CHRONIC PAIN: Philosophy and Process
advertisement
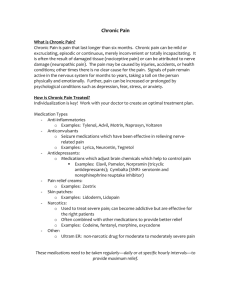
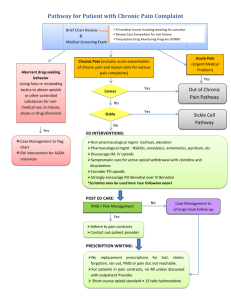
Hill Country Health and Wellness Center THE TREATMENT OF CHRONIC PAIN: Philosophy and Process F inding helpful treatment for chronic pain is one of the biggest issues for many patients coming to Hill Country. We know that many people feel stuck in a system that has only offered medication, or frustrated that medications haven’t really helped. For many patients, depression and anxiety have become mixed in with the physical pain. We believe that chronic pain treatment should include a wide range of both non-medication and medication options. We can provide you with an entire care team dedicated to improving your emotional, mental, AND physical health while managing your chronic pain. OUR PROCESS At your first office visit, your primary care provider will get your history, do a physical exam, and will want to hear what you have already tried, to manage your pain. However, she will not refill or prescribe any pain medications until we have received all relevant records of your previous treatment and prescription history. We want you to know that it may take from one to six months to receive the health information we need to prescribe your pain medications. Your second appointment will be for a chronic pain risk and safety assessment, with one of our behavioral health consultants (BHC). The BHC will ask how your chronic pain has affected your emotional and mental health and help your primary care provider evaluate your health risks. They will discuss options for ways to manage your pain without medication, especially if you may need to be without medications while we receive your records. They will help you identify goals you may have for dealing with daily activities. This appointment can usually happen within a few days, and then the BHC will then work with you and your care team to create a safe, individualized care plan. If you like, we encourage your family’s involvement. For many patients, the chance to work with a BHC is just the opportunity they’ve been looking for, to get some help to “take back my life!” A list of many non-medication options that may help is on the back of this page. When we have all the information we need about your medication and treatment history, your primary care provider will meet with you to plan the use of medications (if needed). We start with the options that provide the lowest risk for side-effects and/or addiction. We follow all DEA guidelines, and we may also have to work within limits of what is covered by your insurance plan. We will be strong advocates for getting the best care options for you. Please keep in mind that the abuse of pain medication is a public health problem that we take seriously. Our policies, and the controlled substances agreement that you may be asked to sign, are not intended to cast suspicion on any of our patients, but have been developed to reduce the risk of prescription medication abuse and addiction in our communities. YOUR RESPONSIBILITIES AS A HILL COUNTRY PATIENT Be honest with us at all times about what you are doing to address your chronic pain. Follow the terms of the agreement signed by you and your provider Stay open to trying new options! Tell us what’s working, and what’s not. Rev. 4/9/2014 OPTIONS FOR REDUCING AND MANAGING CHRONIC PAIN NON-MEDICATION OPTIONS 1) Specific physical exercise, physical therapy Examples: stretching, massage, hydrotherapy, strength training, heat/ice, ultrasound, muscle stimulation, etc. 2) Temporary restricted movement or physical support Examples: rest, reduced activity, splints, compression socks/gloves/sleeves/belts, braces, etc. 3) Specific dietary changes to reduce inflammation or promote healing/weight loss 4) Mind-body integration practices Examples: yoga, meditation, tai chi, Healing Touch, Reiki, prayer, religious/spiritual activity, Feldenkrais Method, rolfing, Trager Approach Movement Therapy 5) Neuro/biofeedback 6) TENS (Transcutaneous Electrical Nerve Stimulation) 7) Acupuncture/acupressure 8) Chiropractic 9) Osteopathic manipulation 10) Over the counter topical treatment Examples: Creams and ointments such as Traumeel, Capsaicin, Menthol. 11) Other “Complementary and Alternative Medicine” (CAM): Examples: Nutritional supplements Herbal supplements or teas/compresses Homeopathy 12) Support groups, classes, self-help resources 13) Counseling/Psychotherapy Examples: Cognitive Behavioral Therapy, stress management, relaxation therapy, Acceptance & Commitment Therapy, behavior modification, hypnotherapy 14) Online resources and self-management apps Rev. 4/9/2014 MEDICATION OPTIONS 1) Non-opioid pain relievers (lower risk) May be over the counter or prescribed Examples: acetaminophen, aspirin, ibuprofen, other non-steroidal antiinflammatory drugs (NSAIDS) 2) Short-term opioid pain relievers (higher risk) Must be prescribed Examples: Codeine, hydrocodone, vicodin, norco, tramadol, etc. 3) Long-term opioid pain relievers (higher risk) Must be prescribed Examples: morphine, hydromorphone, fentanyl, methadone, etc. 4) Muscle relaxants Must be prescribed Examples: flexaril, baclofen, dantrolene 5) Injectable steroids, local anesthetics Requires medical visit to administer Examples: toradol, prednisone, kenalog, lidocaine 6) Antidepressants Must be prescribed Counseling/psychotherapy recommended Examples: SSRIs (Zoloft, Lexapro, Prozac), SNRIs (Cymbalta), Tricyclics 7) Anticonvulsants Must be prescribed Examples: gabapentin, pregabalin, lamitrogene 8) OTHER: Surgical and neurosurgical procedures Require referral to specialty care Examples: spinal cord stimulation, deep brain stimulation, spinal delivery of opioids, ganglion ablation by phenol or electrofrequency, sympathectomy