MSN I - Akal College Of Nursing
advertisement

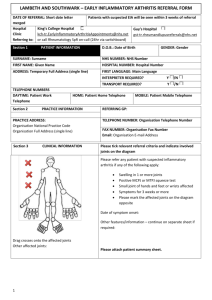
Summary Akal College of Nursing Medical Surgical Nursing-I Topic: Arthritis () Introduction ARTHRITIS is primary reason for work related disabilities and is leading cause of disability among people 65 years of age or older. There are over 100 forms of arthritis. Most common form is osteoarthritis. DEFINITION ARTHRITIS is an inflammation of joint characterized by pain , swelling and limitation of joint movement. TYPES Rheumatoid arthritis Osteoarthritis Spondyloarthropathies Gout arthritis Septic arthritis Still’s disease. GOUTY ARTHRITIS It is a disease in which purine metabolism is altered and the byproduct uric acid accumulates in the body evidenced by increased uric acid in blood stream. Uric acid form crystals which are deposited in connective tissue and trigger an inflammatory response. Cause - hereditary Symptoms- Join pain Swollen joints Redness. Gouty nephropathy Urinary calculi Treatment-Anti inflammatory drugs -Allopurinol and probenicid -Ample fluid to promote excretion of uric acid RHEUMATOID ARTHRITIS It is a chronic systemic progressive inflammatory disease affecting connective tissues of the body. It is characterized by inflammation in lining of synovial joints with severe involvement of joint structure. Affects women more than men. Etiology Cause is still unknown Autoimmunity Genetic predisposition- certain histo compatibility markers Agents- Mycoplasma Clostridium Epstein barr virus Parvovirus Clinical manifestations It is a systemic disease, however joints are generally affected first. Joints tend to be affected symmetrically. Wrist joint, PIP (proximal inter pharyngeal) and MCP( meta carpo phalangeal) joints are involved first. Joint swelling is more apparent in the morning. CRITERIA FOR DIAGNOSIS OF RA Morning stiffness lasting at least 1 hr. Swelling of three or more joints Swelling of wrist, PIP or MCP joints Symmetrical joint swelling Rheumatoid nodules Positive results on test for RF Changes on X ray typical for RF: A definitive requires that 4 of these seven features be present at the same time Articular manifestations- Synovitis -Muscle spasm and weakness -Hand deformity (ulnar drift, Boutonniere deformity, Swan neck deformity) -Rheumatoid nodules Extra articular manifestations- Skin changes - Pulmonary disease - Cardiac disease - Ocular symptoms - Neurological disease - Felty’s syndrome - Vasculitis Other symptoms Fatigue Weakness Low grade fever Anorexia Weight loss Generalized aching DIAGNOSTIC TEST Radiography Blood test- elevated ESR - elevated serum globulins - positive test for C reactive protein - anemia - RF( rheumatoid factor) positive with in 3 months after onset of symptoms - ANA( anti nuclear antibodies) positive Synovial fluid examination- arthrocentesis - Shows synovial fluid is cloudy, milky or dark yellow - Contains numerous inflammatory components - Reduced viscosity - WBC count is as high as 50,000/mm3 Medical management Early RA - NSAIDS (therapeutic doses) - Methotrexate (standard treatment for RA) - Analgesics - Balance of rest and exercise Non pharmacological measures- Relaxation techniques - Heat and cold application 2) Moderate erosive RAIn this stage occupational and physical therapy is prescribed to educate patient about - joint protection - pacing activities - work simplification - range of motion - muscle strengthening exercise Cyclosporin can be given 3) Persistent erosive RAcorticosteroids( local injection may be given) 4) Advanced RARequires high dose of methotrexate, cyclophosphamide, and azathioprine (DMARDS) Through all stages of RA low dose of antidepressants can be given Surgical management Synovectomy- excision of synovial membrane TENORRHAPHY- suturing of tendon Arthrodesis –surgical fusion of joints Arthroplasty- replacement of joints Nursing care PHYSICAL MOBILITY-Preserve joint function - Provide ROM to maintain joint motion and muscle strengthening - Balance rest and activity - Splints may be used during acute -inflammation to prevent deformity - Prevent flexion contractures - Apply heat and cold therapy -Apply paraffin baths and massage as prescribed. -Encourage consistency with exercise program -Instruct client to stop exercise if pain increases - Exercise only to the point of pain - Avoid weight on the inflammed joint - Assess need for assistive devices - Assess client’s reaction to the body change Osteoarthritis It is degenerative joint disease characterized by degeneration and loss of articular cartilage in synovial joint resulting in deterioration of underlying bone. Types Primary It occurs mainly in weight bearing areas with no prior event and is idiopathic. Secondary Resulting from previous injury or inflammatory disease. Etiology Joint injury- repetitive sprain and strain - joint dislocation - fracture - neurological disease. It may involve spine. Mostly occur in weight bearing joints of lower exremities Risk factors Increasing age Genetic predisposition Gender and hormonal factors Obesity and overweight Mechanical factors Congenital and developmental disorder of hips Previous inflammatory disease Clinical manifestations Pain--- Client experiences pain that diminishes after rest and intensify after activity early in disease - As the disease progresses, pain occurs even with slight motion or even at rest -Symptoms are aggravated by temperature change and climate humidity. -Joint Stiffness, swelling, crepitus, and limited ROM -Difficulty getting up after prolonged sitting. -Skeletal muscle disuse atrophy. Functional impairment Heberden’s node--These are hard or bony swellings that can develop in the DIP joints,they are caused by formation of osteophytes of articular cartilage in response to repeated trauma to the joints Osteophytes are also known as bone spurs are bony projections that form along the joints Bouchard’s node—osteophytes on PIP JOINTS Diagnostic test X ray On physical examination reveals tender and enlarged joints. Medical management Drug therapy- Aspirin - NSAIDS Relieve patient’s apprehension about disease and treatment Rest Good nutrition Maintenance of general health Physical therapy- Heat application - Weight reduction - Joint rest - Avoidance of joint overuse - Orthotic devices(splints , braces) - Isometric exercises - Aerobic exercises - Massage ,TENS - Musical therapy -Isometric exercises Surgical management Viscosupplementation( Hyaluronic acid injection ) Tidal irrigation Arthroscopic debridement With or without arthroscopic lavage. Arthroplasty Arthrotomy. Septic arthritis: Septic arthritis is invasion of synovial membrane by pathogens Causes- staphylococcus , - gonococcus - Meningococcus - streptococcus Mode of infection Organism can reach the synovium by one of following routes: Hematogenous Spread inoculation infection Previous trauma to joints, joint replacement, co existing arthritis, diminished host resistance also contribute. Risk factors Advanced age DM RA Pre existing joint disease Joint replacement Long term corticosteroids Pathophysiology Invasion of micro-organism into the joint Synovial membrane swells Become infiltrated with neutrophils Neutrophils release lysosomal enzymes Destroy articular cartilage, subchondral bone and joint capsule Septic arthritis Clinical manifestations Warm painful and swollen joint Decreased range of motion Fever,chills ,rapid pulse Leucocytosis Diagnostic test Aspiration, examination and culture of synovial fluid. CT and MRI. Radioisotope scanning – localizes infectious process Medical management Broad spectrum i/v antibiotics. Synovial fluid monitored for sterility and decrease in WBC. Aspiration of synovial fluid may be done to remove excessive joint fluid , exudate and debris Support by splint. Analgesics NSAIDS Good nutrition and fluid status Progressive range of motion Spondyloarthropathies: It is the another category of systemic inflammatory disorder of skeleton system. It includes: Ankylosing sponylitis Reactive arthritis or Rieter’s syndrome Psoriatic arthritis. Ankylosing spondilitisI: t is a chronic progressive inflammatory disease of the spine and sacro-iliac joint which leads to extensive bony ankylosis or scaring within the joint. It affects men more than women. Begins in adolescence or early adulthood. Results in poker like spine. Common symptoms are pain and stiffness in the back. Treatment- anti inflammatory drugs. Reactive arthritis The disease process is called reactive because arthritis occurs after the infection. It mostly affects the young adult males and is characterized primarily by urethritis, arthritis and conjunctivitis. Dermatitis, and ulceration of the mouth & penis may also be present. Low back pain is common. Psoriatic arthritis It is characterized by synovitis, polyarthritis and spondilytis. The prevalence of arthritis in patient with psoriasis is 15-25%. Prevalence of psoriasis in patient with arthritis is 2.6 – 7%. Medical management Focus is on treating pain and suppressing inflammation and maintains mobility. Maintain ROM with regular exercises. NSAIDS & corticosteroids are helpful. Methotrexate may help with peripheral disease. Surgical management includes total joint replacement. Still’s disease It may refer to: Juvenile idiopathic arthritis Adult onset still’s disease. AOSD is systemic inflammatory disease characterized by triad of fever, joint pain and rash. Serum ferritin is elevated. , RF & ANA are negative. Treatment: steroids e.g. prednisolone Juvenile arthritis have onset before 16 years Limping and flu like symptoms are common manifestations. Persistent swelling of affected joints. Pain with morning stiffness. Submitted by: Komal Rana CI ACN