Thompson-Epidemiology Final Paper
advertisement

1
Tuberculosis Screening
Tuberculosis Screening: The Interferon-gamma Release Assay (IGRA)
for Patients with Normal Immune Systems in Richmond, VA
Dr. Evelyn Davila
Applied Epidemiology
MPH 510
Mark Thompson
April 2013
2
Tuberculosis Screening
Background
Mycobacterium tuberculosis is the bacterium responsible for causing tuberculosis (TB) –
a disease which usually attacks the lungs (pulmonary infection) but can, in less common cases,
infect other organs (extrapulmonary infection) like the brain, kidneys, and lymph nodes (Centers
for Disease Control and Prevention, 2012). Furlow (2010) reports that one-third of the World’s
population is infected with the bacteria. Both pulmonary and extrapulmonary infections can be
fatal if not treated properly (CDC, 2012), and the emergence of drug-resistant strains makes the
need to follow treatment procedures properly more imperative than ever before. It is important to
note that tuberculosis infection does not always lead to disease. The bacterium can live in the
human body without causing any illness in a state of latent infection (CDC, 2012). Although
only 5 to 10% of infections lead to disease (Furlow, 2010), active tuberculosis is still one of the
leading bacterial killers among humans worldwide. In cases of active TB disease, patients
primarily present with chest pain, extended periods of coughing, and coughing up sputum or
blood, but may also show signs of weakness, appetite and weight loss, and fever (CDC, 2012). If
untreated, active TB infections progresses by slowly reducing functioning of vital organs
(Furlow, 2010).
Tuberculosis is spread through the air from person to person (CDC, 2012), and fomites
are not thought to play a role in the transmission of the disease. After seeing a worldwide
decline in disease prevalence after World War II, a resurgence occurred as the global AIDS
epidemic took hold in the 1980s (Furlow, 2010). Immune-compromised individuals are at the
greatest risk for developing active tuberculosis - this may include the aged or the young. For
Tuberculosis Screening
3
example, Jackson (1998) cites significant increases of cases in those 0-14 years of age from 1985
to 1991. HIV/AIDS, however, is the greatest risk factor for TB infections progressing into active
tuberculosis disease (Pawlowski, Jansson, Sköld, Rottenberg, Källenius, 2012). A compromised
immune system can complicate testing significantly, so the following sections outline and
discuss the two available TB screening tests and seek to shed light on the benefits of the blood
test over the skin test in patients with normal immune systems.
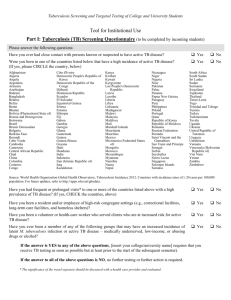
Tuberculosis Screening – Tuberculosis Skin Test
Tuberculosis screening involves testing that, if a positive result is found, indicates only
that a person has likely been infected with the M. tuberculosis bacteria; it cannot determine
whether the infection is latent or active (CDC, 2012). There are two types of screening tests –
the traditional skin test and the newer blood test (CDC, 2012). The Tuberculin Skin Test (TST),
also called the Mantoux tuberculin skin test, has traditionally been the gold standard in TB
screening (Selekman, 2006). This screening involves injecting a small amount of purified protein
derivative (PPD) under the forearm skin to create a wheal (Selekman, 2006). Within 48 to 72
hours, the person receiving the test must return to a facility where a trained healthcare employee
“reads” the results by looking for a reaction on the arm (CDC, 2012). Any raised or hardened
area (also called an induration) is measured with a ruler and considered positive (CDC, 2012;
Selekman, 2006). There are several short comings of this test including the need to sometimes
perform it twice to ensure correct results (avoid false positives) if a person has been vaccinated
(with the BCG vaccine) outside of the U.S. (Selekman, 2006; Furlow, 2010). Also, the
requirement for a patient to return to have the test read by a trained professional can prove
difficult in certain situations. A one-stop screening test would be preferable to these
requirements.
4
Tuberculosis Screening
Tuberculosis Screening - Interferon-gamma Release Assay
The more recent blood test, the Interferon-gamma Release Assay (IGRA), is a blood test
that measures the immune system’s response to the bacterium M. tuberculosis (CDC, 2012). It
detects the release of interferons from blood that has been incubated with proteins that are very
similar to M. Tuberculosis (Furlow, 2010). According to the Center for disease Control and
Prevention, there are currently only two FDA-approved versions of this type of assay for
screening in the United States; the QuantiFERON®–TB Gold In-Tube test (QFT-GIT), and the
T-SPOT®.TB test (T-Spot). The IGRA is more specific than the TST because it uses proteins
not associated with TB vaccinations like the BCG vaccine, leading to fewer false positive results
(Furlow, 2010.) Also, the convenience of not having to return to a health care professional for
results interpretation makes this method more convenient than the TST, even though the cost of
the IGRA can be 4 times higher (Baboolal, Ramoutar, & Akpaka, 2010).
Sensitivity and Specificity
The century-old tuberculosis skin test (TST) has been the standard for a century, but the
low sensitivity and specificity of the TST has led to misdiagnoses (Bocchino et al., 2010). In a
study of 31 Italians and 4 foreigners from high-prevalence countries enrolled for a year, the TST
was evaluated against the IGRA blood tests by T-Spot and QFT-GIT (Bocchino et al., 2010). In
this study, the T-Spot and QFT-GIT IGRA screening tests results are seen in Table 1 below.
Though the T-Spot screening performed slightly better than the QFT-GIT, the differences are
negligible in all areas but the negative predicted value (NPV). The researchers also showed that
the TST yielded positive results in <70% of cases while the IGRA tests were both above 80%
5
Tuberculosis Screening
(Bocchino et al., 2010). The results show that the IGRA screening has a higher sensitivity
(>80%) than
Table 1. IGRA Test Performance
Test
Sensitivity %
Specificity %
PPV %
NPV %
T-Spot
95
71
83
91
QFT-GIT
85
71
81
77
(Bocchino et al., 2010)
the TST (66%) and may be more useful in areas of low prevalence (Bocchino et al., 2010).
For 6 months in 2005, research conducted in Taiwan studied 65 patients -of which 39 had
active TB- to evaluate the effectiveness of the T-Spot IGRA test (Wang, Chou, & Lee, 2007).
Because the prevalence rate in Taiwan in 2003 was 62.38 per 100,000, the goal of this study was
to determine the viability of using an IGRA test in an area of high non-tuberculosis bacterial
disease (Wang, Chou, & Lee, 2007). The results are listed below in table II. It is interesting to
Table II. T-Spot Performance
Test
T-Spot
Sensitivity %
Specificity %
PPV %
NPV %
87.2
88.5
91.9
82.1
(Wang, Chou, & Lee, 2007)
note that all patients had been previously vaccinated with the BCG vaccine (Wang, Chou, & Lee,
2007). The results of this study show all 4 criteria in the table above to be >80% and the ability
of the assay to test rapidly significantly reduces the diagnosis time compared to a TST.
6
Tuberculosis Screening
Though the numbers in both of these studies were impressive, the authors in each
conceded that other reports had varying specificity, PPV, and NPV most likely due to different
selection and diagnosis criteria in those studies (Bocchino et al., 2010; Wang, Chou, & Lee,
2007). However, it does appear that the IGRA is an appropriate test for both high and low
prevalence areas.
Suitability and Ethics of IGRA Screening
The tuberculosis IGRA screening test can be used in the same settings in which the
antiquated TST is administered. However, the CDC recommends the IGRA over the TST in
settings where the patient has received the BCG vaccine (can yield false positives with the TST)
and in situations where patients may find it difficult to return to a trained professional to read the
skin test results (CDC, 2012). These two aspects of the IGRA along with its high sensitivity
make it a desirable tool for global healthcare, but worldwide access to this new technology may
be limited. The initial start-up costs of the test may further limit the numbers of patients or public
health professionals who can utilize it. As mentioned previously, the IGRA tests cost 4 times as
much as the TST (Baboolal, Ramoutar, & Akpaka, 2010). This can cause an ethical dilemma as
health care professionals seek the best available screening tests to be administered where they are
needed in a cost effective manner. Otherwise, there are no ethical concerns regarding the
invasiveness or patient risk of undergoing the IGRA testing
The IGRA’s high sensitivity, rapid detection, and logistical ease of reading results make
these blood tests preferable to the TST. Tuberculosis is a serious, potentially fatal disease, so the
high sensitivity of the IGRA means few true cases are likely to be missed in areas of both high
and low prevalence (as demonstrated in the aforementioned studies). The IGRA also produces
7
Tuberculosis Screening
fast results which are advantageous for identification and treatment of the disease. And the
ability of the IGRA to produce results without a follow up visit of patients to trained health care
professionals means cases will not go unreported (if patients fail to return). Ethically, financial
considerations again apply. Epidemiologists are responsible for advocating public health and
reporting results to assess the wellness of communities and community members. This is best
accomplished when the most effective and reliable techniques are used. In the case of a TB
screening test that costs four times more than the TST, access in developing communities and
poor populations may not be available.
Recommendations
The Virginia Department of Health (2013) reported the incidence of tuberculosis in the
Richmond City district to be 3.4 per 100,000 in 2012. This rate is about half of what it was in the
four preceding years in the same district and slightly higher than the total Virginia incidence rate
in 2012 (VHD, 2013). The Richmond district’s 2012 incidence rate mirrors that of the national
rate in 2011 (CDC, 2012), so the area is not affected by above-average cases. We are fortunate
here in the United States to reside in a country with a low prevalence and low risk of TB
infection. This means the traditional TST is a viable option for the population in Richmond,
Virginia. Since the BCG is rarer here in the states than other countries, the possibility of false
positives is relatively low. This being said, the IGRA is an all-around better method of screening,
so Richmond’s public health would benefit greatly from the use of the Interferon-gamma Release
Assay over the TST.
As stated previously, the technology used in this test has a higher sensitivity and
specificity than the TST by eliminating the possibility of questionable results in patients who
Tuberculosis Screening
8
have received the BCG vaccine. The logistical ease of use of the IGRA eliminates the need for
patients to return to a professional to have the results read which saves time. The benefits of this
screening extend to those taking immunosuppressant medications as well (Greveson, 2009). The
IGRA is undoubtedly the better technology available for TB screening and should be made more
available to all populations worldwide, not just patients in Richmond.
Participation
Increased use of the IGRA test will undoubtedly improve screening participation due to
the nature of its testing. Eliminating the need for a second visit to read the results means patients
only need to be present once for the screening. This will save time not only for the patients, but
also for the health care professionals involved with screening. Granted, the IGRA is more costly
than the TST, but the time savings and reduction of personnel requirements to confirm results
will make this a cost-effective technology. A study performed in San Francisco in 2004 reached
the same conclusion. The authors found that the time savings and cost savings from increased
patient evaluation rates and increased specificity over the TST makes the IGRA a cost effective
method for TB screening (Dewan et al., 2006). I would promote these benefits to health
departments and hospitals to improve participation by highlighting these very attractive
improvements over the TST.
It is the duty of health care professionals to provide the best care possible, and the IGRA is
the best option available. Minorities, especially African Americans, and immigrants are two
groups that bear the burden of TB in the United States (CDC, 2012). In the Richmond area,
which has a substantial immigrant and African American population, it is the responsibility of
the public health system to educate and promote testing participation among all communities to
9
Tuberculosis Screening
ensure the health of the district as a whole. It seems to me that aggressive promotion of the new
technology at health departments and health fairs should be a priority to help reduce the
incidence of TB even further. State funding to reduce start-up costs of implementing this new
technology would surely assist in reducing the cost for patients and increase access to the testing.
The Virginia Department of Health’s Tuberculosis (TB) Control and Prevention Program
mission is stated below.
“The mission of the TB Program is to control, prevent, and eventually eliminate
tuberculosis from the Commonwealth of Virginia. The Program aims to detect every case of
TB in Virginia, assure that every case is adequately and completely treated, and prevent
transmission of TB in communities.”
(VDH, 2013)
This goal can ultimately be accomplished by funding clinics and local health departments to
incorporate IGRA testing, and by educating communities and public health professionals of the
benefits of this new type of screening.
10
Tuberculosis Screening
REFERENCES
Baboolal, S., Ramoutar, D., & Akpaka, P. (2010). Comparison of the QuantiFERON®-TB Gold
assay and tuberculin skin test to detect latent tuberculosis infection among target groups
in Trinidad & Tobago. Pan American Journal Of Public Health, 28(1), 36-42.
Bocchino, M., Matarese, A., Bellofiore, B., Giacomelli, P., Russo, A., Signoriello, G., & ... San
Duzzi, A. (2010). Usefulness of IFN-gamma release assays in clinical management of
difficult TB cases: evidence from clinical practice. European Journal of Inflammation,
8(1), 43-47.
Center Disease Control and Prevention. (2012). Tuberculosis (TB). Retrieved from
http://www.cdc.gov/tb/
Dewan, P., Grinsdale, J., Liska, S., Wong, E., Fallstad, R., and Kawamura, L. (2006). Feasibility,
acceptability, and cost of tuberculosis testing by whole-blood interferon-gamma assay.
BMC Infectious Diseases, 6(1), 47-48.
Furlow, B. (2010). Tuberculosis: A review and update. Radiologic Technology, 82(1), 33-56.
Greveson, K. (2009). Can ELISpot replace the tuberculin skin test for latent tuberculosis?.
British Journal Of Nursing, 18(20), 1248-1254.
Tuberculosis Screening
11
Jackson, M. (1998). Tuberculosis in infants, children, and adolescents: an update with case
studies.. Pediatric Nursing, ({23}) 411(8).
Pawlowski, A., Jansson, M., Sköld, M., Rottenberg, M., Källenius, G. (2012). Tuberculosis and
HIV Co-Infection. Plos Genetics, 8(2), 1-7.
Selekman, J. (2006). Changes in the screening for tuberculosis in children. Pediatric Nursing,
(1), 73.
Wang, J., Chou, C., & Lee, L. (2007). Diagnosis of tuberculosis by an enzyme-linked
immunospot assay for interferon-γ. Emerging Infectious Diseases, 13(4), 553-558.
Virginia. Department of Health. (2013). TB Surveillance Reports: Virginia TB Statistics and
Reports - By Year, 2012. Retrieved from
http://www.vdh.state.va.us/epidemiology/DiseasePrevention/Programs/Tuberculosis/docu
ments/TBCR2012_final.pdf.