Renal Case Study - Dawn Ortiz`s Portfolio
advertisement
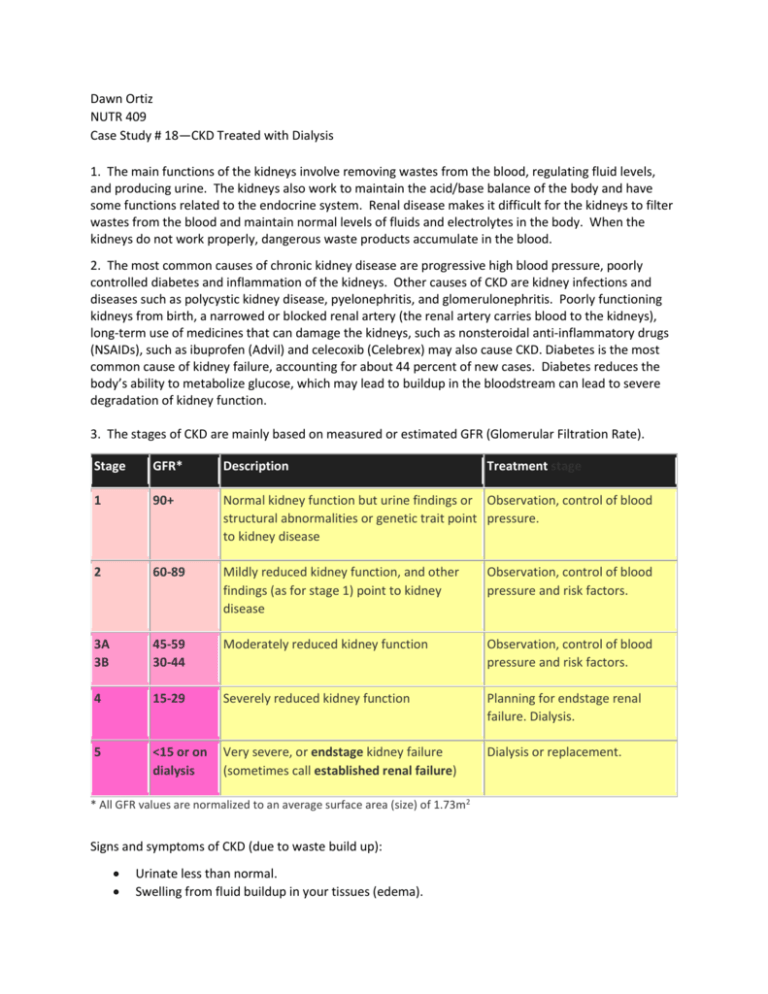
Dawn Ortiz NUTR 409 Case Study # 18—CKD Treated with Dialysis 1. The main functions of the kidneys involve removing wastes from the blood, regulating fluid levels, and producing urine. The kidneys also work to maintain the acid/base balance of the body and have some functions related to the endocrine system. Renal disease makes it difficult for the kidneys to filter wastes from the blood and maintain normal levels of fluids and electrolytes in the body. When the kidneys do not work properly, dangerous waste products accumulate in the blood. 2. The most common causes of chronic kidney disease are progressive high blood pressure, poorly controlled diabetes and inflammation of the kidneys. Other causes of CKD are kidney infections and diseases such as polycystic kidney disease, pyelonephritis, and glomerulonephritis. Poorly functioning kidneys from birth, a narrowed or blocked renal artery (the renal artery carries blood to the kidneys), long-term use of medicines that can damage the kidneys, such as nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil) and celecoxib (Celebrex) may also cause CKD. Diabetes is the most common cause of kidney failure, accounting for about 44 percent of new cases. Diabetes reduces the body’s ability to metabolize glucose, which may lead to buildup in the bloodstream can lead to severe degradation of kidney function. 3. The stages of CKD are mainly based on measured or estimated GFR (Glomerular Filtration Rate). Stage GFR* Description 1 90+ Normal kidney function but urine findings or Observation, control of blood structural abnormalities or genetic trait point pressure. to kidney disease 2 60-89 Mildly reduced kidney function, and other findings (as for stage 1) point to kidney disease Observation, control of blood pressure and risk factors. 3A 3B 45-59 30-44 Moderately reduced kidney function Observation, control of blood pressure and risk factors. 4 15-29 Severely reduced kidney function Planning for endstage renal failure. Dialysis. 5 <15 or on dialysis Very severe, or endstage kidney failure (sometimes call established renal failure) Dialysis or replacement. * All GFR values are normalized to an average surface area (size) of 1.73m2 Signs and symptoms of CKD (due to waste build up): Urinate less than normal. Swelling from fluid buildup in your tissues (edema). Treatment stage Fatigue. Not feel hungry, or you may lose weight without trying. Often feel sick to your stomach (nauseated) or vomit. Trouble sleeping. Headaches or trouble thinking clearly 5. Treatment for Stage 5 CKD: 1) Peritoneal dialysis (APD, CAPD)- Treatment that can usually be carried by you in your own home or at work. Waste products are removed across the natural membrane which lines the inside of the abdomen. This lining is called the peritoneum. The membrane is bathed in a special fluid passed into the abdomen through a small plastic tube. After a few hours this fluid is drained away and replaced by new fluid. APD, (Automated Peritoneal Dialysis) involves the use of a small simple machine, usually attached for approximately 8-9 hours at night. A small amount of involvement is required during the day. CAPD (Continuous Ambulatory Peritoneal Dialysis) involves carrying out 4 fluid exchanges daily. They are usually 4-6 hours apart with a longer gap overnight. The time taken is usually 30-40 minutes and can be timed to fit in with your daily activities. 2) Hemodialysis- Uses machines and takes three half days of every week, usually at a dialysis center. During hemodialysis the blood is treated by passing it through an artificial kidney. 3) Kidney transplant 6. NUTR Therapy 35 kcal/kg 1.2 g PRO/kg 2g K 1g phosphorus 2 g Na 1000 mL fluid + urine output Rationale Weight gain High PRO for stressed state Low K—to avoid over working the kideneys Low phos—“” Low sodium intake—“” Low fluid intake—“” 7. BMI= 33, high BMI attributed to 4 kg wt gain in 2 week from fluid retention, AEB edema. 8. Edema-free weight: 12. Protein needs are higher in people undergoing dialysis. ◾Hemodialysis patients can lose 10-12 grams of amino acids, the building blocks of protein, per treatment. ◾PD patients may lose 5-15 grams of protein per treatment. ◾Infection, inflammation, sores, anemia, some thyroid issues, metabolic acidosis (common with diabetes) and other medical conditions call for a higher protein intake. ◾People who perform daily treatment are able to consume more protein in their diet. 13. Mrs. Joaquin’s phosphorus restriction is due to the fact that excess phosphorus is excreted by healthy kidneys, but when the kidneys fail, phosphorus builds up in the blood, which can cause severe bone and heart problems, tissue calcification and itching. Phosphorus is found in dark colas, milk, cheese, processed meats, fish, poultry, chocolate, whole grains and nuts. For patients with CKD, the recommended amount is 800-1,000 mg per day. Most dialysis patients take phosphate binders with their meals. These medications bind up the phosphorus so it can be excreted in the stool instead of being absorbed. 14. Under a fluid restricted diet, fluid-based foods are also counted as fluids, such as soup, ice pops, gelatin, gravy, watery fruits and ice. To reduce thirst and alleviate dry mouth, she can eat a diet low in sodium, chew on ice chips, suck on sugar-free hard candy and chew gum. 15. Glomerular filtration rate (GFR) is a test used to check how well the kidneys are working. Specifically, it estimates how much blood passes through the tiny filters in the kidneys, called glomeruli, each minute. Normal results range from 90 - 120 mL/min/1.73 m2. Levels below 60 mL/min indicate CKD and levels under 15 mL/min indicate renal failure. Mrs. Joaquin’s GFR is 28 mL/min indicating CKD, but not yet renal failure. Based on her GFR she is in the beginning of stage 4 CKD. 16. Labs supporting Stage 5 CKD are her negative fluid balance, low sodium, high potassium, extremely high BUN (69 mg/dL), extremely high creatinine (12 mg/dL), and extremely high phosphate (9.5 mg/dL). 18. Med Capoten/captropril Erythropoietin Sodium bicarbonate Renal caps Renvela Hectorol Glucophage Indications/Mechanism HTN Controls RBC production antacid Water soluble vitamins Phosphate binder Treatment of secondary hyperparathyroidism in patients with chronic kidney disease on dialysis Type 2 diabetes NUTR concern Take 1 hour before meals Increase iron intake Avoid vitamin and mineral supplements Avoid folic acid Avoid Ca and mineral supps Multi-vitamin, Ca and phosphorus Avoid alcohol 19. One half of adult Pima Indians have Type 2 Diabetes resulting from being over-weight and obese. These people may have developed a thrifty gene that allowed them to store fat during times of plenty so that they would not starve during times of famine. This gene was helpful as long as there were periods of famine. But once these populations adopted the typical Western lifestyle, with less physical activity, a high fat diet, and access to a constant supply of calories, this gene began to work against them, continuing to store calories in preparation for famine. Scientists think that the thrifty gene that once protected people from starvation might also contribute to their retaining unhealthy amounts of fat. 22. At least 50% of the protein ingested should be of high biological value. Protein of high biological value has an amino acid composition that is similar to human protein, is likely to be an animal protein, and tends to be utilized more efficiently by humans to conserve body proteins. The increased efficiency of utilization of high biological value protein is particularly likely to be observed in individuals with low protein intakes.