and Screening Instrument The Youth Assessment and Screening Instrument (YASI), as developed and marketed by Orbis Parthers Incorporated, is a program that not only determines risk, but also determines what resources the high-risk juvenile may need and what protective influences he has, so that a case plan may be developed (Orbis Partners Incorporated (OPI), 2013, p. 1). This instrument can be used by any agency that must determine the needs and risks of the juveniles in their care such as probation departments, schools, and child protective services (OPI, 2013, p. 1). In essence, the YASI is a program that allows probation officers to input information regarding juveniles and analyze the information to formulate an appropriate treatment plan (OPI, 2013, p. 1). The partners at Orbis believe 55 that officers should not just simply assess the juveniles in their care, but use that information to develop a case plan that is tailored for that specific juvenile, and this case plan is the most important part of the assessment process (p. 1). The assessment reveals certain characteristics and risks about the juvenile that can predict future criminality (OPI, 2013, p. 1). These characteristics must be addressed to promote positive changes in the juvenile and limit the risk of continued misbehavior or re-offending, and the case plan displays what the characteristics are and how they should be addressed (OPI, 2013, p. 1). This concentration on assessment, case plans, and discovering factors that aid the juvenile were introduced by the Washington State Juvenile Assessment model, which was developed in the latter part of the 1990s (OPI, 2013, p. 1). The YASI was based on the improvements of the Washington model used in New York and Illinois, along with the youth custody application used in California (OPI, 2013, p. 1). The YASI connects the assessment with the case plan using accessible software that can be purchased by agencies and tailored to fit the needs of that agency (OPI, 2013, p. 2). The YASI has four basic elements, which are the initial assessment, finding the motives of the juvenile, identifying formal and informal controls and applying treatment and supervision goals, and following up with the progress of the case plan (OPI, 2013, p. 2). There are 10 basic domains in the YASI program that have become apparent from current research on criminogenic needs, and they are: - Legal History Family Education Community/Peers Substance Abuse 56 - Mental Health Violence Attitudes Skills Use of Free Time/Employment (OPI, 2013, p. 3) The difference between the YASI domains and other assessments is the fact that YASI uses the latest research to re-develop their domains and enhance the case plan programming (OPI, 2013, p. 3). One of the most appealing features of the YASI is offered to probation officers, and it is the idea of measuring and monitoring strengths in the juvenile’s life such as family and community ties, educational goals and attachments, and goals for the future (OPI, 2013, p. 3). The measuring and consideration of these strengths is what sets the YASI apart from other assessments and solidifies the program in the case planning process (OPI, 2013, p. 3). The YASI consists of a pre-screening application, as well as a full assessment. The pre-screening application is mainly used for classifying the juveniles and consists of at least 30 questions that deal with facts in the juvenile’s life, such as criminal behavior and family dynamics, as well as characteristics of the juvenile that can be changed (OPI, 2013, p. 5). The pre-screening application is used to assist probation officers with detention decisions (OPI, 2013, p. 5). The classifications from this screening are low, moderate, and high risk to re-offend, and the pre-screening immediately alerts officers to the moderate and high risk juveniles, so that these juveniles can receive more concentrated assistance (OPI, 2013, p. 5). The moderate and high-risk juvenile will then undergo the full assessment in order to develop an elaborate analysis of his at-risk behavior and characteristics that will be the basis of the case plan (OPI, 2013, p. 5). An 57 interview with the juveniles is essential for the pre-screening; however, most of the factual (static) information about the juvenile, such as criminal history and family background, can also be found in the police report and prior probation reports (OPI, 2013, p. 5). The full assessment adds to the pre-screen by providing a more elaborate evaluation of the dynamic information, criminogenic needs, protective factors, and risk to re-offend, which are all used in the development of the case plan for the higher-risk juveniles (OPI, 2013, p. 6). The full assessment contains questions that focus on the behavior of the juvenile that will lead to directions for treatment in the case plan (OPI, 2013, p. 6). For ease of understanding, the findings of the full assessment are exhibited in a wheel graph, and users only have to click on a part of the wheel that corresponds with a certain risk factor, which reveals gathered information on the juvenile (OPI, 2013, p. 7). The YASI provides another valued service that other assessments do not provide, which is the reporting of all of the information gathered (OPI, 2013, p. 8). All of the information provided by the full assessment and entered into the YASI software can be made into a report that can be used to formulate a court report, or the YASI report can simply be provided to the court itself (OPI, 2013, p. 8). The YASI report can also be provided to other stakeholders and agencies assisting the juveniles, giving them the information needed to render their services (OPI, 2013, p. 8). Finally, the YASI report can also be used gather statistics for the agency as a whole (OPI, 2013, p. 8). The agency would be able to show the population of juveniles being served, identify problems with the services provided, and determine where continued funding would best be utilized 58 (OPI, 2013, p. 8). After all of the information has been provided in the software, the YASI can be used to predict further criminality and service needs by pinpointing what the juvenile’s criminogenic needs are and how they weigh against the strengths in his life (OPI, 2013, p. 8). Analysis of YASI The YASI is a full service tool that forces probation officers to fully assess, classify, and help treat the juveniles they serve. The pre-screen portion of the YASI is used at the detention intake level to determine if a juvenile should be detained, placed on a program of alternative detention, or released to the care and custody of his parents pending court. It is also used to classify the juveniles that are detained in the facility. The full-assessment allows the probation officer to gather more information about the juvenile and his life, which can then be used for a court report or a report to other agencies that will serve the juvenile and his family. This information is also placed in a case plan that guides the field probation officer in understanding what type of treatment needs to be completed by the juvenile and his or her family. The YASI also determines the strengths of the juvenile, which is not addressed in other assessment tools. Strengths include having a good home life, good community ties, and a good education. This is weighed heavily against the criminogenic needs of the juvenile in the YASI and displayed in the case plan. This counts as the risk to re-offend. The YASI then gives a score of low, moderate, and high-risk to re-offend, and only the moderate and high-risk juveniles will be eligible for detention and for the full assessment. Assigning a risk level to the juveniles does not end the assessment process. The YASI 59 software continues to take all of the information and compile it into a report that can be used as part of the court report. Reporting the outcome of the assessment is also an aspect not seen in other assessment tools. The case plan suggests different treatment options for the juvenile and serves as a follow up to the initial full-assessment. Unfortunately, the YASI does not ask about or assess for head injury. As in the DRAI, there are domains in the YASI that can be expanded to assess for head injury. These domains are community/peers, substance abuse, mental health, violence, attitudes, and skills. If the juvenile participates in sports in the community, a history of concussion could be addressed. Also, if the juvenile abuses substances, finding the reason behind it could uncover possible head trauma. Mental health and violence are definitely domains that could encompass questions about head injury, as mental health changes can occur after injury, including violence and aggression. Attitudes and skills can change drastically after TBI, so if a parent indicates the juvenile’s attitude changed, an inquiry into why the change happened could uncover possible head injury. Positive Achievement Change Tool The Positive Achievement Change Tool (PACT) is a complete assessment that consists of 126 questions that are asked of the juvenile in an intake interview prior to the juvenile appearing in court, and the answers to these questions will determine a risk score that is used to measure the probability of the juvenile re-offending (Barnoski, 2013, p. 1). The PACT is evidence-based and validated, and is a case management assessment program that was developed by the Department of Juvenile Justice in Florida and Assessments.com in 2005 (Barnoski, 2013, p. 1; Olson, 2007, p. 2). The PACT was 60 essentially based off of the Washington State Juvenile Court Assessment, which is what birthed the YASI (Barnoski, 2013, p. 1; Olson, 2007, p. 2). The PACT was created to provide a more precise way of accumulating crucial information to measure a juvenile’s risks and criminogenic needs (Olson, 2007, p. 2). The PACT, much like the YASI, reveals the strengths of the juvenile and what treatment services would work with those strengths to improve the juvenile’s behavior (Barnoski, 2013, p. 1). There are 12 areas of concentration in the PACT that have been proven to be indicators of future criminality: - Criminal History Education Free Time Activity Employment Current Relationships Family Ties Living Arrangements Alcohol/Drugs Mental Health Attitudes and Behaviors Violence Skills (Barnoski, 2013, p. 1; Olson, 2007, p. 3) The PACT is approximately a 45-minute interview, and the practitioners executing the PACT are required to undergo training in motivational interviewing, a key factor in the PACT, to get the most accurate and useful information from the juvenile (Barnoski, 2013, p. 1; Olson, 2007, p. 2). The PACT encourages and measures positive change, and this all begins with the interview. The intake officer must begin motivating the juvenile to desire to make positive changes; therefore, the interview must be more than the exchange of questions and answers, it has to be insightful, uplifting, and rehabilitative. The PACT software also has the capability of producing a case plan for the practitioner, 61 as all of the information put into the program indicates the needs of the juvenile, and is distributed throughout the case plan (Barnoski, 2013, p. 1). Other types of assessments before the PACT, especially in Florida, assessed juveniles based on the alleged offense and their prior record, but the PACT considers family strengths and dynamics, pro-social activities and skills, educational level, and other mitigating factors before deciding the risk level of a juvenile and disposing of the case (Olson, 2007, p. 3). The PACT is an evidence-based tool, and it has gained vast approval due to the fact that focusing treatment on the particular needs of the juvenile has been validated as a means to reduce recidivism, as opposed to just giving a punishment for the crime committed and continued criminal behavior (Olson, 2007, p. 4). The risk levels used in the PACT are based on the probability of the juvenile re-offending, and the levels are: - Low Moderate Moderate-High High (Olson, 2007, p. 4) The questions asked in the PACT create scores displayed as percentages for each area measured, and this percentage is used to determine the risk level of the juvenile (Olson, 2007, p. 2). The PACT aims to fit the recommended treatment and disposition of a case to the risk-level of the juvenile (Olson, 2007, p. 3). If a juvenile is a low-risk to reoffend, he may receive few sanctions or none at all, as he is less likely to commit another offense (“How to Read,” 2006, p. 2). However, a juvenile that is a high-risk to re-offend may very well need more sanctions and interventions, as the likelihood of this juvenile continuing his criminal behavior is high (“How to Read, “ 2006, p. 2). 62 The name of the PACT alone signifies positive change and rehabilitation, and it has two purposes (Olson, 2007, p. 3). The first purpose for naming the PACT was to stress to juveniles the importance of making a positive change in their lives and instilling in them the desire to accomplish something positive (Olson, 2007, p. 3). The second purpose surrounds the acronym, PACT, and it encourages a lawful agreement between everyone in the juvenile justice system, the court, probation officer, juvenile, parent, and service provider, to work together to aid the juvenile in making positive choices and decisions in his life (Olson, 2007, p. 3). The PACT itself was created to achieve four goals, and they are: identify the juvenile’s risk-level to re-offend to ensure services are provided to juveniles that risk higher, determine the risks and strengths of the juvenile to be certain treatment services are focused on the juvenile’s needs, concentrate on decreasing issues that cause risk and increasing the juvenile’s strengths, and aid practitioners in following up with the progress of the court’s treatment plan for the juvenile (“How to Read,” 2006, p. 1). Analysis of PACT The Sacramento County Probation Department uses the PACT when writing juvenile court reports and recommending dispositions in the cases. The PACT is only used for disposition and not for detention decisions at the time of arrest. The PACT is completed at the intake level; however, there are occasions where the PACT is not completed, and the juvenile court report writer, who is also a probation officer, completes the PACT by interviewing the juvenile’s parents, as the juvenile court report writer is not allowed to speak with the juvenile without the permission of his attorney. If a juvenile is 63 not detained at the time of arrest, but is cited, and he fails to appear for the citation hearing, the juvenile court report writer will complete the PACT before the court report is submitted for review. The court wants to know what the PACT risk level is to help determine if the juvenile should be committed to secure detention, committed to a placement facility, placed on home supervision, and/or referred to counseling after being adjudicated. In Sacramento County, low- and moderate-risk juveniles are not recommended for commitment to the detention center or a placement facility post-adjudication, unless the decision is overridden by a supervisor due to the nature of the offense or the juvenile not having a parent or guardian available. The PACT lets the juvenile court report writer know what, if any, type of counseling the juvenile and his family may need. If the juvenile receives a certain score in family and relationships, functional family therapy will be recommended. All of the information received and recorded in the PACT is autopopulated into a case plan, and the counseling and treatment plans are already chosen based on the PACT percentage scores and determined risk-levels. The PACT deals mostly with the juvenile’s risk to re-offend and the positive changes the juvenile needs to make after adjudication. It is not used at the intake level for detention decisions. Although the PACT interview is administered at the intake level, the information is forwarded to the officer that prepares the court report to help them determine a dispositional recommendation to the court. This is the difference between the PACT and the previous two assessments discussed. The DRAI is only used for 64 detention decisions, and the PACT is only used for post-adjudication. The YASI is the only assessment that encompasses both aspects. The PACT does not assess for, or even ask about, head injury. It is quite interesting that the PACT is developed to positively affect change in the juvenile, but it does not ask about something so important. TBI after head injury can dramatically change a juvenile’s life, and to not consider the possibility of this contributing factor is counter-productive. Every effort should be made to uncover the reasons why the crime has been committed. The PACT considers the juvenile’s strengths and issues, but does not ask about something so important. There are sections of the PACT that can also be expanded to address possible head injury, and they are: current relationships, family ties, living arrangements, alcohol/drugs, mental health, attitudes and behaviors, and violence. Summary All of the assessments reviewed in this chapter are unique, in that they measure some of the same characteristics and risks, but are used quite differently. The DRAI is strictly used to aid probation officers in determining if a juvenile should be securely detained or not upon entering the detention center after arrest. The YASI is also used to aid probation officers in making detention decisions, but it takes the risk assessment a step further with the full assessment. The YASI also provides information to guide the probation officer and the court in the final disposition of the case. The YASI identifies and measures qualities, characteristics, and risks of each juvenile to make a prediction on whether a juvenile will continue to re-offend and what services are available to assist that juvenile. The YASI is a full service assessment. The PACT is an assessment much like 65 the YASI, but it is not used to make initial detention decisions. The PACT identifies and measures risks and strengths of juveniles to determine which services would best help the juvenile to reduce his risks and increase his strengths. The PACT is used to aid the court in determining dispositions and sanctions. Appendix A is a key that explains the codes and information in Appendix B. Appendix B illustrates what basic topics these assessments address and do not consider. Appendix B considered questions about health, sports, injuries, hospitalizations, abuse, and head injury/TBI. It is evident that none of the above assessment instruments mandate that an intake officer ask or assess for head or brain injury when receiving juveniles for possible detention in their juvenile hall facilities. Unfortunately, the probation department in which this researcher is employed does not specifically ask or know about the offenders that have suffered a TBI, and offenders do not know the significance of their injuries to alert their probation officers and/or therapists. This researcher has never been trained to specifically ask or assess for TBI. The assessments guide the intake officers in asking the juveniles basic questions about their health, but do not appear to make it clear if they are asking about injuries outside of arrest at all, not to mention whether they were recent and major or not. As the research shows in Chapter Two, some individuals suffering from severe TBI may not even believe they have an injury, problem, or disability. Therefore, simply asking the juvenile or their parent a general question about their health or any injuries may not be thorough enough to get the most accurate information and picture of what is happening with the juvenile. Juveniles and parents could also believe that the 66 concussion(s) the juvenile sustained a year ago while playing sports is not worthy of discussing now because the juvenile is no longer under a doctor’s care. They may not know that the reason the juvenile steals and excessively curses may be indicative of damage to his brain due to the concussion or head injury. It is also clear that informing and training intake officers about the symptoms and significant impact of TBI can help them be the information agents for the juveniles, parents, and the Court. The intake officers need to be aware of the specific questions and wording they need to use and look for in order to inquire about head or brain injury. 67 Chapter 4 Assessment Tool and Protocol Researcher’s Proposal The purpose of this assessment tool and protocol, Assessment of Head Injury Tool (AHIT), is to guide probation departments and their juvenile intake officers in asking the questions necessary to thoroughly and accurately assess juveniles for entry into the Juvenile Detention Facility, as well as the criminal justice arena. The previous chapters in this project discussed how youth are more prone to head injury due to the many activities in which they are involved, how TBI can affect cognitive functioning and behavior, some of the available treatments, and how the assessments used by juvenile intake staff do not assess for TBI. An accurate assessment and classification of the juveniles entering detention facilities should decrease harm to the juvenile, other juveniles in the housing units, staff supervising the housing units, and the liability on the Department as a whole. AHIT should also increase the safety and security of detained minors, staff, and the institution as a whole. As the first contact in the criminal justice arena after arrest, it should be the responsibility of the Probation Officer in the Juvenile Hall Intake Unit to use AHIT, accompanied by their existing intake questionnaire, to assess the juvenile for possible head injury or traumatic brain injury (TBI), past or present, and classify the juveniles accordingly. AHIT, shown on page 69, along with the existing intake questionnaire, should be administered to every juvenile entering the Juvenile Detention Facility for detention and 68 every juvenile entering the intake process through law enforcement citation. The most accurate information is necessary to make the best dispositional recommendations to the court and the appropriate referrals for treatment. 69 Assessment of Head Injury Tool (AHIT) 1. Have you ever had an injury to your head in any of the following situations? (Check all that apply): O O O O O O O Motor Vehicle Accident Sporting Event Fall Gang confrontation, incident, or event Shooting Other specify: _______________________________ None (Do Not Continue AHIT Tool) 2. When did the injury occur? __________________________________________________________________ 3. Did you have any of the following symptoms immediately occur after the injury? (Check all that apply): O O O O O Confused or Disoriented Memory Loss Loss of Consciousness/Pass Out for less than 20 minutes Loss of Consciousness/Pass Out for more than 20 minutes Other ___________________________________________________ 4. Were you hospitalized? O Yes O No 5. If yes, what happened and how long were you there? _______________________ __________________________________________________________________ 6. During the next few days, did you experience any of the following: (Check all that apply): O O O O O O O Memory Loss Headaches Problems with balance Insomnia Irritability Confusion Other ____________________________________________________ 70 7. Did any of the above symptoms continue and/or get worse? __________________ __________________________________________________________________ 8. Do you still have any symptoms today? __________________________________ ___________________________________________________________________ 9. Do you take any medication? If yes, what kind? ___________________________ ___________________________________________________________________ 10. Do you participate in treatment or therapy for this injury? What kind? __________ ___________________________________________________________________ 11. Is there anything you want to add about your injury or injuries? ___________________________________________________________________ ___________________________________________________________________ ___________________________________________________________________ ___________________________________________________________________ ___________________________________________________________________ ___________________________________________________________________ 71 Protocol If the minor states he has had a previous head injury with multiple symptoms, but the symptoms are no longer present, he may have suffered a mTBI, but this will not be a diagnosis. The minor may no longer be suffering from any symptoms, but the information should be logged in the intake report for review by the Court. If the minor suffered an injury, was unconscious more than 20 minutes, was hospitalized, prescribed medication, and suffered ongoing symptoms for six months after injury, he had a TBI. If the symptoms are still present, especially dizziness, headaches, irritability, comments that do not make sense, and medication, the minor needs to undergo a clinical interview for possible severe TBI and possibly a medical clearance to be admitted into the juvenile hall. An override can occur if the crime committed is a major index crime, and if the safety and security of the minor, victim, and community are at risk. The Supervising Probation Officer, or his designee, shall have the responsibility of the override. The goal of AHIT is to gain as much insight into the life of the minor being admitted for detention as possible. The safety of the juvenile and everyone else in the facility is of great concern. If the individual has suffered one or more head injuries, it is imperative that he not experience another. Detention facilities can have emergency situations, such as fights and assaults, that would exacerbate the minor’s previous or current symptoms. If a minor suffered a severe head injury, his behavior may be more than juvenile hall staff can handle. He may consistently defy authority and become aggressive with staff and other youth in the facility. This may cause an issue of restraint and possible injury to the juvenile or staff, and force a liability issue. It is imperative that 72 probation departments uncover the real reason a person’s behavior is beyond control so staff can make the best placement option that will suit the needs of the juvenile, staff, and community. The current research on TBI is clear. Injury to the head can cause mild to profound damage to the brain, and the frontal lobe is most commonly damaged (Miura et al., 2005, p. 662). Juveniles are at such great risk because of the amount of physical activity they participate in such as sports, playful activity, and gang membership (Miller, 1999, p.158; Miura et al., 2005, p. 662; Sonnenberg et al., 2010, p. 1003). This brain damage causes people to lose consciousness, memory, and cognitive abilities, and an injured person can also sustain permanent balance and physical impairments that alter his life (Miller, 1999, p. 157). This individual could behave totally different from the way he behaved prior to the injury. The worst part about TBI is that the injured person cannot and does not understand the damage that has occurred to his brain, so the willingness to participate in counseling, treatment, or therapy is not present (Matthes & Caples, 2013, p. 129). This person may consistently defy authority due to his quick temper, inability to control his impulses, and his inability to know how to behave in social situations, not to mention detention facilities. This behavior may not be signs of a persistent criminal offender. This behavior could be due to damage to the brain as a result of a sustained head injury. Therefore, it is extremely important that agencies complete the AHIT assessment and comply with the stated AHIT protocol to limit further injury and liability. If it is discovered that a juvenile may have suffered or is currently suffering from a possible head injury, a medical screen in the form of a clinical interview needs to be 73 completed. The individual will need to be medically cleared before admittance to the detention facility. If the individual cannot be cleared, the Supervising Probation Officer, or his designee, will have to do an override and determine if the alleged crime demands the individual be detained. If the crime does not demand detention, the Supervising Probation Officer shall determine whether the juvenile will be held at the detention facility or released to the care and custody of his parent(s) with a recommendation to seek immediate medical attention. This information should be immediately shared with the minor’s attorney, the District Attorney, and the Court. If the individual can be housed in the detention facility with past or present head injury or TBI, he should be housed in the clinic, if possible, and observed. If the individual is cleared by the clinic to be housed elsewhere in the facility, the first choice should be isolation and not general population so that the individual does not sustain further head trauma or cause harm or disruption for other juveniles or staff. The mental health team in the facility should be immediately notified of the situation, and treatment should begin while in detention, as research indicates treatment and rehabilitation early on in recovery after a head injury can limit the symptoms and consequences of the TBI. The attorneys and the Court should be made aware of the injury so consideration can be given to the mitigating factors associated with the commission of the crime. After disposition and adjudication, if the minor is placed on probation, the information about the TBI shall be shared with the Probation Officer supervising the minor. A case plan and treatment goals should be formulated to assist the minor 74 regarding the crime, but most importantly his TBI. Every effort should be made to assist brain-injured juveniles in the completion of their case plan and treatment goals before said juvenile can be returned to Court for a violation of their probation. The research indicates that cognitive behavioral therapy has been a successful approach in the rehabilitation of individuals suffering from TBI, as it makes them aware of their impairment and encourages them to learn once again how to deal with certain social situations and control their impulses. Therefore, counseling and treatment under the cognitive behavioral therapy umbrella is recommended under AHIT, as said treatment is evidence-based. Implementation Concerns and Summary During the implementation of the AHIT Protocol, this researcher anticipates Probation Departments considering the issues of funding, liability, and becoming involved in the medical treatment of possible injured juveniles that enter the criminal justice system. These are concerns that any manager would have in implementing any new rule, policy, or procedure. If a juvenile is confirmed to have suffered a TBI and needs a clinical interview or continued treatment, the question will be who funds the interview and treatment. However, the AHIT will be utilized with the detention risk assessment immediately upon the juvenile entering the detention center to determine whether the juvenile will be released or detained. If a clinical interview or medical clearance is needed, the juvenile will not be accepted into custody. The law enforcement officer will have to transport the juvenile to the hospital for clearance, or release the juvenile to the custody of his or her parents with a citation to appear in court. The 75 probation department will not have to worry about liability, as custody was never accepted. Often times, juveniles are arrested and transported to the detention facility for subsequent criminal offenses, and they are already on probation. If a juvenile is on informal or six months court probation, they were never removed from the custody of their parents, so their parents are responsible for the cost of the clinical interview and possible treatment. If the juvenile is already a Ward of the Court, which is formal probation, their parents can still be charged for the medical treatment, especially if the juvenile still resides in the home with his or her parents. The probation department will alert the parents to the need for the interview and possible treatment. If the juvenile is adjudicated for the offense, his or her case plan should include cognitive-behavioral counseling to address the TBI. The parents are responsible for the acquisition of counseling, as well as payment. If the juvenile was adjudged a Ward of the Court due to his or her parents being unavailable, and the juvenile needs a clinical interview or medical clearance due to a severe TBI, then the probation department will be responsible for funding. The juvenile was committed to the care and custody of the probation officer, and the probation department is responsible for maintaining the health and wellness of that juvenile. The parents can still be billed and held financially responsible for extra treatment rendered, just as they would be for any damage to the detention facility at the hands of the juvenile. The final concern is the thought of becoming involved in the medical status of the juvenile. The priority of the probation department at the time AHIT is utilized is to 76 merely determine if there is a need for clinical interview or medical clearance, and if so, to alert the parents and the court about possible consequences and behavioral changes that could exist with TBI. Ultimate treatment for TBI will fall on the parents, and the probation department does not have to approve of the treatment, unless the parental rights were removed. In this instance, the juvenile would be adjudged a Ward of the Court, and committed to the care and custody of the probation officer, so the probation department is obligated to provide medical care. 77 Chapter 5 Conclusion Traumatic brain injury, as stated in Chapters One and Two can cause cognitive impairments and severe behavioral changes, especially in youth, as they are involved in more activities that could cause injury. Injured individuals can become violent and disobedient due to the inability to control their anger and impulses, which poses liability issues for probation staff supervising these individuals while detained in the detention center or on probation in the community. Juveniles that have suffered severe TBI can pose major problems for probation staff, as their behavior can be unpredictable, bizarre, and uncontrollable. These individuals will need constant redirection, isolation, and restraint to complete simple directives, which could compromise the safety and security of the institution. These individuals can also flood the juvenile court system with constant violations of probation, as they do not have the capacity to follow the conditions of the court or directives of the probation officer with no knowledge of the consequences of their impairment or ability to control their behavior. Currently, probation departments may be unaware of TBI and the consequences of such injury, so juveniles suffering from possible injury might be labeled as persistent offenders and committed to detention and treatment facilities. Since their injury is never considered, they graduate to the adult system as juvenile delinquents or career criminals. The criminal justice system then continues to fail and becomes more overcrowded. However, if juveniles suffering from TBI cannot control their behavior, they could be considered victims of the criminal justice system, as no one attempted to uncover the real 78 reasons behind their actions. Also, the criminal behavior of these individuals continues to terrorize and victimize the community. Liability issues could arise with the continued victimization of society, as the public will want to know why was this juvenile not properly assessed or treated. The juveniles that suffer from TBI, along with their parents, may not know the severity of the injury or the future problems that can arise. The probation department could be the first agency to alert the parent to a severe medical condition and possibly save the life of a juvenile or innocent member of society. As stated in Chapter Two, some of the individuals that have suffered with head trauma have committed suicide due to the deterioration of brain functions, which leads to physical impairment, such as blindness, memory loss, inability to effectively communicate, and problems with walking. Chapter Two also discussed how some adult athletes that have suffered multiple concussions died sooner than others due to damage to the brain. TBI is an extremely serious issue that goes beyond compliance with probation and orders of the court. Detection and treatment of TBI could mean the difference between life and death. The Sacramento County Probation Department is now using many evidencedbased treatment interventions for juvenile crime. One such program is the Aggression Replacement Training (ART) program. ART is a multimodal intervention that was designed to reduce anger and violence among adolescents involved with the criminal justice system, and has recently been introduced to adults involved with said system (Sacramento County Probation Intranet Site (SCPIS), 2011). This program attempts to teach the offenders pro-social skills that will aid them in controlling their anger impulses 79 (SCPIS, 2011). However, if the Probation Officers, therapists, and offenders do not know that the offender’s lack of impulse control and aggression is due to their previous head injury, they may never be able to effectively use the skills the ART program teaches. This can also lead to false failures in the program and frustration on the part of the therapists (SCPIS, 2011). It may appear that the offenders are not taking the therapy serious and not exhibiting sufficient effort. This may also frustrate the offenders because they are exhibiting a great deal of effort, but it does not seem to work. It is suggested that probation departments continue the ART therapy program and others that aid offenders in dealing with impulse control and aggression, but add a question or two to their intake assessments to determine if the offender suffered a head injury at some point in their life where they were unconscious for 20 minutes or more. If an offender states they have suffered a head injury, then the offender should be referred to their physician for a MRI or CT scan to determine the severity of damage to the brain. Once this information is known, the therapist and probation officer should discuss the findings with the offender and his parent(s) to modify the offender’s case plan to include the proper treatment. This will help the offender, the offender’s family, and the legal system to fully understand the possible reasons for the criminal behavior and aggression exhibited by the offender, thus relieving the system of the burden of housing offenders that falsely appear to not respond to treatment or rehabilitation. Traumatic brain injury can change the course of one’s life and the lives of their families. The juvenile justice system consists of more than one victim. The juvenile, more often than not, suffers from a poor home life or emotional problems, which causes 80 him or her to victimize someone else. The families of the victim and the juvenile usually suffer as well. If more information was received and considered regarding TBI, the suffering could be minimized for all parties concerned. This researcher strongly recommends that probation departments throughout the United States utilize AHIT and abide by the AHIT protocol to properly and effectively assess juveniles in their care before their cases are resolved. The AHIT and AHIT protocol will only assist the probation officer in becoming the most successful change agent they can be and improve his or her ability to perform his or her duties, which is to protect the safety and security of the community, as well as the injured juvenile. 81 APPENDIX A Codification Key SUBJECT CODE MEANING Health Y Questions N Assessment specifically asks about health of juvenile Assessment does not ask about health Sports Y Assessment asks if juvenile plays or played Questions N Assessment does not ask about sports at all Abuse Y Questions N Assessment specifically asks if juvenile has ever been abused Assessment does not ask about abuse of the juvenile at all (HQ) (SQ) (AQ) Hospitalizations Y (HOSP) N Injury Y Questions N Assessment asks if the juvenile has spent more than one day in the hospital Assessment does not address hospitalization Assessment asks if juvenile has had serious injury Assessment only asks if juvenile is currently injured (IQ) Head Y Injury/TBI N (HI/TBI) Assessment asks if juvenile has or has ever had a serious injury to the head or suffered brain damage Assessment does not ask about injury to the head or brain at all 82 APPENDIX B Assessment Analysis ASSESSMENTS HQ SQ AQ HOSP IQ HI/TBI Y Y Y N N N YASI Y Y Y N N N PACT Y Y Y N N N DRAI 83 References Abel, D. (2010, April 28). Bill Addressing Student Concussions Advances. The Boston Globe. Retrieved from http://www.boston.com/news/education/k_12/articles/2010/ 04/28/bill_addressing_student_concussions_advances/ Antonucci, A. S., Gansler, D. A., Tan, S., Bhadelia, R., Patz, S., & Fulwiler, C. (2006). Orbitofrontal Correlates of Aggression and Impulsivity in Psychiatric Patients. Psychiatry Research: Neuroimaging, 147, 213-220. Assessments.com (2006). How to Read and Interpret the PACT Overview and the YES Case Plan Reports, 1-4. Baguley, I. J., Nott, M. T., & Howle, A. A. (2012). Late Mortality After Severe Traumatic Brain Injury in New South Wales: A Multicentre Study. Medical Journal of Australia, 196 (1), 40-45. Barnoski, R. (2013). PACT Full Assessment Positive Achievement Change Tool Full Assessment, Assessments.com, 1-5. Battista, J. (2012, December 15). ‘Train Wreck of a Play’ Collides With Consciences. The New York Times, p. SP1. Blake, P. Y., Pincus, J. H., & Buckner, C. (1995). ‘Neurologic Abnormalities in Murderers’. Neurology, 45, 1641-1647. Blumer, D., Benson, D. F., (1975). Personality Changes with Frontal and Temporal Lobe Lesions (Benson, D. F., & Blumer, D., Eds.). Psychiatric Aspects of Neurological Disease. New York: Grune and Stratton, 151-170. 84 Brooks, N. (1984). Closed Head Injury. Oxford: Oxford University Press. Brooks, N., Campsie, L., Symington, C., Beattie, A. & McKinlay, W. (1986). ‘The Fiveyear Outcome of Severe Blunt Head Injury: A Relative’s View’. Journal of Neurology, Neurosurgery and Psychiatry, 49, 764-770. Brower, M. C., & Price, B. H. (2001). ‘Neuropsychiatry of Frontal Lobe Dysfunction in Violent and Criminal Behaviour: A Critical Review’. Advances in Neuropsychiatry, 71, 720-726. Brumbaugh, S., Hardison-Walters, J. L., & Winterfield, L. A. (2010). Suitability of Assessment Instruments for Delinquent Girls. Girls Study Group Understanding and Responding to Girls’ Delinquency. Office of Juvenile Justice and Delinquency Prevention, 1-11. Bryant, R. A. (2001). Posttraumatic Stress Disorder and Traumatic Brain Injury: Can they Coexist? Clinical Psychology Review, 21, 931-948. Bryant, R. A., & Hopwood, S. (2006). Commentary on “Trauma to the Psyche and Soma.” Cognitive Behavioral Practice, 13(1), 17-23. Buchsbaum, M.S., Nuechterlein, K.H., & Haier, R.J. (1990). Glucose Metabolic Rate in Normals and Schizophrenics During the Continuous Performance Test Assessed by Positron Emission Tomography. British Journal of Psychiatry, 156, 216-227. 85 Carlson, K. F., Kehle, S. M., Meis, L. A., Greer, N. MacDonald, R., Rutks, I., Sayer, N. A., Dobscha, S. K., & Wilt, T. J. (2011). Prevalence, Assessment, and Treatment of Mild Traumatic Brain Injury and Posttraumatic Stress Disorder: A Systematic Review of the Evidence. Journal of Head Trauma Rehabilitation, 26(2), 103-115. Collins, M. W., Grindel, S. H., & Lovell, M. R.(1999). Relationship Between Concussion And Neuropsychological Performance in College Football Players. Journal of the American Medical Association, 282(10), 964-970. DePalma, R. G., Burris, D. G., Champion, H. R., & Hodgson, M. J. (2005). Blast Injuries. New England Journal of Medicine, 352(13), 1335-1342. Dinn, W., Gansler, D., Moczynski, N., and Fulwiler, C. (2009). Brain Dysfunction and Community Violence in Patients with Major Mental Illness. Criminal Justice and Behavior, 36(2), 117-136. Dooley, J., Anderson, V., Hemphill, S., & Ohan, J. (2008). Aggression after Paediatric Traumatic Brain Injury; A Theoretical Approach. Brain Injury, 22(11), 836-846. Farrington, D. P. (1982) Implications of Biological Findings for Criminological Research. National Institute of Justice. U.S. Department of Justice, 1-35. Flanagan, S. R. (2007). Pharmacological Treatment of Insomnia for Individuals with Brain Injury. Journal of Head Trauma Rehabilitation, 22(1), 67-70. Foa, E. B., Keane, T. M., Friedman, M. J., Cohen, J. A. (2008). Effective Treatments for PTSD, Practice Guidelines from the International Society for Traumatic Stress Studies. 2nd ed. New York, NY: Guilford Press. 86 Giancola, P. R. (1995). Evidence for Dorsolateral and Orbital Prefrontal Cortical Involvement in the Expression of Aggressive Behavior. Aggressive Behavior 21, 431-450. Gibbens, T. C. N., Pond, D. A., & Stafford-Clark, D. (1959). A Follow-up Study of Criminal Psychopaths. Journal of Mental Science, 105, 108-115. Grafman, J., Schwab, K., & Warden, D. (1996). Frontal Lobe Injuries, Violence and Aggression: A Report of the Vietnam Head Injury Study. Neurology, 46, 12311238. Haddad, S. H., & Arabi, Y. M. (2012). Critical Care Management of Severe Traumatic Brain Injury in Adults. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, 20, 12-26. Hall, K. M., Karzmark, P., Stevens, M., Englander, J., O’Hare, P. & Wright, J. (1994). Family Stressors in Traumatic Brain Injury: a Two-year Follow-up. Archives of Physical Medicine and Rehabilitation, 75, 876-884. Harrison-Felix, C., Whiteneck, G., DeVivo, M., Hammond, F. M., & Jha, A. (2004). Mortality Following Rehabilitation in the Traumatic Brain Injury Model Systems of Care. NeuroRehabilitation, 19(1), 45-54. Harrison-Felix, C., Kreider, S. E. D., Arango-Lasprilla, J. C., Brown, A. W., Dijkers, M. P., Hammond, F. M., . . . Zasler, N. D., (2012). Life Expectancy Following Rehabilitation: A NIDRR Traumatic Brain Injury Model Systems Study. Journal of Head Trauma Rehabilitation, 27(6), E69-E80. 87 Henry, B., & Moffitt, T.E., (1997). Neuropsychological and Neuroimaging Studies of Juvenile Delinquency and Adult Criminal Behavior. (Stoff DM, Breiling, J., Maser JD, Eds.). Handbook of Antisocial Behavior. New York: Wiley. Kolb, B., & Milner, B. (1981). Performance of Complex Arm and Facial Movements After Focal Brain Lesions. Neuropsychologia, 19, 505-514. Kreutzer, J. S., Wehman, P. H., Harris, J. A., Burns, C. T. & Young, H. F. (1991). ‘Substance Abuse and Crime Patterns among Persons with Traumatic Brain Injury referred for Supported Employment’. Brain Injury, 5, 177-187. Larson, E. B., & Zollman, F. S. (2010). The Effect of Sleep Medications on Cognitive Recovery from Traumatic Brain Injury. Journal of Head Trauma Rehabilitation, 25(1), 61-67. Leon-Carrion, J., and Ramos, F. (2002). Blows to the Head During Development Can Predispose to Violent Criminal Behaviour: Rehabilitation of Consequences of Head Injury is a Measure for Crime Prevention. Brain Injury, 17(3), 207-216. Levin, H. S., Amparo, E., Eisenberg, H. M., Williams, D. H., High, W. M. J., McArdle, C. B., & Weiner, R. L. (1987). Magnetic Resonance Imaging and Computerized Tomography in Relation the Neurobehavioral Sequelae of Mild and Moderate Head Injuries. Journal of Neurosurgery, 66, 706-713. Lewis, D. O., Pincus, J. H., Feldman, M., Jackson, L., & Bard, B. (1986). Psychiatric, Neurological, and Psychoeducational Characteristics of 15 Death Row Inmates in the United States. American Journal of Psychiatry, 143, 838-845. 88 Luiselli, J. K., Arons, M., Marchese, N., Potoczny-Gray, A., & Rossi, E. (2000). Incidence of Law-Violating Behavior in a Community Sample of Children and Adolescents with Traumatic Brain Injury. International Journal of Offender Therapy and Comparative Criminology, 44, 647-656. Martell, D. A. (1992). Estimating the Prevalence of Organic Brain Dysfunction in Maximum-security Forensic Psychiatric Patients. Journal of Forensic Sciences, 37, 878-893. Martland, H. S. (1928). Punch Drunk. Journal of the American Medical Association, 91, 1103-1107. Masson, F., Maurette, P., Salmi, L. R., Dartigues, J. J., Velsey, J., Destaillats, J.-M., & Erny, P. (1996) Prevalence of Impairments 5 Years after a Head Injury, and the Relationship with Disabilities and Outcome. Brain Injury, 10, 487-497. Matthes, J., & Caples, H. (2013). Ethical Issues in Using Deception to Facilitate Rehabilitation for a Patient with Severe Traumatic Brain Injury. Journal of Head Trauma Rehabilitation, 28(2), 126-130. McCrea, M. (2007). Mild Traumatic Brain Injury and Postconcussion Syndrome: The New Evidence Base for Diagnosis and Treatment. New York, NY: Oxford University Press. McCrea, M., Iverson, G. L., & McAllister, T. W. (2009). An Integrated Review of Recovery After Mild Traumatic Brain Injury (mTBI): Implications for Clinical Management. Clinical Neuropsychology, 23, 1368-1390. 89 McKee, A. C., Cantu, R. C., Nowinski, C. J., Hedley-Whyte, E. T., Gavett, B. E., Budson, A. E., . . .Stern, R. A. (2009). Chronic Traumatic Encephalopathy in Athletes: Progressive Tauopathy following Repetitive Head Injury. Journal of Neuropathology and Experimental Neurology, 68(7), 709-735. McMillan, T.M., Teasdale, G.M., Weir, C.J., & Stewart, E. (2011). Death after Head Injury: the 13 Year Outcome of a Case Control Study. Journal of Neurological Neurosurgery Psychiatry. 82(8), 931-935. Mednick, S. A., Moffett, T. E., & Stack, S. A. (Eds.). The Causes of Crime: New Biological Approaches. Cambridge: Cambridge University Press. Miller, E. (1999). Head Injury and Offending. The Journal of Forensic Psychiatry, 10(1), 157-166. Miller, K. J., Ivins, B. J., & Schwab, K. A. (2013). Self-reported Mild TBI and Postconcussive Symptoms in a Peacetime Active Duty Military Population: Effect of Multiple TBI History Versus Single Mild TBI. Journal of Head Trauma Rehabilitation, 28(1), 31-38. Miura, H., Fujiki, M., Shibata, A., & Ishikawa, K. (2005). Infuence of History of Head Trauma and Epilepsy on Delinquents in a Juvenile Classification Home. Psychiatry and Clinical Neurosciences, 59(6), 661-665. Moffitt, T.E. (1990). The Neuropsychology of Juvenile Delinquency: A Critical Review. (Tonry, M. and Morris, N., Eds.). Crime and Justice: A Review of Research Chicago: University of Chicago Press. 90 Nocera, J. (2012, December 14). Should Kids Play Football? The New York Times, p. A23. Olson, D., (2007). Florida Makes PACT with State’s Youthful Offenders. A Publication of the National Council of Juvenile and Family Court Judges. Juvenile and Family Justice Today, 1-6. Orbis Partners Incorporated. (2013). Solutions for the Helping Professions. YASI. Youth Assessment & Screening Instrument Brochure, 1-10. Perron, B., & Howard, M. (2008). Prevalence and Correlates of Traumatic Brain Injury Among Delinquent Youths. Criminal Behavior and Mental Health, 18, 243-255. Pilon, M., & Belson, K. (2013, January 10). Seau Suffered From Brain Disease. The New York Times, p. B13. Pine, D.S., Bruder, G.E., Wasserman, G.A., Miller, L.S., Musabegovic, A., & Watson, J.B. (1997). Verbal Dichotic Listening in Boys at Risk for Behavior Disorders. J American Academy Child Adolescent Psychiatry, 36, 1465-1473. Raine, A., (1993). The Psychopathology of Crime: Criminal behavior as a Clinical Disorder. San Diego: Academic. Raine, A., Buchsbaum, M.S., Stanley, J., Lottenberg, S., and Abel, L., Stoddard, J. (1994). Selective Reductions in Pre-frontal Glucose Metabolism in Murderers. Biological Psychology, 36, 365-373. Raine, A., Buchsbaum, M.S., & La Casse, L. (1997). Brain Abnormalities in Murderers Indicated by Positron Emission Tomography. Biological Psychiatry, 42, 495-508. 91 Raine, A., Park, S., Lencz, T., Bihrle, S., LaCasse, L., Widom, C. S., . . .Singh, M. (2001). Reduced Right Hemishphere Activation in Severely Abused Violent Offenders During a Working Memory Task: An fMRI Study, Aggressive Behavior, 27, 111-129. Richardson, J. T. E. (1990). Clinical and Neuropsychological Aspects of Closed Head Injury. London: Taylor & Francis. Ruff, R. (2005). Two Decades of Advances in Understanding of Mild Traumatic Brain Injury. Journal of Head Trauma Rehabilitation, 20, 5-18. Sacramento County Probation Department. (2012). Juvenile Intake Manual. Sacramento, CA. Sacramento County Probation Department. (2011). Evidence Based Practices. Sacramento County Intranet. http://saccounty.net. Sonnenberg, L., Dupuis, A., & Rumney, P. (2010). Pre-school traumatic Brain Injury and Its Impact on Social Development at 8 Years of Age. Brain Injury, 24 (7-8), 1003-1007. Stein, M. B., & McAllister, T. W. (2009). Exploring the Convergence of Posttraumatic Stress Disorder and Mild Traumatic Brain Injury. American Journal of Psychiatry, 166 (7), 768-776. Steinhart, D., (2006). Juvenile Detention Risk Assessment: A Practice Guide to Juvenile Detention Reform. Juvenile Detention Alternatives Initiative A Project of the Annie E. Casey Foundation, 1-101. 92 Sundin, J., Fear, N. T., Iversen, A., Rona, R. J., & Wessely, S. (2010). PTSD After Deployment to Iraq: Conflicting Rates, Conflicting Claims. Psychological Medicine, 40 (3), 367-382. Tarter, R.E., Hegedus, A.M., Winsten, N.E., & Alterman, A.I. (1985). Intellectual Profiles and Violent Behavior in Juvenile Delinquents. Journal of Psychology, 119, 125-128. Thaxton, L., & Patel, A. (2007). Sleep Disturbances: Epidemiology, Assessment, and Treatment. (Zasler, N. D., Katz, D. I., & Zafonte, R. D., Eds.). Brain Injury Medicine: Principles and Practice. New York, NY: Demos Medical Publishing, 557-576. Volavka, J. (1995). Neurobiology of Violence. Washington, D.C.: American Psychiatric Press. Volavka27, J. (1999). The Neurobiology of Violence: An Update. Journal of Neuropsychiatry and Clinical Neurosciences, 11, 307-314. Volkow, N.D., Tancredi, L.R., Grant, C., Gillespie, H., Valentine, A., Mullani, N., . . . Hollister, L. (1995). Brain Glucose Metabolism in Violent Psychiatric Patients: A Preliminary Study. Psychiatry Research Neuroimaging, 61, 243-253. Zeigler, T. (2012, February 1). Chronic Traumatic Encephalopathy (CTE). SportsMD Media, Inc. 93 Zollman, F. S., Larson, E. B., Wasek-Throm, L. K., Cyborski, C. M., & Bode, R. K. (2012). Acupuncture for Treatment of Insomnia in Patients with Traumatic Brain Injury: A Pilot Intervention Study. Journal of Head Trauma Rehabilitation, 27(2), 135-142.